Leave a Comment:
412 comments
I am not sure where to find your two free guides. It says to scroll down to receive them but nothing is there. Can you please send me the link to the guides? Thanks.
ReplyHi Joan-
Our free info is linked here-
https://peoplebeatingcancer.org/cancer-resources/
David Emerson
Reply[…] Multiple Myeloma Survivor- A Different kind of Second Opinion- […]
ReplyHi,
1. What conventional treatments did you receive? Duration of remission, if applicable?
2. What unconventional treatments did you undergo? Were they simultaneous to conventional?
3. What can you advise and/or inform someone diagnosed with Smoldering Myeloma (With HIGH LAMBDA Free Light Chain) six months ago at age 72, who is currently only on watch every three to four months?
Hi Barbara-
I underwent induction therapy of vincristine, adiamycin and dexamethasone in 1995. I then underwent two courses of cytoxan followed by an autologous stem cells transplant. I underwent local radiation before and after the above chemo.
In September of ’97 I was end-stage, told nothing more could be done. I then began antineoplaston therapy from the Burzynski Research Institute in Houston, TX.
Depending on your other risk factors, a lambda FLC that is above the normal range does not mean high risk. Meaning the SMM patient with normal risk can live with SMM for years and not progress to full MM. At 72 I would recommend non-toxic therapies, pre-habilitation, clean living, etc. etc. in an effort to achieve quality of life.
It is certainly difficult to live with MM hanging over the SMM patient’s head. The key is to focus on pre-habilitation to reduce the risk of a mm diagnosis and at the same time condition the SMM patient to respond better to moderate induction if it is ever needed.
Let me know if you have any questions.
Hang in there Barbara,
David Emerson
ReplyHi David,
I am just about to get my biopsy and the doctor wants an MRI. Actually he wanted a PET scan but I said MRI. I just found out there is something called a “whole body MRI scan” I am finding out if that is what the doctor ordered but I think not. I think the whole body MRI scan is a newer product that people are buying proactively because it can detect cancer early in many of the body organs. So I think I will get this type of MRI. Do you have opinions on this whole body MRI? Also, when does one get their second opinion? After the first doctor has given their diagnosis and treatment plan or before that?
[…] To Learn More About the Importance of a Second Opinion- click now […]
Reply[…] To Learn More About the Importance of a Second Opinion- click now […]
Reply[…] To Learn More About the Importance of a Second Opinion- click now […]
Reply[…] To Learn More About the Importance of a Second Opinion- click now […]
ReplyI was diagnosed with mm, in 2018, and have had three hemp/oncologist, since . I.am
A 77 year old female, now being treated at UNMCC,, and still trying out different treatments.
Hi Mary-
I am sorry to learn of your myeloma diagnosis. Breaking in one oncologist is difficult enough. Breaking in three in a four year period would be above and beyond the call of duty.
Those myeloma patients over the age of 75 are considered to be elderly and therefore should be treated differently than the average myeloma patient.
Let me know if you have any questions. Hang in there,
David Emerson
ReplyHi David,
Thanks for sharing so much great information. I am MM patient diagnosed in November 2021. I have been on induction now for 8 cycles and have decided not to do the transplant. It has been a difficult decision as there is a lot of various opinions from different Myeloma specialists. My local oncologists said no transplant and my Myeloma specialist said Transplant was a must for PFS. I am 63 and he thinks because I am considered young it is the best way to go. I recently got a 3rd opinion for a highly respected specialist who is doing a lot of cutting edge research in the Myeloma field and he said no transplant. It has been very confusing. I am doing really well with little to no side effects from treatment. I would be very interested in your nutrition guide to help me learn more about eating right. Thanks
Replymy son recently was diagnosed with MM and I am advocate of holistic help for him and myself and would like to know what suppliments are good to ad to his chemo. he is taking velcade and I am good with curcumin. what other ones would be useful to add to his regime. It sounds like he will be getting low doses for the next 4 weeks and if that works he would move to once a month. otherwise, they felt it would be needed another month.
