
Recently Diagnosed or Relapsed? Stop Looking For a Miracle Cure, and Use Evidence-Based Therapies To Enhance Your Treatment and Prolong Your Remission
Multiple Myeloma an incurable disease, but I have spent the last 25 years in remission using a blend of conventional oncology and evidence-based nutrition, supplementation, and lifestyle therapies from peer-reviewed studies that your oncologist probably hasn't told you about.
Click the orange button to the right to learn more about what you can start doing today.
- You are here:
- Home »
- Blog »
- Multiple Myeloma »
- Stem Cell Transplant for Newly Diagnosed Multiple Myeloma- What are Risks?
Stem Cell Transplant for Newly Diagnosed Multiple Myeloma- What are Risks?
“Two-thirds of HSCT survivors develop at least one chronic health condition; while a fifth develop severe or life-threatening conditions.”
Dear David- I am a newly diagnosed multiple myeloma (NDMM) patient. My oncologist is advising me to have an autologous stem cell transplant (ASCT)). I know that you question the “risk/benefit” trade off of an ASCT so I’m trying to understand the issues.
So the question becomes for me the individual assessment of the trade off between:
- ASCT with possible longer progression-free survival – which hopefully means less damage to the body from the disease progression vs
- no ASCT with the risk of earlier disease progression, but less damage to the body from the toxic treatment.
Did I understand that somewhat correctly? Ellen
Hi Ellen-
Keep in mind that we are talking about “risks” or the odds or possibility of bodily damage from either regular chemotherapy versus high-dose, aggressive chemotherapy from an ASCT. Many variables in your particular situation can alter the odds, alter specific risks.
I also think it’s important for all newly diagnosed multiple myeloma patients to understand the Cure vs. Control Debate as discussed by Dr. Rajkumar of the Mayo Clinic. In short, conventional MM oncology considers an ASCT to be “potentially curative” even though no one that I know has ever been cured of MM with an ASCT.
To reply to your statement directly “ASCT… which hopefully means less damage to the body from the disease progression…”
If I understand what you are saying, a longer event-free survival (EFS) or first remission means that the patient’s MM does less damage to the patient being in remission. I think you are taking the long-view of MM survival.
While I appreciate your thinking, the challenge is getting over the first hurdle, ASCT, and the damage it causes for the rest of the NDMM patient’s life.
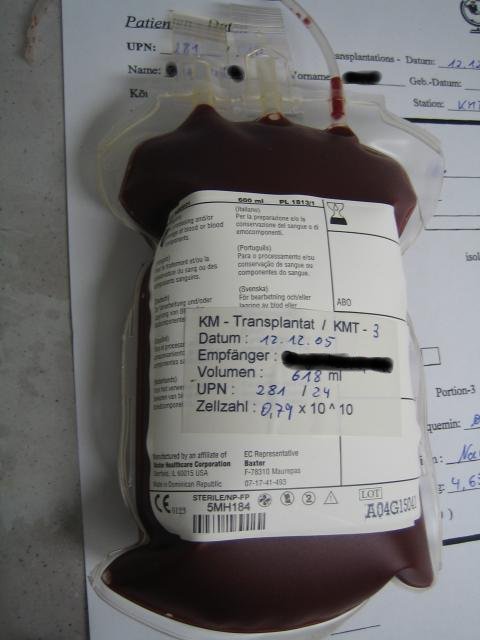
If it’s one thing that is dramatically illustrated in the article linked and excerpted below, an ASCT means more chemotherapy early in the NDMM patient’s life as a MM er. ASCT is designed to kill more MM cells, causing a deeper remission. Patients gain a deeper remission, fewer MM cells in their blood but endure more toxicity in doing so.
The challenge for the NDMM patient is that all this chemo, all this toxicity is early in the process, often in the first year of the patients MM diagnosis.
More toxicity creates more organ damage aka short, long-term and late stage side effects. To be specific
- blood/immune,
- hormone,
- kidney,
- heart, and
- treatment-related secondary cancers.
All preceded by a 2 percent chance that patients die during the procedure itself.
To look at your thinking through the cure vs. control debate, it is the attempt to “cure” a patient’s MM that causes damage and increases the risk of mortality that is the problem. Conversely, by trying to “control” the MM, the patient, in theory anyway, manages both his/her MM as well as his/her health.
I’m not sure I was able to clarify your issues. I hope this helps but be sure to ask me any more questions that you have.
Hang in there,
David Emerson
- MM Survivor
- MM Cancer Coach
- Director PeopleBeatingCancer
Recommended Reading:
- Stem Cell Transplant- Treatment-related Secondary Cancer
- Myeloma Stem Cell Transplant Side Effect- PTSD
- The “best” human stem cells for your bone marrow transplant-
Long-term health impacts of hematopoietic stem cell transplantation inform recommendations for follow-up
“However, hematopoietic stem cell transplantation (HSCT) survivors are at risk of developing long-term complications, such as
- endocrinopathies,
- musculoskeletal disorders,
- cardiopulmonary compromise and
- subsequent malignancies.
These complications have a direct impact on the morbidity and mortality experienced by HSCT survivors. Two-thirds of HSCT survivors develop at least one chronic health condition; while a fifth develop severe or life-threatening conditions.
HSCT patients who have survived for at least 5 years post-transplantation are at a fourfold to ninefold increased risk of late mortality for as long as 30 years from HSCT, producing an estimated 30% lower life expectancy compared with the general population.
The high burden of morbidity experienced by HSCT survivors makes it critically important that there is standardized follow-up of HSCT survivors at high risk for post-HSCT complications…”
In a recent cohort study of 2574 patients who had survived for at least 5 years after allogeneic or autologous HSCT without recurrence of the original disease, Martin et al. evaluated mortality, projected life expectancy and cause of death [106].
The estimated survival of the cohort at 20 years follow-up after HSCT was 80.4%. Mortality rates were four- to ninefold higher than expected in the population for at least 30 years following HSCT, producing an estimated lower life expectancy of 30% compared with the general population, regardless of current age.
Leading causes of the higher mortality rate were:
- SMNs and recurrent diseases,
- followed by infections,
- chronic GvHD,
- respiratory disease and
- cardiovascular disease…


