
Diagnosed with Cancer? Your two greatest challenges are understanding cancer and understanding possible side effects from chemo and radiation. Knowledge is Power!
Learn about conventional, complementary, and integrative therapies.
Dealing with treatment side effects? Learn about evidence-based therapies to alleviate your symptoms.
Click the orange button to the right to learn more.
- You are here:
- Home »
- Blog »
- side effects ID and prevention »
- Prostate Cancer…Seriously Uncomfortable Cystoscopy…
Prostate Cancer…Seriously Uncomfortable Cystoscopy…
“It’s also because the results from the prostate-specific antigen (PSA) test, which can be part of the screening, may lead to a misdiagnosis of prostate cancer…”
I needed to find a new primary care physician, the insurance company decided to quit doing business with my longstanding doctor. So, I meet this doctor for the first time. They decide after reading my questionnaire that I am in need of many tests to evaluate possible prostate cancer (PCa).
Because i had noted my pissing issues, that I should get a PSA test (prostate specific antigen) After the remainder of the examination, I went across the hall to the blood lab and took the test.
A month later, upon returning to the doctor, she informs me that i have a PSA of 5.45, and that this number is too high. There is no explanation of what this means, just that it may indicate the presence of cancer She states that I need to make an appointment with a urologist.
A few weeks later, I meet my new doctor, the urologist. The doctor proceeds to take note of the fact that my father had prostate cancer and was treated twice. The doctor tells me I am in need of further tests. A month goes by and 2 CAT scans and 2 MRI’s later, the CAT scans and the MRI’s indicate there is nothing wrong. Undeterred, my urologist schedules a cystoscopy and a biopsy, another month away.
The day of these tests, I endure the humiliation and seriously uncomfortable cystoscopy. The nurse injects lubricant into my penis and then pushes the probe into me and into my bladder. I’m asked if I want to view the monitor; I have no interest in viewing the monitor, I just want to get this thing out of my penis and bladder. The women in the room make fun of my wimpish response to being naked, spread eagled in stirrups; “Imagine doing this at least once a year in the gynecologists office.” After the probe is removed, I am informed by the nurse that the last guy smacked her as she shoved the probe in. I feel somewhat vindicated regarding my whimpishness.
Michael Thompson
- Prostate Cancer Survivor
- Board Member- PeopleBeatingCancer
Recommended Reading:
Everything You Want to Know About Prostate Cancer
“What’s prostate cancer?
Prostate cancer is a serious disease that affects thousands of men each year who are middle-aged or older. About 60 percent of the cases occur in men older than age 65. The American Cancer Society (ACS) estimates that 174,650 American men will be newly diagnosed with this condition in 2019.
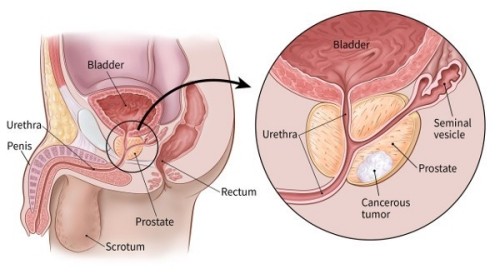
The prostate is a small gland found in a man’s lower abdomen. It’s located under the bladder and surrounding the urethra. The prostate is regulated by the hormone testosterone and produces seminal fluid, also known as semen. Semen is the substance containing sperm that exits the urethra during ejaculation…
Most cases of prostate cancer are a type of cancer called an adenocarcinoma. This is a cancer that grows in the tissue of a gland, such as the prostate gland.
Prostate cancer is also categorized by how fast it grows. It has two types of growths:
- aggressive, or fast growing
- nonaggressive, or slow growing
With nonaggressive prostate cancer, the tumor either doesn’t grow or grows very little over time. With aggressive PCa, the tumor can grow quickly and may spread to other areas of the body, such as the bones.
There’s no known cause for PCa. Like all cancers, it could be caused by many things, including a family history or exposure to certain chemicals…
Your doctor will likely use both the results from your PSA test and your Gleason score to help determine the stage of your PCa. The stage indicates how advanced your cancer is. This information helps your doctor plan your treatment.
Another tool used in staging PCa is the American Joint Committee on Cancer (AJCC) TMN staging system. Like many other types of cancer, prostate cancer is staged using this system based on:
- the size or extent of the tumor
- the number of lymph nodes involved
- whether or not the cancer has spread (metastasized) to other sites or organs
PCa stages range from 1 to 4. The disease is most advanced in stage 4. Learn more about prostate cancer staging, and what each stage means…
Screening for prostate cancer often depends upon your own personal preferences. This is largely because most prostate cancers grow slowly and don’t cause any health problems, according to the Centers for Disease Control and Prevention (CDC)Trusted Source.
It’s also because the results from the prostate-specific antigen (PSA) test, which can be part of the screening, may lead to a misdiagnosis of cancer. For both of these reasons, screening could cause unnecessary worry and unneeded treatment.
Screening recommendations
The ACS does have screening recommendations for men as they get older. They recommend that during an annual exam, doctors talk to men of certain ages about the pros and cons of screening for PCa. These conversations are recommended for the following ages:
- Age 40: For men at very high risk, such as those with more than one first-degree relative — a father, brother, or son — who had prostate cancer at an age younger than 65.
- Age 45: For men at high risk, such as African American men and men with a first-degree relative diagnosed at an age younger than 65.
- Age 50: For men at average risk of prostate cancer, and who are expected to live at least 10 more years.
The U.S. Preventive Services Task Force (USPSTF) now recommends that men aged 55 to 69 decide for themselves whether to undergo a prostate-specific antigen (PSA) test, after talking it over with their doctor.
The USPSTF concludes that the potential benefits of PSA-based screening for men aged 70 and above does not outweigh the expected harms.


