Diagnosed with Cancer? Your two greatest challenges are understanding cancer and understanding possible side effects from chemo and radiation. Knowledge is Power!
Learn about conventional, complementary, and integrative therapies.
Dealing with treatment side effects? Learn about evidence-based therapies to alleviate your symptoms.
Click the orange button to the right to learn more.
- You are here:
- Home »
- Blog »
- non-conventional therapies »
- Radiation Dermatitis- Short, Long-term Damage
Radiation Dermatitis- Short, Long-term Damage
“Radiation dermatitis is one of the side effects of cancer treatment radiotherapy that people experience most often. Also known as radiodermatitis, it happens when radiation therapy damages the outer layers of a person’s skin.
Radiation dermatitis aka radiodermatitis, is a common side effect of radiation therapy. Local radiation can damage your skin. No big secret here. The challenge for many cancer survivors is that radiation dermatitis can be either/or a short-term or a long term side effect.
Because RD is not well understood or studied by conventional oncology, most cancer patients don’t know to take preventative steps before, during or after their radiation. As the saying goes, “an ounce of prevention is worth a pound of cure.”
I underwent local radiation to my neck and again a year or so later, to my lower back. Same cancer but two different areas for two different reasons.
The local radiation to my neck caused redness and irritation to my skin but little outward damage. I have chronicled the radiation damage to my salivary glands (xerostomia) and swallowing muscles (dysphagia) in the recommended reading section below.
The radiation to my lower back was a higher dose and therefore caused more serious radiation dermatitis on the outside as well as radiation damage to the bone, muscle and nerves.
As I often lament, I wish I knew then what I know now. According to the studies linked and excerpted below, the following evidence-based but non-conventional therapies would have helped me manage my RD-
- Green Tea- EGCG
- Antioxidants-
- Hyberbaric Oxygen therapy-HBOT
Are you about to undergo radiation therapy? Have you recently completed radiation therapy? Scroll down the page, post a question or comment and I will reply to you ASAP.
To Learn More About Side Effects of Chemo and Radiation- click now
Hang in there,
David Emerson
- Cancer Survivor
- Cancer Coach
- Director PeopleBeatingCancer
Recommended Reading:
- Radiation-induced Dysphagia-Difficulty Swallowing
- Radiation-induced Xerostomia- Dry Mouth
- Chemo-Radiation-Induced Short-Term Side Effects
Radiation & Inflammation
“The immune system has the power to modulate the expression of radiation-induced normal and tumor tissue damage. On the one hand, it can contribute to cancer cure, on the other it can influence acute and late radiation side effects, which in many ways resemble acute and chronic inflammatory disease states.
The way radiation-induced inflammation feeds into adaptive antigen-specific immune responses adds another dimension to the tumor-host crosstalk during radiation therapy and to possible radiation-driven autoimmune responses.
Understanding how radiation impacts inflammation and immunity is therefore critical if we are to effectively manipulate these forces for benefit in radiation oncology treatments…”
What to know about radiation dermatitis
“Radiation dermatitis is one of the side effects of cancer treatment radiotherapy that people experience most often.
Also known as radiodermatitis, it happens when radiation therapy damages the outer layers of a person’s skin.
An estimated 95 percent Trusted Source of people who receive radiation therapy will have some form of radiation dermatitis, including redness, skin dryness, or skin peeling.
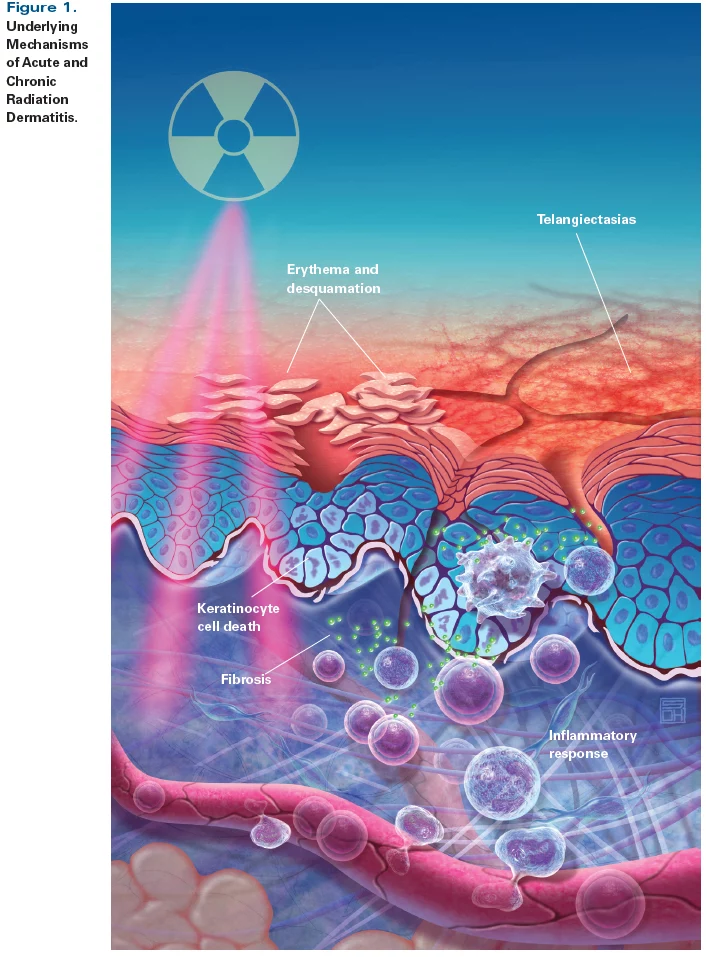
Chronic radiation-induced dermatitis: challenges and solutions
“Chronic radiation dermatitis is a late side effect of skin irradiation, which may deteriorate patients’ quality of life. There is a lack of precise data about its incidence; however, several risk factors may predispose to the development of this condition.
