
Diagnosed with Cancer? Your two greatest challenges are understanding cancer and understanding possible side effects from chemo and radiation. Knowledge is Power!
Learn about conventional, complementary, and integrative therapies.
Dealing with treatment side effects? Learn about evidence-based therapies to alleviate your symptoms.
Click the orange button to the right to learn more.
- You are here:
- Home »
- Blog »
- Pre-Myeloma »
- Best Imaging Methods – SBP, MGUS, SMM
Best Imaging Methods – SBP, MGUS, SMM
“Our study confirms that WB MRI detects skeletal disease in a higher number of treatment-naïve (Multiple Myeloma) patients than PET/CT..”
What are the best imaging methods for both myeloma and pre-myeloma? The study linked and excerpted below is studying the sensitivity of both MRI and PET/CT detecting “skeletal disease” in multiple myeloma patients.
Fine. But what about the best imaging methods for detecting bone disease in pre-multiple myeloma? Monoclonal Gammopathy of Undetermined Significance (MGUS) or Smoldering Multiple Myeloma (SMM)?
I’m not challenging the study in any way. I’m simply offering a different reason why a person would get an MRI or PET/CT.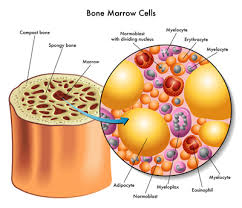
Let me explain.
You have been diagnosed with either a
- single bone plasmacytoma
- MGUS or
- SMM
By itself, none of these diagnostic terms is that worrisome. Pre-MM is not cancer, they are blood disorders. The worrisome issue, in my opinion anyway, is that pre-mm can become full-blown MM.
According to research, the risk of MGUS becoming MM is 1% annually and the risk of SMM becoming MM is 10% for the first three years, 3% for years 4-10 and 1% after year 10.
It is the risk of pre-MM becoming frank MM that is the issue. I believe the study below can give you key info to help determine your risk of your pre-MM becoming frank MM.
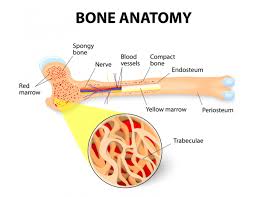
Your m-spike can go up and down. Your immunoglobulins, free light chains, blood cells, all can go up and down. But bone involvement, monoclonal proteins IN your bone marrow, that is important to determine. Therefore you will want to determine the best imaging methods to detect possible bone involvement.
If you have been diagnosed with pre-MM, talk to your oncologist about whole body MRI (WBMRI).
- To Learn More About Solitary Bone Plasmacytoma- click now
- To Learn More About the pros and cons of Ionising Radiation- click now
- To Learn More about a Pre-Myeloma Diagnosis- click now
If you are interested in learning more about evidence-based therapies as well as the best imaging methods shown to reduce the risk of MM, scroll down the page, post a question or comment and I will reply to you ASAP.
Thanks,
David Emerson
- MM Survivor
- MM Cancer Coach
- Director PeopleBeatingCancer
Recommended Reading:
Risk of SMM to MM- Imaging too?
Comparison of the diagnostic performance and impact on management of 18F-FDG PET/CT and whole-body MRI in multiple myeloma
“This study compared the diagnostic performance and impact on management of 18F-fluorodeoxyglucose positron emission tomography/computed tomography (18F-FDG PET/CT) and whole-body magnetic resonance imaging (WBMRI) in treatment-naive myeloma…
Blinded clinical and imaging data were reviewed by two haematologists in consensus and management recorded following clinical data ± 18F-FDG PET/CT or WBMRI. Bone disease was defined using International Myeloma Working Group (IMWG) criteria and a clinical reference standard. Per-patient sensitivity for lesion detection was established. McNemar test compared management based on clinical assessment ± 18F-FDG PET/CT or WBMRI…
Results-
Sensitivity for bone lesions was 69.6% (32/46) for 18F-FDG PET/CT (54.3% (25/46) for PET component alone) and 91.3% (42/46) for WBMRI. 27/46 (58.7%) of cases were concordant.
In 19/46 patients (41.3%) WBMRI detected more focal bone lesions than 18F-FDG PET/CT. Based on clinical data alone, 32/46 (69.6%) patients would have been treated. Addition of 18F-FDG PET/CT to clinical data increased this to 40/46 (87.0%) patients (p = 0.02); and WBMRI to clinical data to 43/46 (93.5%) patients (p = 0.002).
The difference in treatment decisions was not statistically significant between 18F-FDG PET/CT and WBMRI (p = 0.08)…
Conclusion
Compared to 18F-FDG PET/CT, WBMRI had a higher per patient sensitivity for bone disease.
However, treatment decisions were not statistically different and either modality would be appropriate in initial staging, depending on local availability and expertise…
A small number of studies, with limited sample sizes, have compared the diagnostic accuracy of 18F-FDG PET/CT and WBMRI in myeloma [2,3,4,5], but to date, there has been a lack of comparative data of the impact on management of 18F-FDG PET/CT and WBMRI.
Both techniques have advantages. While WBMRI has superior sensitivity for diffuse bone marrow infiltration [6], 18F-FDG PET/CT better demonstrates lesion viability following treatment [7];
both convey prognostic information [8, 9].
Additionally, in patients with smouldering myeloma, the presence of >1 focal bone lesion detected by WBMRI [10] or the presence of a focal FDG-avid lesion [11] is a strong prognostic factor for progression to myeloma such that they are now recognised as an indication to treat otherwise asymptomatic myeloma [12, 13]…
…We hypothesised that the greater sensitivity of WBMRI for detection of myeloma compared to 18F-FDG PET/CT would alter patient management in a greater proportion of cases. Thus, the primary aim of this study was to compare the diagnostic performance of 18F-FDG PET/CT and WBMRI for bone disease in patients with a new myeloma diagnosis and to assess whether management differed depending on which imaging was performed initially…
18F-FDG PET/CT
There was moderate agreement between the two readers in scoring for the presence/absence of focal CT and PET disease, with a kappa score of 0.44 and 0.47, respectively. Identification of CT disease was discordant in 3/12 patients, where CT positive but FDG-negative lesions were noted by one reader. Identification of FDG-positive disease was also discordant in 3/12 patients.
Whole-body MRI
There was excellent agreement between the two readers in scoring for the presence/absence of focal lesions on a per patient basis (kappa score, 1.00). With respect to the scoring of the number of lesions across the 7 regions, mean ± SD focal lesion score was 7.4 ± 5.7 for Reader 1 and 7.7 ± 5.5 for Reader 2; with an intraclass correlation coefficient of 0.95 [95%CI: 0.84-0.99].
With respect to the presence/absence of bone marrow infiltration, there was good agreement between both readers with a kappa score of 0.74; one patient with a bone marrow infiltration percentage of 90% on biopsy was assigned incorrectly as negative by one reader…
Impact on clinical management
Based on the review of clinical data alone, 32/46 (69.6%) of patients would be treated for myeloma rather than active surveillance, in accordance with institutional treatment protocols. Review of clinical data with 18F-FDG PET/CT resulted in treatment of 40/46 (87.0%) patients, and review of clinical data with WBMRI resulted in treatment of 43/46 (93.5%) patients…
Discussion
Our study confirms that WBMRI detects skeletal disease in a higher number of treatment-naïve patients than 18F-FDG PET/CT and also detects a higher number of lesions per patient with concordance in disease positivity/lesion number in only 59% of patients…

