Leave a Comment:
9 comments
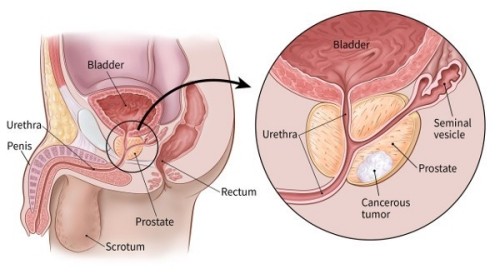
[…] To Learn More about Low-Risk Prostate Cancer- click now […]
ReplyPSA 18.1
MRI controlled
BIOPSY with 9 CORES (ADENOCARCINOMA),
Gleason 3+3=6/10
Group 1.
Active survalence 7 years.
At VA offering surgical removal; radiation SBRT and EBRT.
Overwhelmed with this prostrate cancer journey.
NEVER POSTED ANYTHING SO HOW COULD THERE BE A DUPLICATE SAID ANYTHING?
PSA 18.1
MRI controlled
BIOPSY with 9 CORES (ADENOCARCINOMA),
Gleason 3+3=6/10
Group 1.
Active survalence 7 years.
At VA offering surgical removal; radiation SBRT and EBRT.
Overwhelmed with this prostrate cancer journey.
PSA 18.1
MRI controlled
BIOPSY with 9 CORES (ADENOCARCINOMA),
Gleason 3+3=6/10
Group 1.
Active survalence 7 years.
At VA offering surgical removal; radiation SBRT and EBRT.
Overwhelmed with this prostrate cancer journey.
Want info on nutrition, supplements (Taking Prosta Genix), lifestyle.
Hello David – I will try and be brief.
jan, 2015: first ever PSA test @ age 52 – PSA of 6
July, 2015: 2nd test: PSA score of 8
Oct, 2015: biopsy, gleason 3/3 in 8 of 12 cores, high of 30%
Doctors recommend the “gold standard” (their words) of prostatectomy.
I have gone cold turkey and stopped coffee, sugar, meat, oils, and dairy. Basically a McDougall diet. then I read about Budwig, and for the last 7 days I have been taking FO/CC mixture twice a day – not very McDougall-ish. I also started exercising and have lost 12 pounds.
What are your thought on all of this? I told the doctors in October I will make a decision in Jan. or Feb.
I have no symtoms and overall I feel great. I still can’t believe I actually have cancer.
ReplyHi John-
I am sorry to read of your prostate cancer diagnosis. I have to say however, that you are doing a great job of pursuing lifestyle therapies that may already be lowering your PSA.
To answer your questions:
1) If you are interested I will link evidence-based research citing the citotoxic properties of antioxidant supplements such as curcumin, green tea extract, etc. This form of therapy is a good idea regardless of what additional therapies you choose at a later date.
2) A prostatectomy can and usually does lead to serious collateral damage such as incontinence and erectile disfunction. I will link info that calls into question the need for this aggressive therapy for your stage.
3) If, after reading the HIFU info linked below you are interested in learning more about that therapy I can do further research for you- studies, specialists, that kind of thing.
Please read the study conducted by Dr. Dean Ornish regarding gene expression of men diagnosed with low grade prostate cancer (you).
Prostate Cancer Genes Altered By Intensive Diet And Lifestyle Changes
This is the HIFU info-
High-intensity focused ultrasound (HIFU) for prostate cancer- low side-effect curative approach ?
John- after reading the above you may still decide to have a prostatectomy. This is up to you. My goal is to provide a spectrum of information for you so that you can have choices.
This is a link to Gleason info that relates to you-
Let me know if you have questions about the above info.
thanks
David Emerson
ReplyMy dad has a PSA >1500? is there still chance to be treat? He is 69 and was very healthy before… feeling sick for about 4 month…
ReplyHi Jian-
A very high PSA can be misleading. Please read the link below. Please consider having another psa test done as well as a biopsy. Please have a biopsy, get more information and we can discuss your/your dad’s treatment options. Contact me again and I can recommend both conventional and non-conventional therapies. Hang in there. David Emerson
How High Can the PSA Go?
“It is possible for the PSA to go to very high levels. There is no absolute maximum value. In fact, I have seen PSA values over 2000 ng/mL. As a rule of thumb, the higher the serum PSA, the more extensive the tumor, but this is not an absolute rule or a direct relationship. It varies from individual to individual. For example, a man with a PSA of 40 ng/mL does not have twice as much tumor as a man with a PSA of 20 ng/mL. It IS generally true, however, that a man’s PSA will go from 20 to 40 when the tumor roughly doubles in size. Each person’s tumor makes and leaks PSA at its own rate. Similarly, I have patients with PSAs over 300, yet who are alive without tumor 10 years after receiving radiation and hormones. Having said that, a smaller fraction of that group is alive than out of the group of men with PSAs of 10….” read more…