Does your testosterone/urinary function before a radical prostatectomy (complete prostate removal) for prostate cancer influence your chances of urinary continence and/or erectile dysfunction after a radical prostatectomy?
You have been diagnosed with prostate cancer. You are considering your therapy plan- radiation, ADT, prostatectomy…what questions should you ask your oncologist? What are your priorities?

I am both a cancer survivor and cancer coach. My role is not to be for or against and therapy, my role is to try to present all sides of a given therapy whether it is conventional (FDA approved) or evidence-based non-conventional.
Further, experience and research have taught me that there are dozens of evidence-based therapies that your conventional oncologist may not mention. Pre-habilitation, for instance, has been shown to enhance the cancer patients ability to undergo therapies.
What are some side effects from prostatectomy for prostate cancer?
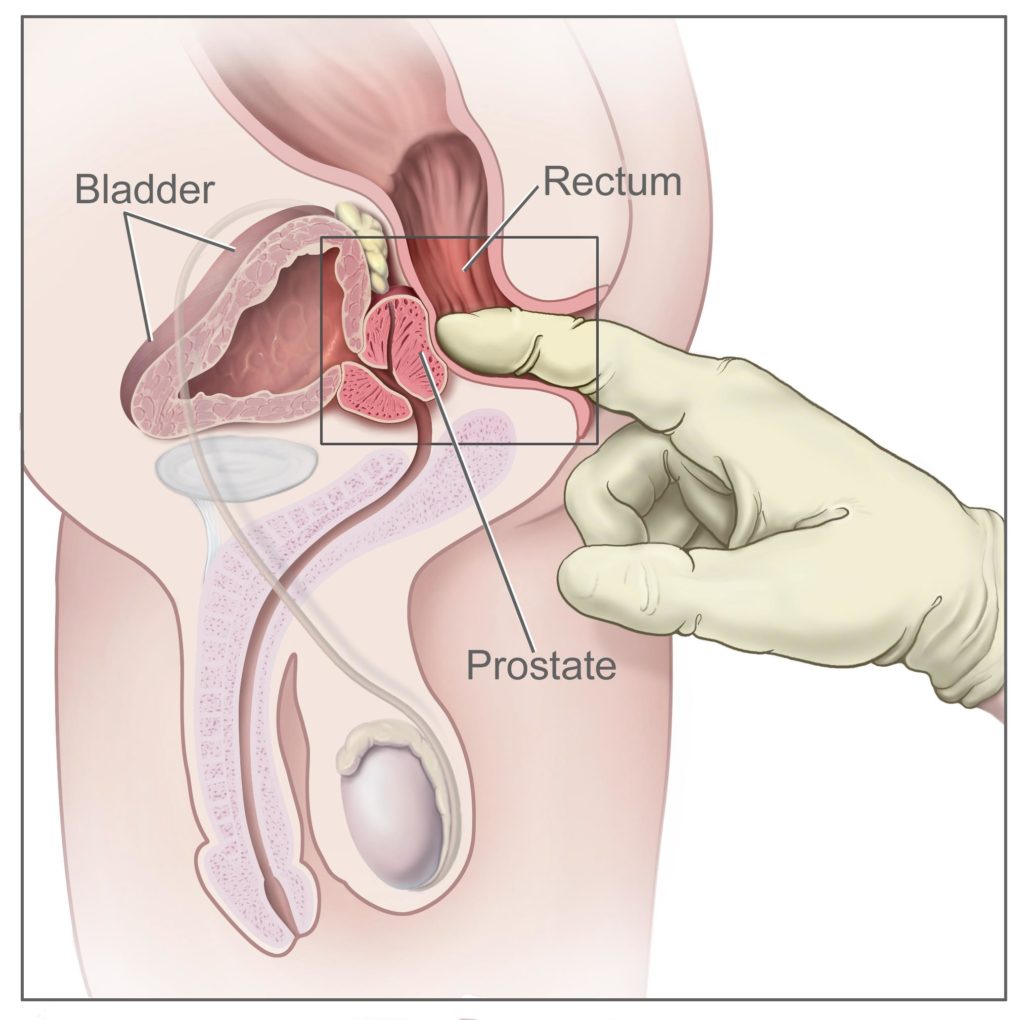
- Urinary incontinence: This is the inability to control urine flow. It can range from mild leakage to complete loss of bladder control. It often improves over time but can persist in some cases.
