What is the newest treatment for multiple myeloma? What is the success rate, what are the side effects? How much will it cost???
I am posting Tom’s account for three reasons- first, CAR T-Cell therapy is one of the newest treatments for multiple myeloma (MM). Second, many MMers are intensely interested in learning more about CAR-T cell therapy and three,Tom has done a thorough job of listing all important stages, issues, etc. The information below is Tom’s account, in Tom’s words.
Please keep in mind that the newest treatments for MM change frequently. Research, FDA approval (or not) change the landscape for newest treatments regularly. But this is also the way we want it…
Lastly, Tom gave me an email address for any/all readers to email questions to him.
To Learn More about CAR-T Therapy and Myeloma- click now
David Emerson
- MM Survivor
- MM Cancer Coach
- Director PeopleBeatingCancer
Recommended Reading:
My Multipe Myeloma journey:
I started getting MM symptoms 4 years prior to CAR-T and was diagnosed two years ago.
I refused stem cell transplantation and initially opted for Velcade, Revlimid, Dexamethason of which I did 6 cycles or 24 infusions. I was refractory to the treatment.
I then started on Daratumumab (CD 38 marker) weekly for 8 weeks and bi-monthly for 2 months and very quickly got good results but hit a barrier beyond which no further improvements were made.
The doctor was unable to explain why. The answer became apparent once I started CAR-T preparations when my bone marrow results showed that I was negative for CD38 marker, meaning that Daratumumab had worked perfectly.
The problem was that I had other MM strains which didn’t carry the CD38 marker. MM is not a homogeneous cancer.
After two years of taking 4mg weekly of Dexamethasone and almost daily Lenalidomide alongside loads of secondary meds and treatment drugs, I suffered many side effects such as corneal toxicity (my eye sight is only just starting to recover) and ear ringing (temporary).
Dexamethasone in particular is a nasty steroid that not only causes violent mood swings, difficulty in mental focusing and insomnia but also painful swelling of the stomach.
My most severe side effect has been memory impairment or chemo brain. I still find it hard to recover short to medium term memory or vocabulary words, although it is slowly improving. Remembering names and events is sometimes a challenge.
I also note a distinct dimness and slowness in my mental faculties, hopefully this will also be temporary in nature.
The CAR-T treatment took place in the following way:
- I underwent CAR-T (Chimeric Antigen Receptor T-cell) treatment at the Secondary University Hospital of Jiaotong in Xi’an, China headed by Dr. Wanhong Zhao.
- T-lymphocytes were collected through a blood extraction process which took about 2 hours (thick needles, but little pain)
- Prior to this I received three days of cyclophosphamide chemotherapy. Side effects were moderate breathlessness and partial hair loss 3 months later.
- These were sent to Legend Biotech Laboratory in Nanjing. They were genetically modified within a week.
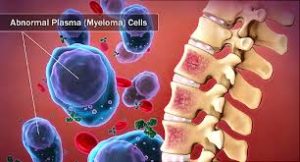
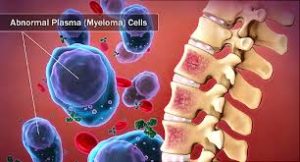
- Here “markers” were placed on the T-lymphocytes. In my case they were BCMA (B-Cell Maturation Antigen) markers. These markers have the specificity that they bind exclusively to MM protein receptors. Once they bind the T-Cells are able to kill the MM cells.
- Prior to CAR-T, I received for three days cyclophosphamide and fludarabine chemo-cocktail. Side effects were moderate breathlessness and dizzy spells and partial hair loss 3 months later.
- After 48 hours rest, I received the BCMA engineered T-cells in three doses (total 130 million cells) day 1, day 3 and day 7.
- I then waited for about 10 days for my body to show signs of fever. At this point hospitalisation is mandatory.
- The CAR-T was injected following the immuno-repressent chemo treatment to limit the body from attacking. When CAR-T cells came into contact with MM cells they got stimulated and started to multiply.
- Once the CAR-T numbers grew in numbers the body reacted with an all out alarm to the “foreign” invasion and high temperature and flu like symptoms ensued.
- Fever climbed to over 40ºC for 5 days and ice packs and fever medication was used to limit the rise.
- CTS (Cytokin release syndrome) at this stage can be a mortal threat as organs can start to fail so constant monitoring was carried out. However, a controlled reaction must take place for the treatment to work.
- On the fifth day my blood pressure fell to around 50/50 and I was administered an antibody to stop the mild CTS and within a few hours I was able to leave the hospital.
- In summary the CAR-T multiply as they get into contact with MM cells and kill them, whilst at the same time the body’s immune system attacks the CAR-T cells.
- In less than 10 days all traces of MM had disappeared from my bone marrow. Previously I had up to 48% MM infiltration prior to CAR-T.
- Low levels of M-Protein linger in the blood months after treatment. These residual amounts diminish 50% every 4 weeks and take over 3 months to be completely eliminated.
- My current post-CAR-T side effects are lung infections (mild to medium), and random allergic coughing.
- I am told it will take 12 months for my immune system to normalise and 12 months for my skeletal system to recover.
