
Diagnosed with Cancer? Your two greatest challenges are understanding cancer and understanding possible side effects from chemo and radiation. Knowledge is Power!
Learn about conventional, complementary, and integrative therapies.
Dealing with treatment side effects? Learn about evidence-based therapies to alleviate your symptoms.
Click the orange button to the right to learn more.
Breast Cancer Risk Scores
Determining breast cancer risk is important information for women. However, breast cancer risk scores have pros and cons that should be understood by women.
Olivia Munn gives the perfect direction in the article linked and excerpted below- “Ask your doctor to calculate your Breast Cancer Risk Assessment Score,”
Like just about every kind of medical information, there are pros and cons to understand.
What are the pros and cons of breast cancer risk scores?
Pros:
- Early Detection: Risk scores can help identify individuals at higher risk of developing breast cancer, allowing for earlier screening and preventive measures. Early detection often leads to better outcomes.
- Personalized Medicine: These scores allow for a more personalized approach to healthcare. By assessing an individual’s unique risk factors, doctors can tailor screening and prevention strategies to suit their needs.
- Resource Allocation: Risk scores can help healthcare systems allocate resources more efficiently by focusing screening efforts on those at higher risk, potentially reducing unnecessary procedures for low-risk individuals.
- Patient Awareness: Providing patients with information about their breast cancer risk can empower them to make informed decisions about their health, including lifestyle changes and screening options.
- Research Advancements: Utilizing risk scores in research can help identify new risk factors and improve our understanding of breast cancer, leading to advancements in prevention, diagnosis, and treatment.
Cons:
- Limited Accuracy: Risk scores are based on statistical models and may not accurately predict an individual’s actual risk. False positives and false negatives can occur, leading to unnecessary worry or missed diagnoses.
- Incomplete Data: Risk scores rely on available data, which may not capture all relevant risk factors. This can lead to underestimation or overestimation of risk in certain populations.
- Ethical Concerns: There are ethical considerations surrounding the use of risk scores, particularly regarding privacy, consent, and potential discrimination based on genetic or other risk factors.
- Cost and Accessibility: Some risk assessment tools may be costly or require specialized expertise to administer, limiting their accessibility to certain populations.
- Psychological Impact: Learning about one’s increased risk of breast cancer can cause anxiety and distress, particularly if there are limited options for reducing that risk or if the individual feels stigmatized due to their risk profile.
I am a long-term cancer survivor. I am biased of course but I think everyone should take basic, inexpensive steps to reduce their risk of cancer. Basic, inexpensive therapies such as:
- Clean nutrition- (I recommend the Mediterranean Diet)
- Nutritional supplementation
- Daily moderate exercise
- Little alcohol, no tobacco
- and more
Are you considering asking your doctor to calculate your breast cancer risk score? If you would like to learn more about breast cancer therapies- both conventional and evidence-based non-conventional therapies, send me an email David.PeopleBeatingCancer@gmail.com
Good luck,
David Emerson
- Cancer Survivor
- Cancer Coach
- Director PeopleBeatingCancer
What a Breast Cancer Risk Calculator Can and Can’t Tell You
“The actress Olivia Munn credited a simple tool with helping her doctor catch the disease early. But experts cautioned that it can’t give you the full picture…
“Ask your doctor to calculate your Breast Cancer Risk Assessment Score,” Ms. Munn urged the public in her post…
What do breast cancer risk calculators take into consideration?
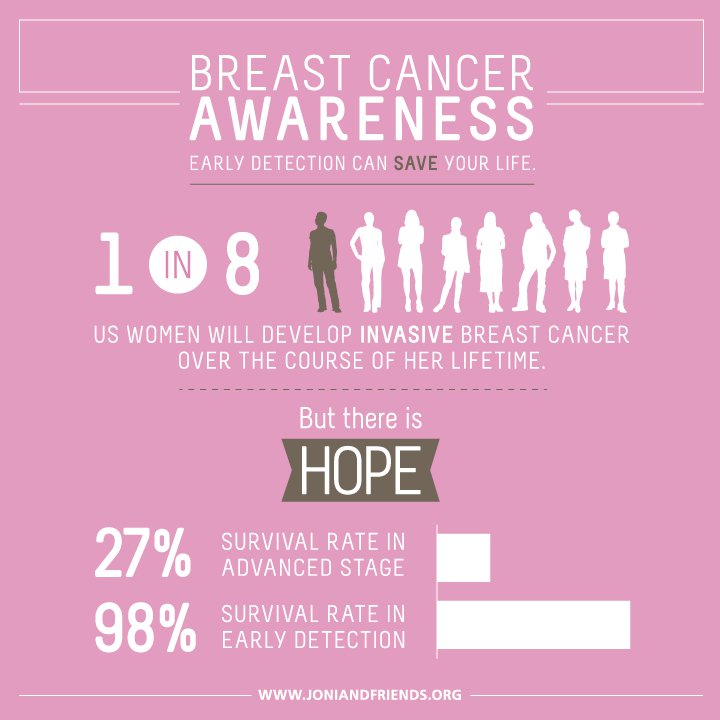
About one in eight women will develop breast cancer in her lifetime. But tools like the one Ms. Munn’s doctor used can offer a more personalized picture of an individual patient’s risk…
There are two main calculators: the Breast Cancer Risk Assessment Tool, also known as the Gail model, and the Tyrer-Cuzick Risk Assessment Calculator, also called the IBIS model. Both ask users their age, race, ethnicity, family history of breast cancer, when they first started their periods, and, if they have children, how old they were when they had their first child. All of these factors can influence a person’s risk of breast cancer…
The calculators compare a person’s answers with the average for other women from the same age and racial group, and use that to estimate five-year risk and lifetime risk of developing breast cancer…
The Gail model cannot accurately calculate risk for women with a history of invasive breast cancer or ductal carcinoma in situ or those with mutations in the BRCA1 or BRCA2 genes, which raise the risk of breast cancer, said Dr. Sandhya Pruthi, a breast medicine specialist the Mayo Clinic Comprehensive Cancer Center. Accuracy can also vary for different racial groups…
According to the National Cancer Institute, the Gail calculator may underestimate risk in Black women with previous biopsies and Hispanic women born outside the United States. It may also be inaccurate for American Indian or Alaska Native women, because data about their risks is limited…
It’s also essential to make sure that you understand the data required to answer the questionnaires and input it correctly, Dr. Pruthi said. Even small changes in the answers can yield vastly different risk scores. And experts noted that these calculators should be used as part of more comprehensive care, including regular doctor appointments and recommended screenings such as mammograms. They can also be useful for women who aren’t yet old enough to have routine mammograms…
Knowing your risk estimate can help you and your doctor discuss whether you might need more frequent mammograms or genetic testing, or whether certain preventive steps might help lower your risk…
“If you are high risk, we actually can do something about that,” she added. Doctors may recommend that women with a high score make certain lifestyle changes — such as exercising more, cutting back on smoking and reducing alcohol intake — or that those with a high five-year risk take medications that can help reduce the likelihood of breast cancer…
However, doctors caution that interpreting your score can be difficult on your own. The difference between the five-year risk score and lifetime risk, in particular, can be hard to understand, Dr. Brawley said…
A risk score can’t determine whether a person will or won’t develop breast cancer. And it doesn’t say anything about your chances of dying from the disease, Dr. Woloshin said…


