Recently Diagnosed or Relapsed? Stop Looking For a Miracle Cure, and Use Evidence-Based Therapies To Enhance Your Treatment and Prolong Your Remission
Multiple Myeloma an incurable disease, but I have spent the last 25 years in remission using a blend of conventional oncology and evidence-based nutrition, supplementation, and lifestyle therapies from peer-reviewed studies that your oncologist probably hasn't told you about.
Click the orange button to the right to learn more about what you can start doing today.
- You are here:
- Home »
- Blog »
- Multiple Myeloma »
- Non-Secretory Multiple Myeloma
Non-Secretory Multiple Myeloma
“…truly non-secretory myeloma to less than 3% of all newly diagnosed myeloma patients. With regard to prognosis, it appears from most series that patients with non-secretory myeloma have a prognosis similar to or better than that of patients with secretory myeloma..”
Hi David- I am wondering about monitoring my MM. I am non secretory. I had a BMB to confirm this then underwent chemo for a short period, could not tolerate well. Then off for an autologous stem cell transplant (ASCT).
That was over one year ago and I have been cruising along quite well since. I am being monitored by my free light chain blood work.
I am grateful no more BMB but I am concerned as the original diagnosis was stage 1, only because I didn’t have the normal markers in my blood work that the criteria said I should have (missing because I am non secretory).
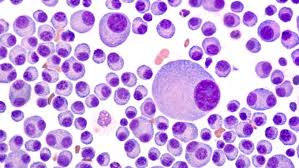
I have a hemotologist who has never worked with non secretory so I wonder now if his diagnosis of stage 1 was correct. My malignant cells in the original BMB were 80-90%. I fractured over 9 vertebrae and multiple ribs and one shoulder prior to treatment.
I’m going to sign up for your course. Any info you can shed on the non secretory would be appreciated. My dad passed away from MM a few years ago so I believe there must be a genetic link. I am now 62 years old.
Recommended Reading-
- Multiple Myeloma Response – MRD, sCR, CR, VGPR, PR ???
- Multiple Myeloma Diagnosis- Can’t Trust Conventional Cancer Research
- Relapsed/Refractory Multiple Myeloma- Patient Preferences
Non-Secretory Myeloma: A Clinician’s Guide
Inherited predisposition to multiple myeloma
“Conclusion and future directions-
Several lines of evidence point to a genetic predisposition to MM and other plasma cell dyscrasias. Until recent years, only case-control studies and reports of occasional high risk families supported this view.
More recently, identification of hyperphosphorylated paratarg proteins and identification of putative susceptibility loci by GWASs have provided more firm evidence indicating inherited predisposition to MM and related disorders. The discovery of pP-7 as a frequent target of paraproteins in MM offers a potential link between the old concept of chronic antigenic stimulation as a potential cause of MM, and observations of familial predisposition as well as racial disparities in the incidence of MM.
GWASs have to date identified several susceptibility potential regions of interest in MM and further molecular studies aimed at identification of specific genes of interest are ongoing. Although these discoveries are provocative, further work will be required to identify the genes and mechanisms underlying inherited susceptibility to MM, and these studies will be facilitated by the use of additional resources such as family registries and large-scale consortia.”