It includes radiotherapy dose, fractionation, technique, concurrent systemic therapy, comorbidities, and personal and genetic factors. Chronic radiation dermatitis is mostly caused by the imbalance of proinflammatory and profibrotic cytokines.
Clinical manifestation includes changes in skin appearance, wounds, ulcerations, necrosis, fibrosis, and secondary cancers. The most severe complication of irradiation is extensive radiation-induced fibrosis (RIF). RIF can manifest in many ways, such as skin induration and retraction, lymphedema or restriction of joint motion.
Diagnosis of chronic radiation dermatitis is usually made by clinical examination. In case of unclear clinical manifestation, a biopsy and histopathological examination are recommended to exclude secondary malignancy. The most effective prophylaxis of chronic radiation dermatitis is the use of proper radiation therapy techniques to avoid unnecessary irradiation of healthy skin.
Treatment of chronic radiation dermatitis is demanding. The majority of the interventions are based only on clinical practice. Telangiectasia may be treated with pulse dye laser therapy. Chronic postirradiation wounds need special dressings. In case of necrosis or severe ulceration, surgical intervention may be considered. Management of RIF should be complex. Available methods are rehabilitative care, pharmacotherapy, hyperbaric oxygen therapy, and laser therapy. Future challenges include the assessment of late skin toxicity in modern irradiation techniques..”
Antioxidant Diet Supplementation Starting 24 Hours after Exposure Reduces Radiation Lethality
“Antioxidants mitigate radiation-induced lethality when started soon after radiation exposure, a delivery time that may not be practical due to difficulties in distribution and because the oral administration of such agents may require a delay beyond the prodromal stage of the radiation syndrome.
We report the unexpected finding that antioxidant supplementation starting 24 h after total-body irradiation resulted in better survival than antioxidant supplementation started soon after the irradiation.
The antioxidant dietary supplement was
- l-selenomethionine,
- sodium ascorbate,
- N-acetyl cysteine,
- α-lipoic acid,
- α-tocopherol succinate,
- and co-enzyme Q10.
Total-body irradiation with 8 Gy in the absence of antioxidant supplementation was lethal by day 16. When antioxidant supplementation was started soon after irradiation, four of 14 mice survived. In contrast, 14 of 18 mice receiving antioxidant supplementation starting 24 h after irradiation were alive and well 30 days later.
The numbers of spleen colonies and blood cells were higher in mice receiving antioxidant supplementation starting 24 h after irradiation than in mice receiving radiation alone. A diet supplemented with antioxidants administered starting 24 h after total-body irradiation improved bone marrow cell survival and mitigated lethality, with a radiation protection factor of approximately 1.18…”
Green Tea Ingredient Shows Promise for Preventing Severe Radiation Dermatitis
“Prophylactic use of a green tea constituent significantly reduced the incidence and severity of radiation-induced dermatitis (RID) in breast cancer patients in a randomized trial, researchers say.
The incidence of grade 2 or worse RID was significantly lower in patients treated with the green tea constituent – epigallocatechin-3-gallate, or EGCG – than in the placebo group…
EGCG has the potential to become a new skin care option for patients receiving radiotherapy, the investigators believe…
Most cases of RID began two to three weeks after the start of radiotherapy, but the average interval to RID appearance was delayed in the EGCG group compared to the placebo group (3.27 weeks vs 2.89 weeks; P=0.001)…
Compared to the placebo group, the EGCG group had significantly lower rates of grade 2 burning feeling (19.8% vs 44.4%), itching (41.4% vs 72.2%), pain (13.5% vs 24.1%), and tenderness (21.6% vs 46.3%).
There were no serious adverse effects related to the application of either EGCG or placebo…”