ReplyHi Dennis-
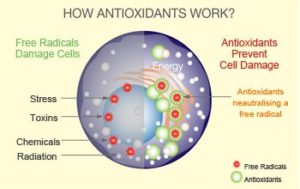
I am sorry that your son has been diagnosed with MM. Research has shown curcumin’s ability to enhance the efficacy of Velcade/bortezomib. See the study linked below. Depending on what other chemotherapy regimens your son is undergoing, there will be other supplements what, according to research, will act synergistically with his chemotherapy regimens.
All to say, in order go recommend anti-mm nutrition, integrative or complementary supplementation and anti-mm lifestyle therapies, I would need to know your son’s
MM stage at diagnosis (I,II,III)
Symptoms (bone, nerve pain, hyper viscosity, etc.)
Age
Goals, etc.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3344248/
Consider finding and working with a MM specialist rather than a general oncologist or hematologist/oncologist. Consider both the cure vs. control side of the treatment debate discussed below.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3923461/
Depending on your son’s age, your overall survival goals may be long-term.
Let me know if you have any questions. Good luck.
David Emerson
Reply[…] Multiple Myeloma Survivor- A Different kind of Second Opinion- […]
ReplyHi, I have not been diagnosed, but suspect. How do I get this “second opinion?”
ReplyHi Rachel,
I am a different kind of second opinion. I represent a long-term MM survivor’s perspective. Understand that formal diagnostic testing is the only way to get a diagnosis of MM that your health insurance, for example, will accept.
But I can help with a basic understanding of your symptoms such as bone pain or kidney involvement.
Why do you “suspect” you have MM?
David Emerson
ReplyHello David,
My name is Arnold Venti. I was diagnosed in August 2021 with stage 2 MM. I just recently joined your coaching course on MM & my wife & I are impressed with the amount of time & effort you have given to helping others survive as you have.
I have completed the first phase of induction treatment (RVD) and got my M-Spike down to .28, putting me in “good partial remission.” On Dec. 16, I started the ASCT process, first with Zarxio injections, then adding Mozobil. But after 2 days of stem cell collection, I could only produce 300,000, with the goal being 4-5 million. The transplant was aborted and I was given a month off, which is about to come to an end. The docs want me to try again, but I feel I have several strikes against me. 1) my age – 76; 2) the harshness of the treatment itself, then short & long-term side effects, especially zero immunity; 3) the danger of Covid & other viruses.
Currently I am being treated at UCSD in La Jolla. In a few days, I will have a meeting with an oncologist at Scripps/MD Anderson, also in La Jolla, for a 2nd opinion. Thanks for the info about what to ask at such a meeting.
In your opinion, is the ASCT the ONLY way to put my MM in long-term remission, or are there other good options to ask about when we meet with either my present oncologist or the 2nd opinion doc.
Thanks very much. Looking forward to hearing from you.
Hi Arnold-
I responded directly to you via your email address.
Thanks,
David Emerson
ReplyDo you consider massage therapy as an evidence based option for reducing side effects in MM patients?
ReplyHi Lori-
Personal experience as well as studies confirm that massage helps relieve pain. Be careful as to what type of pain- bone, joint or muscle.
David
ReplyI’m helping a friend find some natural cures for her multiple myeloma since she has to take the chemo treatments per her insurance. Some of the drugs she is taking seem pretty severe in the side effects they can cause. She is taking Remlevid, dexamethasone, Decadron, and valcade (bortezomib). She was told at first that she was in Stage1 with a year life expectancy but this does not add up for me. I’m thinking with a year, she is in late stage 2 or stage 3. I’ve told her about the sodium bicarbonate treatment and juicing, taking vitamin C (she doesn’t have access to IV Vitamin C), and wasn’t sure if she could take latrile with these meds or not. Not sure if she can take tumeric with these meds either. I don’t want to tell her about them until I know more of how they will react with her chemo drugs. Can you give me any info on this? Thanks so much!