- Erectile dysfunction (impotence): Prostate surgery can damage the nerves and blood vessels involved in erections, leading to difficulty achieving or maintaining an erection. Recovery of erectile function varies among individuals, and some may require additional treatments such as medication or devices to aid in achieving erections.
- Changes in orgasm: Some men may experience changes in the sensation of orgasm following prostate surgery. This can include decreased intensity or dry orgasms (orgasm without ejaculation).
- Infertility: Prostatectomy typically results in a loss of fertility because the prostate gland produces a significant portion of the fluid in semen.
- Changes in penis length: Some men may experience a shortening of the penis following surgery. This can occur due to scarring or changes in the anatomy of the pelvic region.
- Bowel problems: Prostate surgery can sometimes lead to bowel problems such as diarrhea, constipation, or rectal leakage. These issues are usually temporary but may require management.
- Lymphedema: Removal of lymph nodes during surgery can sometimes lead to lymphedema, a condition characterized by swelling due to the accumulation of lymph fluid. This typically affects the legs but can also occur in the genital area.
While my own cancer is very different from prostate cancer I have been following the success and complications of prostatectomy for years. Several of my friends have undergone this procedure and I have made it a priority to learn about it in order to outline the pros and cons of this aggressive therapy.
To Learn more about prostatectomy, read the posts linked below-
Have you been diagnosed with PCa? What stage? What therapies are you considering? Please watch the free cancer coaching webinar to the right of this page to learn more.
Thank you,
David Emerson
- Cancer Survivor
- Cancer Coach
- Director PeopleBeatingCancer
Recommended Reading:
“The aim of the present study was to evaluate how serum testosterone level (T) can affect urinary continence and erectile function in patients undergoing radical prostatectomy (RP). We included 257 patients with clinically localized prostate cancer, those who had filled out the preoperative quality of life questionnaires (University of California, Los Angeles Prostate Cancer Index, International Index of Erectile Function (IIEF)), and those who had T and total PSA sampled the day before surgery.
We calculated correlations between T and age, body mass index (BMI), PSA, urinary function or bother (UF, UB) and sexual function or bother (SF, SB) and IIEF-5 in the whole population and in sub-populations with normal (⩾10.4 nmol l−1) and low (<10.4 ng ml−1) T using Pearson’s and Spearman’s correlation coefficients…
Finally, a significant result of our study is the strong correlation between urinary symptoms and sexual function in eugonadal (healthily functioning gonads) men, and the lack of this correlation in hypogonadal men…
Conclusion-We demonstrated a significant association between preoperative PSA and testosterone in men with low T (T<10.4 nmol l−1) levels before prostatectomy, and this correlation was not evident in men with normal T.
Moreover, we showed that before RP men with low T presented significantly worse erectile function (lower SF scores) compared with men with normal T, and that T is positively correlated with erectile function when it is >10.4 nmol l−1.
Finally, men with normal T preoperatively presented a strong correlation between their urinary continence and sexual activity…”
“This study was a randomized controlled trial. Pelvic floor muscle exercises were applied to the procedure group three times a day for 6 months. No exercises were applied to the control group. Incontinence and quality-of-life assessments of the 60 patients in the experimental and control groups were performed on months 0 (10 days after removal of the urinary catheter), 1, 3, and 6 through face-to-face and telephone interviews.
Total Incontinence Consultation on Incontinence-Short Form scores, which provide an objective criterion for the evaluation of individuals with incontinence problems, decreased over time. This decrease was statistically highly significant in the third and sixth months.
Pelvic muscle floor exercises are suitable for patients experiencing incontinence after radical prostatectomy.”