Diagnosed with Cancer? Your two greatest challenges are understanding cancer and understanding possible side effects from chemo and radiation. Knowledge is Power!
Learn about conventional, complementary, and integrative therapies.
Dealing with treatment side effects? Learn about evidence-based therapies to alleviate your symptoms.
Click the orange button to the right to learn more.
- You are here:
- Home »
- Blog »
- side effects ID and prevention »
- Steroid-Induced Shoulder Avascular, Osteonecrosis: I.D. Therapies
Steroid-Induced Shoulder Avascular, Osteonecrosis: I.D. Therapies
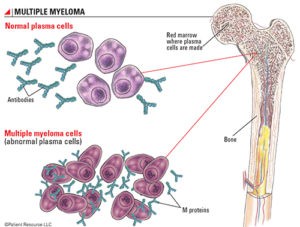
Steroid-induced shoulder avascular or osteonecrosis is one of a string of long-term and late stage side effects that occurred during the years after my conventional therapies following my multiple myeloma diagnosis in early 1994.
The irony of surviving multiple myeloma since early 1994 is having to deal with a litany of short, long-term and late stage side effects. Alopecia, fatigue and nausea were my introduction to chemotherapy.
But those adverse events pale in comparison to
- nerve damage (CIPN, RILP),
- brain damage (chemotherapy-induced cerebral dysfunction),
- heart damage (chemotherapy-induced cardiomyopathy)
- and the risk of secondary cancers.
If y0u are a MM patient or survivor or a cancer patient of any type, please, please, please undergo as little toxicity as possible. While your oncologist will offer the “standard-of-care” therapy plan, understand that there may be many therapies options to manage your cancer with little or no toxicity.
Going forward, what will I do? Steroid-induced shoulder avascular or osteonecrosis is percolating in both shoulders. I have pain but it is manageable. I will not undergo any form of toxic therapies at this point.
As far as I can decipher from the research linked below, Steroid-induced shoulder avascular or osteonecrosis is incurable and the conventional therapies suggested may not provide a solution for very long. Please read to the bottom of the post below.
To my way of thinking, if avascular, osteonecrosis is caused by lack of blood flow, my therapy to prevent collapse should be increasing blood flow to the area as fully, as often as possible.
The same daily, moderate exercise I do each and every morning to manage all of my other side effects is also essential now, for my steroid-induced shoulder avascular or osteonecrosis.
Further, the same bone building nutrition and supplementation that I have been taking and writing about on PBC for years now, is required for my steroid-induced shoulder avascular or osteonecrosis.
If you have steroid-induced shoulder/hip/ankle avascular or osteonecrosis, please scroll down the page to post your experience and questions to me.
To Learn More about Chronic Non-Cancer Pain- click now
I will post additional blogs if my situation changes.
David Emerson
- MM Survivor
- MM Cancer Coach
- Director PeopleBeatingCancer
Recommended Reading:
- Long-Term Multiple Myeloma Survivor- If I Knew Then What I Know Now
- Multiple Myeloma Diagnosis- Can’t Trust Conventional Cancer Research
- MGUS, SMM, Myeloma-Antioxidants in Food vs. Supplements
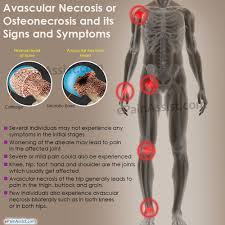
Avascular necrosis
“Avascular necrosis (AVN), also called osteonecrosis or bone infarction, is death of bone tissue due to interruption of the blood supply.[1] Early on, there may be no symptoms.[1] Gradually joint pain may develop which may limit the ability to move.[1] Complications may include collapse of the bone or nearby joint surface.[1]
Risk factors include bone fractures, joint dislocations, alcoholism, and the use of high-dose steroids.[1] The condition may also occur without any clear reason.[1] The most commonly affected bone is the femur.[1] Other relatively common sites include the upper arm bone, knee, shoulder, and ankle.[1]
Treatments may include medication, not walking on the affected leg, stretching, and surgery.[1] Most of the time surgery is eventually required and may include core decompression, osteotomy, bone grafts, or joint replacement.[1] About 15,000 cases occur per year in the United States.[4] People 30 to 50 years old are most commonly affected.[3]
Causes-
The main risk factors are…and the use of high-dose steroids.[1] Other risk factors include radiation therapy, chemotherapy, and organ transplantation.[1] Osteonecrosis is also associated with cancer…
Avascular Necrosis in the long-term Multiple Myeloma Survivor
“Hi David. I am an 18 year multiple myeloma survivor. I’ve had 2 autologous stem cell transplants. The last one I had was 6 years ago. A year ago March I was diagnosed with Avascular Necrosis in both hips…
Shoulder Osteonecrosis: Pathogenesis, Causes, Clinical Evaluation, Imaging, and Classification
“The humeral head (shoulder) is the second most common site for nontraumatic osteonecrosis after the femoral head, yet it has attracted relatively little attention. Osteonecrosis is associated with many conditions, such as traumatism, corticosteroid use, sickle cell disease, alcoholism, dysbarism (or caisson disease), and Gaucher’s disease. The diagnosis is clinical and radiographic with MRI, with radiographs being the basis for staging…
After the femoral head, the humeral head is the most frequent location for nontraumatic osteonecrosis 1 . This pathology is underestimated, and a proper clinical evaluation must be presented as knowledge for the orthopaedic surgeon.