ReplyHi Sarah,
You’ve mentioned several different areas of possible therapies for your friend. By “areas” I mean dosing as it relates to her stage, integrative therapies shown to enhance the efficacy of her chemo (curcumin has been shown to enhance the efficacy of velcade/bortezomib) and finally, a big issue is that of natural cure- MM is considered to be incurable. The longest living MM survivors I know of combine low-dose chemo with integrative or complementary therapies.
I will send the nutrition guide and the supplementation guide to your email address. The info in these guides should give you both some guidance going forward.
Hang in there,
David Emerson
ReplyI paid $198.00 and have not received the books 787-462-5156
Replygreat website – thanks. I am 68 and lived a lifestyle since the age of 17 that matches your recommendations. healthy, organic diet, no meat, nothing processed or with chemicals, vigorous exercise, close relationships with wonderful caring friends, a career that I love and regular supplements including CBD for the past 2-3 years. dx with MM 1 week ago. what a blow !
ReplyDear Mr. Emerson,
My name is Kristina Morgan R.N. M.S.N. I am working as a pro-bono advocate for a patient who has been diagnosed with MM, second diagnosis by UCSD. She is adamant about not receiving traditional therapy and she has been utilizing alternative vitamin and herbal remedies.. She has had 3 blood transfusions within the last 6 months. Her labs are not good. I have been in contact with the BMT Team at UCSD. Her oncologist is extremely concerned as I am about her labs. She asked me to contact you. I referred her to the ER 2 nights ago secondary to extreme chest pain which did not result in an emboli diagnosis. She refuses to allow me to contact her oncologist about this last incident. She has viewed your website and has requested I reach out to you. At this point I am extremely concerned. I am not against alternative treatments. However, I believe in the future she may go hat route. As I see it she needs chemo asap.. She does not want to take
chemo and she has no-one in this area to care for her.. I totally understand how she feels. Therefore, I am respectfully reaching out to you for any recommendations from your experience.
If you should wish to contact me, my cell no is 760-518-1171. Thank you in advance for your assistance/guidance in this matter.
Kristina
ReplyHi Kristina-
I am sorry to learn about the MM patient. While I am the first person to question toxic MM therapies, even I admit that all MM patients with advanced MM (stage 2 or 3) must undergo chemotherapy to bring their MM under control. RVD is the SOC induction therapy and has proven to be remarkable for newly diagnosed MM patients.
If I were to speak to the MM patient I would recommend pre-habilitating her MM and then discuss possible integrative therapies to take WITH her induction chemotherapy (RVD).
I would caution against an autologous stem cell transplant, depending on her diagnosis.
I am telling the above to give you the basic info I would give if I were to talk with this person sometime.
Let me know if you would like me to speak to this person on the phone.
Thank you,
David Emerson
ReplyHello David where can I find the anti-cancer diet. thanks Gerardine
ReplyHi Gerardine- The “nutrition guide” in the MM CC program cites specific anti-MM foods and supplements. I encourage
you to watch the video of the Ted Talk given by Dr. William Li as he talks about anti-angiogenic foods.
David
Reply1. on March, 2020, I was diagnosed with Smouldering Myeloma which should to be monitored on a 3to 6 months basis. No lytic lesions on CT and Bone marrow showed good preservation of normal hematopoiesis , albeit with a 10-20% plasma infiltrate. IgG = 26.9 g/L, Abnormal Band= 19g/L, IgG Kappa paraprotein 19g/L. Kappa Free light Chains= 479. K/L ratio = 43.55, Hemoglobin = 140g/L
2. Monitoring on 16.06.2020. – IgG= 29.3g/L, Abnormal Band = 22g/L, Kappa free light trains= 575, K/L ratio= 57.5, B2M= 2.57 mg/L, Hemoglobin= 138g/L, LDH= 211U/L
3. Monitoring on 03.10.2020: IgG=33.2g/L, Abnormal Band= 30.9g/L, Kappa free light trains= 864, K/L ratio= 97.07, B2M= 2.252, Hemoglobin= 114, Gamma=34.7g/L, LDH= 569 U/L, Creatine = 106.08umol/L. ESR=42mm/h.