I have had a full response and have zero Minimum Residual Disease with only trace amounts of Kappa protein showing up. CAR-T@Koenye.com
Relapsed Refractory Multiple Myeloma? CAR-T vs. Triplet Therapy
“All 16 patients who had a response (partial response or better) and who could be evaluated for minimal residual disease (MRD) had MRD-negative status…”
You were diagnosed with multiple myeloma (MM) years ago. Your first remission was the longest and you’ve relapsed twice or three times now and your remissions are getting shorter. You’ve probably been dealing with short, long-term and late stage side effects…for years. You’ve read about CAR-T therapy…
There has been a lot of talk about CAR-T Cell therapy. Based on the studies I’ve read, CAR-T does seem as though this therapy elicits a greater overall response and a longer PFS than does the standard-of-care doublet or even newer triplets.
But at what cost? Side effects and financial cost seem to be serious. Make sure you understand this therapy.
The challenge of the RRMM is to make sense of the alphbet soup of relapsed/refractory multiple myeloma (RRMM) therapies. Is PCD better for you than CAR-T or the standard-of-care? The key is to compare apples to apples and apply what you learn to your specific situation.
Compare:
- overall/objective response rate– how many patients responded to a given chemo cocktail-
- adverse events aka side effects– more MMers may respond to a chemo cocktail but there may be more side effects as well-
- PFS-Progression-Free Survival- how long, on average, before the MMer relapsed-
- OS-Overall Survival-how long the MMer lived-
- Cost– does your insurance pay for the therapy.
Recommended Reading:
“Triplet treatment with the combination of pomalidomide, cyclophosphamide, and dexamethasone (PCD) in patients with relapsed or refractory multiple myeloma (RRMM) who have received at least 2 prior lines of therapy could improve clinical outcomes, according to study results published in the Annals of Hematology…
The overall response rate was 76%, with 27% of patients achieving very good partial response. Median time to best response was 3.6 months.
No patients achieved a complete response. The authors noted this could be because none of the patients who experienced immunofixation underwent bone marrow aspiration, as bone marrow aspiration is rarely performed outside the context of clinical trials…
After a median follow-up of 16 months, median progression-free survival (PFS) was 7.3 months and median overall survival (OS) was not reached.
Nine patients had high-risk cytogenetics, and median PFS was shorter in this group (3.3 months) compared with patients who had standard-risk cytogenetics (7.9 months; P =.0027). OS was similarly shorter in patients with high-risk cytogenetics, at 6.5 months compared with not reached (P =.003).
The most frequent adverse event was hematologic toxicity, with 37% of patients experiencing grade 3 or 4 cytopenia. Adverse events resulted in discontinuation of therapy in 18% of patients.
The authors concluded that treatment with PCD was feasible and cost effective, and that it resulted in improved response rates and PFS compared with doublet pomalidomide and dexamethasone treatment, which is currently the standard of care in this patient population.”
“The phase 3 study enrolled 307 patients in 24 countries with relapsed or refractory multiple myeloma who had received at least two prior therapies. They received either pom-dex alone or pom-dex in tandem with isatuximab.
The isatuximab combo kept cancer at bay for a median of 11.5 months, a five-month improvement over the 6.5 months for pom-dex alone. It also increased the number of patients for whom pom-dex worked—the combo shrank tumors in 60% of patients, compared to 35% for the standard of care alone. What’s more, of the patients who responded to treatment, the isatuximab combo worked faster, taking a median of 35 days to get a response versus 58 days for pom-dex alone…
An analysis showed that the isatuximab combo performed similarly in different subgroups, including the elderly and people with poor kidney function…”
“Preclinical studies suggest that bb2121, a chimeric antigen receptor (CAR) T-cell therapy that targets B-cell maturation antigen (BCMA), has potential for the treatment of multiple myeloma…
Results for the first 33 consecutive patients who received a bb2121 infusion are reported. The data-cutoff date was 6.2 months after the last infusion date.
Hematologic toxic effects were the most common events of grade 3 or higher, including
- neutropenia (in 85% of the patients),
- leukopenia (in 58%),
- anemia (in 45%), and
- thrombocytopenia (in 45%).
A total of 25 patients (76%) had cytokine release syndrome, which was of grade 1 or 2 in 23 patients (70%) and grade 3 in 2 patients (6%).
Neurologic toxic effects occurred in 14 patients (42%) and were of grade 1 or 2 in 13 patients (39%). One patient (3%) had a reversible grade 4 neurologic toxic effect.
The objective response rate was 85%, including 15 patients (45%) with complete responses. Six of the 15 patients who had a complete response have had a relapse. The median progression-free survival was 11.8 months (95% confidence interval, 6.2 to 17.8).
All 16 patients who had a response (partial response or better) and who could be evaluated for minimal residual disease (MRD) had MRD-negative status (≤10−4 nucleated cells). CAR T-cell expansion was associated with responses, and CAR T cells persisted up to 1 year after the infusion…
CONCLUSIONS-We report the initial toxicity profile of a BCMA-directed cellular immunotherapy for patients with relapsed or refractory multiple myeloma. Antitumor activity was documented.