In addition to post‐traumatic avascular osteonecrosis (AVN) 2 , causes of humeral head necrosis (Fig. (Fig.1)1)… and corticosteroid therapy 4 ; as a result, a large population of patients are at high risk for shoulder osteonecrosis…
Corticosteroids
Corticosteroids are a common cause of atraumatic humeral head necrosis, but the exact mechanism is unknown. Hernigou 4 evaluated the natural history and the rate of disease progression with a long‐term follow up.
The outcomes of 215 shoulders (125 adult patients) with osteonecrosis related to corticosteroids were evaluated at early stages before collapse with radiographs and MRI. With an average 15 years of follow up (range 10 to 20), there was pain in 65% of asymptomatic shoulders and collapse had occurred in 50% of shoulders. In symptomatic shoulders, collapse has developed in most at the final follow up. The time between the diagnosis and collapse was an average lof 6 years. At the most recent follow up (average 15 years), 50% of shoulders had required surgical treatment. Stage, occurrence of pain, and continuation of peak doses of corticosteroids were risk factors for progression of osteonecrosis.
The role of steroid dose remains controversial. Suspected as early as 1957 21 , whether this is a dose response, threshold, peak‐dose, or idiosyncratic phenomenon is unclear. The high dose of steroids during the first several weeks seems to be more important than the total cumulative dose. In addition, patients may have a predisposition toward osteonecrosis, with a possible genetic susceptibility for the disease.
The most commonly accepted theory surrounding corticosteroids and shoulder osteonecrosis involves fat accumulation in marrow (Fig. (Fig.4),4), leading to increased intraosseous hypertension and decreased blood flow.
This concept has been extrapolated 22 into a multiple‐hit theory in which corticosteroids alter bone homeostasis, injure bone cells, impair blood flow, and suppress bone cell precursors in susceptible patients. Corticosteroids inhibit angiogenesis and promote a hypercoagulable state, which could contribute to the formation of intravascular thrombosis…
Clinical Evaluation
Insidious pain with movement is frequent in nontraumatic necrosis of the humeral head. Pain at night is not frequent; however, in one study, 70% of patients had difficulty sleeping 35 . Symptoms may prevent physical work in up to 80% of patients. A “click accompanying certain movements” results from joint incongruity, cartilage flap, or a large loose body. Patients with osteonecrosis of the humeral head are usually younger than patients with osteoarthritis.
Physical examination may reveal tenderness, but motion is often preserved until the late stages. The discomfort is greater with the arm abducted or elevated 90°, corresponding to maximum glenohumeral loading.
Depending on the history, useful tests may include blood count, erythrocyte sedimentation rate, and C‐reactive protein to help rule out infection. Specific serology for rheumatoid arthritis is useful to rule out inflammatory conditions…
Imaging
MRI is the modality of choice for patients with a suspicious history, along with physical examination with examination of normal radiographs. The diagnosis of osteonecrosis on MRI was based on band‐like abnormal signals, and band‐like hypo‐intense zones on T1‐weighted images (Fig. (Fig.8).8). It is 99% sensitive and specific for detecting early shoulder osteonecrosis, which usually presents as an area of low‐intensity signal on T1‐weighted and high‐intensity signal onT2‐weighted images (Fig. (Fig.9).9). Bone marrow edema and a joint effusion may also be present. The later stages of shoulder osteonecrosis are better assessed using plain radiography and, in some cases, CT scans. CT scans are useful for evaluating patients with a suspected subchondral fracture, which may not be seen on MRI…
Treatment
Conservative treatment options are proposed and effective in patients with stage I and II osteonecrosis. Two types of core decompression have been described…
After collapse, the indication is usually an arthroplasty. Osteonecrosis as a surgical indication accounts for approximately 5% of all shoulder arthroplasties performed. However, relatively few studies have evaluated the outcomes following arthroplasty for osteonecrosis of the humeral head and many studies include only a few cases or have a short‐term follow‐up.
The decision to use hemi‐arthroplasty or a total shoulder arthroplasty is usually based on the glenoid status and the surgeon’s opinion. One absolute contraindication for arthroplasty is active infection, and relative contraindications include significant brachial plexus injury and concomitant deltoid and rotator cuff insufficiency, where a reverse shoulder arthroplasty can be proposed. The challenge when it comes to shoulder arthroplasty in patients with atraumatic osteonecrosis remains prosthesis longevity, as these patients are relatively young…”