“Most people with smoldering multiple myeloma eventually develop myeloma, which is why patients are closely monitored by their doctors.”
Most people with smoldering multiple myeloma progress to full-blowa MM. But not all people. Why would any SMM patient begin chemo if they didn’t have to? What is the benefit of beginning chemotherapy?
- Fact- SMM is not cancer. It is pre-cancer.
- Fact- SMM does increase the risk of myeloma but does not guarentee a multiple myeloma diagnosis.
- Fact-once a person begins chemotherapy, the multiple-drug resistence (MDR) clock starts ticking.
- Fact- chemotherapy is toxic. Toxicity means short, long-term and late stage side effects.

I’m pretty sure that the studies linked and excerpted below are factual. Chemotherapy will reduce a SMMer’s risk of progressing to frank multiple myeloma. For a time anyway. Not permanently.
Chemotherapy can increase a SMMer’s “progression-free survival.” Meaning, if a person is diagnosed with SMM, he/she might progress to MM. Chemotherapy probably will increase a high-risk SMM patient’s time before he/she is diagnosed with MM.
But the real question, in my opinion, is what will early chemotherapy do for overall survival (OS)? AKA length of life?
After reading and re-reading those articles below, the most important reason I can come up with in favor of beginning chemotherapy is that beginning chemotherapy now will probably result in a longer progression-free survival. And the drawbacks of chemotherapy are many.
The problem, as I see it, is that when a person is diagnosed with SMM, they cannot know if they will progress to full-blown MM. They probably will, but they might not. They might not have to endure the risks, the problems that come with chemotherapy.
Consider the evidence-based, non-toxic therapies shown to reduce your risk of a full-blown MM diagnosis.
I am a long-term survivor of multiple myeloma. I have undergone conventional, non-conventional, and alternative MM therapies. I have lived the good, the bad and the ugly that MM treatment has to offer.
Have you been diagnosed with smoldering multiple myeloma? Scroll down the page, post a question or comment and I will reply to you ASAP.
Thank you,
David Emerson
- MM Survivor
- MM Cancer Coach
- Director PeopleBeatingCancer
Recommended Reading:
“Patients with smoldering myeloma treated with Revlimid (lenalidomide) monotherapy achieved a statistically significant improvement in progression-free survival compared with those who were observed, according to preliminary findings of the ECOG E3A06 study.
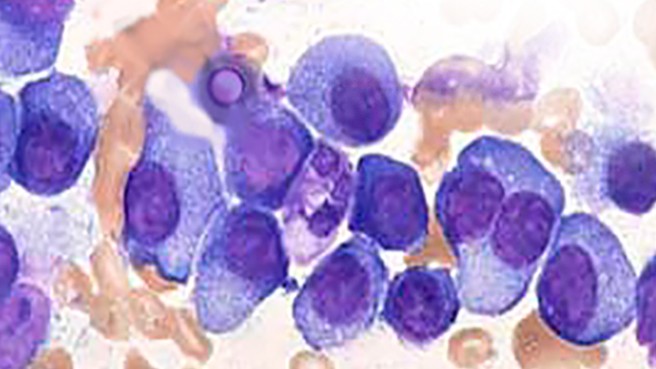
Smoldering multiple myeloma is an early precursor to multiple myeloma and produces certain proteins – measured in the blood and urine – that show up before a person has any symptoms. Most people with smoldering multiple myeloma eventually develop myeloma, which is why patients are closely monitored by their doctors.
“A portion of patients with smoldering myeloma do progress to clinical myeloma, which requires significantly more therapy,” Madhav Dhodapkar…
“It is very important for us to know if using Revlimid early on will actually prevent progression to clinical myeloma, and actually lead to improved outcomes. If it does, it will change the standard of care,” he added…
In the treatment arm, patients received Revlimid orally once daily on days one through 21 for every 28-day cycle until disease progression or unacceptable toxicity. The control arm underwent observation until progression to symptomatic myeloma.
Single-agent Revlimid demonstrated a significant improvement in progression-free survival (the time that a patient lives with the disease but it does not get worse) – the study’s primary endpoint – compared with observation. Secondary outcomes will include overall response rate, duration of response, overall survival and safety.
In addition, the safety profile appeared to be consistent with previous studies.
“In multiple myeloma, there has been an important question regarding the risks and benefits of treating patients with smoldering myeloma. We believe that the properties of Revlimid could play an important role in delaying the progression of smoldering myeloma into active myeloma,” Jay Backstrom, chief medical officer for Celgene, the agent’s manufactuere, said in a press release.
“Therapy consisting of elotuzumab plus lenalidomide and dexamethasone yielded a high response rate and demonstrated tolerability in patients with high-risk smoldering multiple myeloma…
Of note, patients previously treated for smoldering multiple myeloma were deemed eligible for study participation.
Before the intervention was started, Dr Ghobrial and colleagues took bone marrow samples from 32 of the patients for baseline assessment and whole exome sequencing of plasma cells. The primary end point of the study was progression-free survival (PFS) at 2-years…
At the point when these data were presented, 40 patients had completed 24 treatment cycles; 38 of these patients are being actively followed-up with, as 2 died during therapy. According to Dr Ghobrial and colleagues, there is no evidence of disease progression among these patients.
At a median follow-up of 29 months, the 2-year PFS was not reached. At 36-months, however, the 3-year PFS and event-free survival rates were 95% and 100%, respectively. The overall response rate was 84% and included:
- 3 (6%) patients with complete remission,
- 18 (37%) with very good partial responses,
- 20 (41%) with partial responses,
- 5 (10%) with minimal response, and
- 3 (6%) with stable disease.
Using fluorescence in situ hybridization (FISH), Dr Ghobrial and colleagues identified 20 (40%) patients with high-risk cytogenetics, defined by the presence of del17p, t(4;14), and gain 1q.
“Interestingly, in 6 patients, high-risk SCNAs (1q gain and 17p deletion) were not reported in iFISH but were detected by whole exome sequencing. The analysis of these 32 samples showed that patients who are harboring mutations in the DNA repair pathway genes, had modest response to treatment,” Dr Ghobrial and colleagues explained.
Adverse events most frequently reported in the study included fatigue (92%), diarrhea (72%), and hyperglycemia (62%). The most common adverse events grade ≥3 were hypophosphatemia (34%), neutropenia (26%), and lymphocytopenia (22%).
Although no patients were reported as having disease progression to overt multiple myeloma, the small patient cohort and lack of a comparator arm prompt the need for further research of this combination in larger settings.
“The combination of elotuzumab, lenalidomide, and dexamethasone is well tolerated and demonstrates a high response rate with no progression to overt MM [multiple myeloma] to date,” Dr Ghobrial and colleagues said.
“Correlation with genomic studies can help define patients who benefit the most from this early therapeutic intervention,” they concluded.—Hina Khaliq”