- You are here:
- Home »
- Blog »
- pre-cancer »
- Proton-Pump Inhibitors Up Kidney Disease Risk
Proton-Pump Inhibitors Up Kidney Disease Risk
“This study demonstrated an increased risk of CKD or ESRD among Proton Pump Inhibitor users. Whether this association is causal requires further investigations.”
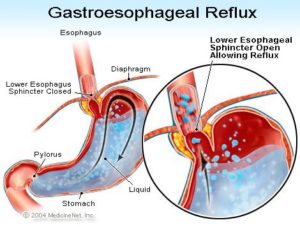
I’m coming at the issue of Proton Pump Inhibitors and kidney disease from a different perspective. I’m writing this post as a long-term cancer survivor. Gastroesophageal Reflux Disease (G.E.R.D.) increases the risk of Barrett’s Esophagus. BE increases the risk of esophageal cancer. Reducing your risk of cancer, any cancer, should be a priority in life.
GERD is a relatively simple health issue that few people really worry about. Taking antacids or PPI’s are a relatively easy fix of this problem. The challenge, as I see it, is that people often take PPI’s for much longer than they are supposed to. Many of us live with lots of distractions in life- job, relationships, kids, etc.
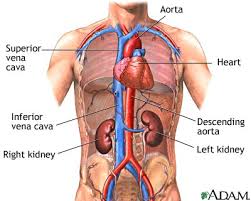
The problem is, as the studies linked and excerpted below explain, long-term use of PPI’s can lead to kidney damage, chronic kidney disease or even end-stage renal disease.
It may be difficult for you to get temporary relief from your acid reflux by taking Pepcid, Nexium, or Prilosec (PPI medications) and also worry about your long-term side effects from these over-the-counter therapies. All I can say is the your risk of long-term side effects of PPI use is real and there are non-toxic therapies to reduce GERD in addition to lifestyle therapies.
If you would like to learn more about reducing your symptoms of GERD, scroll down the page, post a question or comment and I will reply to you ASAP.
Thank you,
David Emerson
- MM Survivor
- MM Cancer Coach
- Director PeopleBeatingCancer
Recommended Reading:
- Lytic Lesions Increase Risk of Death in Multiple Myeloma
- MGUS Progressing to Multiple Myeloma- Obesity and Inflammation?
- Multiple Myeloma Chemotherapy- Daratumumab Increases Risk of Listeria
Efficacy of turmeric in the treatment of digestive disorders: a systematic review and meta-analysis protocol
“Our study aims to systematically review the therapeutic and adverse effects of turmeric and its compounds on digestive disorders, including dyspepsia, peptic ulcer, irritable bowel disease, Crohn’s disease, ulcerative colitis, and gastroesophageal reflux disease…”
Proton Pump Inhibitors and Risk of CKD: A Meta-analysis
“Proton pump inhibitors (PPIs) are one of the most commonly prescribed medications worldwide. Recent studies have raised a concern over increased risk of chronic kidney disease (CKD) or end-stage renal disease (ESRD) among PPIs users but the results of those studies were inconsistent. This meta-analysis was conducted to summarize all available data and to estimate this potential association.
RESULTS- Of 8,950 studies, five studies (three cohort studies and two case-control studies) with 536,902 participants met the eligibility criteria and were included in the meta-analysis. We found that individuals with PPIs use had significantly increased the risk of CKD or ESRD when compared with non-PPIs users (pooled RR of 1.33, 95% CI, 1.18-1.51). There was no publication bias of overall included studies assessed by the funnel plots.
CONCLUSION- This study demonstrated an increased risk of CKD or ESRD among PPIs users. Whether this association is causal requires further investigations.”
Proton Pump Inhibitor Use May Up CKD, ESRD
“Proton pump inhibitor (PPI) users have an increased risk of chronic kidney disease (CKD) or end-stage renal disease (ESRD), according to a review presented at the annual meeting of the American Society of Nephrology, being held in New Orleans.
Karn Wijarnpreecha, MD, from Bassett Medical Center in Cooperstown, New York, and colleagues conducted a literature review to identify all studies through March 2017 that evaluated the risk of CKD or ESRD among PPI users versus non-PPI users. Five studies (three cohort studies and two case-control studies with 536,902 participants) were included in the meta-analysis…
The researchers found that PPI users had a significantly increased risk of CKD or ESRD versus non-PPI users (pooled relative risk, 1.33). Funnel plots showed no publication bias for included studies.
“This study demonstrated an increased risk of CKD or ESRD among PPI users. Whether this association is causal requires further investigations,” the authors write.”