Diagnosed with Cancer? Your two greatest challenges are understanding cancer and understanding possible side effects from chemo and radiation. Knowledge is Power!
Learn about conventional, complementary, and integrative therapies.
Dealing with treatment side effects? Learn about evidence-based therapies to alleviate your symptoms.
Click the orange button to the right to learn more.
- You are here:
- Home »
- Blog »
- side effects ID and prevention »
- Radiation for Bone Mets-
Radiation for Bone Mets-
“Radiotherapy for painful bone metastases is a standard of care, but a new study that looked at earlier use of the modality had an unexpected result.”
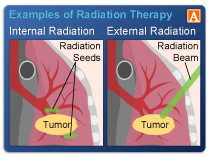
To say that local radiation therapy for bone mets has pros and cons is an understatement. I say this because I underwent three courses of prophylactic radiation therapy to manage my cancer. The pros- bone pain subsides within weeks. The cons? I developed radiation-induced lumbosacral plexopathy as well as many other long-term side effects in the years following treatment.
I find it interesting that the first two articles linked below basically are polar opposites on the issue of local radiation for the treatment of bone mets. In my experience, this simply means that both are true- radiation can be used to over-treat and/or radiation can be used too little, depending on the oncologist and depending on the institution.
And the third article below explains that the use of local radiation must be tailored to the patient. Essentially saying what I am saying…
So what is the cancer patient to do? Here is what I’ve learned since my cancer diagnosis in 2004.
- Understand the challenge. You are not an oncologist but you are the person who will experience the risks and benefits of local radiation for bone mets.
- Consider evidence-based non-conventional therapies cited to enhance and/or protect radiation therapy- consider:
Radiation therapy zapped my lesions buying me months of pain-free survival. Pain-free survival that allowed me to find the evidence-based, non-conventional, controversial therapy that put me into complete remission. But by undergoing so much radiation, I developed serious nerve damage that will probably put me in a wheelchair someday.
Would you risk local radiation to treat your own bone mets knowing the pros and cons of doing so?
David Emerson
- Cancer Survivor
- Cancer Coach
- Director PeopleBeatingCancer
Recommended Reading:
- Multiple Myeloma Q and A- Bone Involvement
- Multiple Myeloma Side Effects- Radiation-Induced Lumbosacral Plexopathy
- Multiple Myeloma Bone Therapy- Cissus Quadrangularis
- Lytic Lesions Increase Risk of Death in Multiple Myeloma
- Multiple Myeloma Symptoms, Side Effects- Vitamin D3
Groundbreaking’: Prophylactic Radiotherapy Ups Survival
“Radiotherapy for painful bone metastases is a standard of care, but a new study that looked at earlier use of the modality had an unexpected result. It showed that prophylactic radiotherapy given to patients with cancer and asymptomatic bone metastases not only reduces skeletal-related events and hospitalizations, but also offers a survival benefit.
In the first study of its kind, almost 80 patients with more than five high-risk metastases were randomly assigned to receive either prophylactic radiotherapy or standard care…
“It suggests that treating to cure the cancer is not the only thing that can help people live longer,” she said in a statement…
Speaking to Medscape Medical News, Siva said that the use of radiotherapy for symptomatic bone pain is a “well-established standard of care,” but the question addressed by the current study — in which radiotherapy was used for asymptomatic bone metastases — was “whether we can bring forward this treatment to improve outcomes”…
As for the magnitude of the survival benefit, Siva said that, “if this was drug A, then there would be a very large and interested pharmaceutical market chasing after this…”
Gillespie acknowledged that “more work is needed to optimize the appropriate use” of radiotherapy in order “to avoid overtreatment,” but also on how to identify these patients while they still have asymptomatic bone metastases “since we may not always see them.”
… said studies like the current one “illustrate the importance of the role of the radiation oncologist not only in the treatment of cancer, but also in our role in the overall healthcare and delivery system and health of our patients, for example, on issues around cost containment, by prevention of hospitalizations, or morbidity…”
The patients were required to be age 18 or older, and have an ECOG performance status of 0–2, a solid tumor malignancy, and more than five metastatic sites on imaging. At least one of those metastases should have been high-risk, defined as bulky disease of >2 cm, or involving the hip, shoulder or sacroiliac joints, the long bones, or the junctional spine and/or posterior element…
The median age of the patients was 61-65 years, and around half were female. The most common histologies were lung, breast, and prostate cancer, and 90% were planned to have systemic therapy. About half of patients had received a bone-modifying agent…
The primary endpoint of the study was skeletal-related events, defined as pathologic fracture, cord compression, surgery for instability, or radiotherapy for pain.
A skeletal-related event occurred in just 1.6% of patients given prophylactic radiotherapy vs 29% in the no radiotherapy arm (P < .001)…
In terms of safety, grade 2 or higher adverse events were experienced by 38% of patients in the radiotherapy arm vs 21% in the control group, with 13% and 3%, respectively, deemed to be potentially treatment-related. The most common events were nausea, emesis, erythema, fatigue, and diarrhea, the majority of which were grade 2…
Statewide quality improvement project reduced excessive radiation treatments for bone metastases by 80%
“The effort by the Michigan Radiation Oncology Quality Consortium reduced unnecessary medical procedures, and saved the time and resources of patients and families…”
Paper cited: “Contemporary practice patterns for palliative radiotherapy of bone metastases: Impact of a quality improvement project on extended fractionation,” Practical Radiation Oncology. DOI: 10.1016/j.prro.2021.05.002
How Radiation Therapy Is Becoming More Personal
Thanks to advances in radiation therapy, treating all patients with a particular tumor the same is becoming a thing of the past…
Now, clinicians can see — in real-time — how an individual patient’s tumor is responding to therapy, and make adjustments during treatment…