
Diagnosed with SMM, SPB, or MGUS?
Learn how you can stall the development of full-blown Multiple Myeloma with evidence-based nutritional and supplementation therapies.
Click the orange button to the right to learn more.
- You are here:
- Home »
- Blog »
- Pre-Myeloma »
- Solitary Plasmacytoma on Rib w/ Amyloidosis
Solitary Plasmacytoma on Rib w/ Amyloidosis
“The Bortezomib/Dexamethasone regimen induced high rates of rapid hematologic and organ responses in AL amyloidosis patients.”
Hi David- My wife is newly diagnosed with a solitary plasmacytoma on a rib with amyloidosis. Kappa light chains are 200 mg/L, Lambda are normal at 9. 24 hr. urine is completely normal.
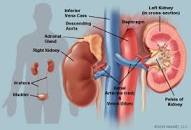
Kidney biopsy confirms Kappa light chains cause of kidney dysfunction with creatinine currently at 1.99, eGFR at 26. Electrolytes are all normal.
My wife is 64 and in otherwise very good health aside from elevated cholesterol. No heart involvement. 5% plasma neoplasm cells in bone marrow. PET-CT shows no lesions other than the rib plasmacytoma.
The MM specialist is highly recommending autologous stem cell transplant and CyBorD as an alternate. We are apprehensive about the aggressive transplant option and have a 2nd opinion appointment scheduled with an amyloidosis specialist.
We would greatly appreciate your thoughts on treatment, cure vs. control, etc. She started taking Fenbendazole and Curcumin three weeks ago as recommended by a relative for whom it completely cured his advanced bladder cancer.
Hi Richard- I am sorry to read of your wife’s Solitary Plasmacytoma of Bone (SPB) diagnosis. I just re-read the blog post that you came in on. I think I was channeling your wife’s situation when I wrote that post :-).
All kidding aside, let me be more specific as to why that post is central to your wife’s situation.
- induction therapy
- ASCT and
- maintenance therapy.
David Emerson
- MM Survivor
- MM Cancer Coach
- Director PeopleBeatingCancer
Recommended Reading:
Multiple Myeloma Chemos That Cause Kidney Damage-
“In this review, we recognized that there are multiple ways novel anti- multiple myeloma therapies can affect renal function, cause kidney damage.”
Kidney damage is tricky for the multiple myeloma (MM) patient and survivor because MM itself can damage your kidneys. Kidney damage can be a symptom of MM. Further, as the article linked below explains, MM chemotherapy itself causes kidney damage as well.
The scariest problem facing newly diagnosed MM patients is quoted in the top article in the very first sentence “effects of these therapies can lead to unanticipated effects on the kidney.” In other words, some of these “novel” MM therapies are not old enough, have not been tested enough for oncology to thoroughly understand the degree of kidney damage caused by novel chemotherapy regimens…
Lastly, and this is my own perspective on MM chemotherapy drugs, the negative kidney effects cannot be fully know and understood, until years after chemo administration. Like all long-term and late stage side effects, a MM patient can’t know the full extent of his or her kidney damage until they’ve lived beyond their MM diagnosis for years, even decades, beyond their original MM diagnosis.
Just knowing they kidney damage can be an issue for multiple myeloma patients can help. Also, there are a number of foods and supplements that can help your kidneys heal…”
- renal (100%),
- cardiac (72%),
- hepatic (19%) or
- nervous system (10%) involvement