I was started giving treatments on18.10.2020 as follows:
Cycle No.1:
First (01st) Cycle Day 1
Zoledronic Acid 4mg
Dexamethasone 20mg
INJ Bortezomib 2mg
Thalidomide 50 mg (will be given orally) Once a day
Day 2
(after 4 days) 1.INJ Bortezomib 2 mg
2. Dexamethasone 20 mg (will be given orally)
3. Thalidomide 50 mg (will be given orally)
Day 3 (After 4 days) INJ Bortezomib 2mg
2. Dexamethasone 20 mg (will be given orally)
3. Thalidomide 50 mg (will be given orally)
Day 4 (After 4 days) INJ Bortezomib 2mg
2. Dexamethasone 20 mg (will be given orally)
3. Thalidomide 50 mg (will be given orally)
2nd, 3rd, and 4th Cycles will be repeated mostly in the same way. There will be a gap of 21 days between each cycle.
Would you please tell me I am in What stage of SMM or MM? Why such a big jump in between 2nd 3rd monitoring? I am 72 years old.
Appreciate, very much if you guide me accordingly. Thanks lot’
ReplyI have considered joining your program, but one of the things holding me back relates to age. The people I see like you who go into remission for 20+ years are generally diagnosed in their 40s or younger. I was diagnosed at 67, and just turned 68. Do you have evidence that your program contributes substantially to longevity for those like myself who are diagnosed at more advanced ages? Most folks in my family lived into their 90s. I have no comorbidities. I am also an avid researcher, and disciplined at following protocol, with the exception of those times I am nauseated from the Velcade. During those times, I don’t do bad things, I just am not able to do all the good things. Thank you in advance for your response.
ReplyHi Cathy,
Thanks for reaching out. The average age of the newly diagnosed MM patients is 69 according to the American Cancer Society. The ages of MM CC clients, as far as I can tell, spreads from 40’s,50’s,60’s,70’s,80’s and even a pre-mm client in his 90’s. It sounds like you are heading in the right direction. Good luck.
David Emerson
ReplyDear David,
Are you familiar with light chains myeloma? It is one of the types of aggressive MM which about 15% of MM patients have. While the evidence-based nutrition, supplementation and lifestyle therapies appear to benefit MM patients, will the described evidence-based therapies help those who have a free light chain disease such as aggressive light chains myeloma?
Thank you for your response.
ReplyHi Ronald,
I will reply to your post directly via email. Thanks.
David Emerson
Reply[…] Multiple Myeloma Survivor- A Different kind of Second Opinion- […]
Reply[…] Multiple Myeloma Survivor- A Different kind of Second Opinion- […]
Reply[…] A Different kind of Second Opinion-Multiple Myeloma Cancer Coaching […]
Reply[…] A Different kind of Second Opinion-Multiple Myeloma Cancer Coaching […]
Reply[…] A Different kind of Second Opinion-Multiple Myeloma Cancer Coaching […]
Reply[…] A Different kind of Second Opinion-Multiple Myeloma Cancer Coaching Multiple Myeloma: Car-T Cell Immunotherapy Update David Emerson: Multiple Myeloma Survivor Since 3/94 My Multipe Myeloma journey: I started getting MM symptoms 4 years prior to CAR-T and was diagnosed two years ago. I refused stem cell transplantation and initially opted for Velcade, Revlimid, Dexamethason of which I did 6 cycles or 24 infusions. I was refractory to the treatment. I then started on Daratumumab (CD 38 marker) weekly for 8 weeks and bi-monthly for 2 months and very quickly got good results but hit a barrier beyond which no further improvements were made. The doctor was unable to explain why. The answer became apparent once I started CAR-T preparations when my bone marrow results showed that I was negative for CD38 marker, meaning that Daratumumab had worked perfectly. The problem was that I had other MM strains which didn’t carry the CD38 marker. MM is not a homogeneous cancer. After two years of taking 4mg weekly of Dexamethasone and almost daily Lenalidomide alongside loads of secondary meds and treatment drugs, I suffered many side effects such as corneal toxicity (my eye sight is only just starting to recover) and ear ringing (temporary). Dexamethasone in particular is a nasty steroid that not only causes violent mood swings, difficulty in mental focusing and insomnia but also painful swelling of the stomach. My most severe side effect has been memory impairment or chemo brain. I still find it hard to recover short to medium term memory or vocabulary words, although it is slowly improving. Remembering names and events is sometimes a challenge. I also note a distinct dimness and slowness in my mental faculties, hopefully this will also be temporary in nature. The CAR-T treatment took place in the following way: […]
Reply[…] A Different kind of Second Opinion-Multiple Myeloma Cancer Coaching […]
Reply[…] A Different kind of Second Opinion-Multiple Myeloma Cancer Coaching […]
Reply[…] A Different kind of Second Opinion-Multiple Myeloma Cancer Coaching […]
Reply[…] A Different kind of Second Opinion-Multiple Myeloma Cancer Coaching […]
Reply[…] A Different kind of Second Opinion-Multiple Myeloma Cancer Coaching […]
Reply[…] A Different kind of Second Opinion-Multiple Myeloma Cancer Coaching […]
ReplyI think you are wrong about sugar. I am receiving immunotherapy for my MM and I have Krispy Kreme donuts after every infusion. My M-protein is zero. Gina
ReplyHi Gina,
I’m not sure what you mean about being wrong about sugar. While I and many studies encourage reducing sugar I don’t believe that anyone can totally eliminate all sugar from their diet. Regarding a donut after every infusion, my guess is that the mind-body benefits of a donut outweigh the negatives regarding sugar:-)
I would add fruits and veggies to your diet however. MM is a marathon not a race. Congrats on an M-spike of zero.
thanks
David Emerson
Reply[…] A Different kind of Second Opinion-Multiple Myeloma Cancer Coaching […]
Reply[…] Multiple Myeloma Cancer Coaching- Getting a Different kind of Second Opinion […]
ReplyI see you don’t monetize your website, don’t waste your traffic, you can earn additional bucks every
month because you’ve got high quality content. If you
want to know how to make extra $$$, search for: Boorfe’s tips best adsense
alternative
My father has a large lump on his neck and he will not go to the doctor but i am pretty sure it is cancer of his lymph node. I have tried to get his to at least start taking some natural things like Teas and hash oil topically…. is there any advice you can give me to pass on to him about types of treatments and or things he could try at home?
I have read that taking alkaline things can stop cancer growth…. any suggestions might help.
ReplyHi Tara-
The key to your father’s quality and quantify of life going forward is a function of him getting a diagnosis for his neck. Please tell your dad that he does NOT have to do anything that his doctor tells him. Your dad is simply trying to figure out what the lumps are.
Good luck,
David Emerson
ReplyMy mom had breast cancer, stage 2, estrogen positive and her (+), in 2000 which she underwent chemo for and one of the chemo’s damaged her heart.
Two weeks ago she was diagnosed w/ liver and bone cancer. The biopsy shows it is the return of the breast cancer…. estrogen positive but this time her (-).
I would like to research natural/alternative healing vs. chemo. I can’t find any places in central TX anywhere online that treat other than w/ chemo as the main treatment.
Any suggestions on possible treatments to look into or doctors/practitioners, etc. would be greatly appreciated!!
ReplyHi Leslie-
I am sorry to read of your mom’s BC relapse. I want to understand your situation clearly. Are you saying that your mom’s breast cancer, first diagnosed in 2000 has metastasized to her bones and liver?
I am asking as my recommendations for therapies vary depending on the survivor’s situation.
Let me know and we can discuss therapy specifics.
David Emerson
ReplyMy mom went through a similar experience and she too healed herself through a natural process by an herbalist she got in contact with.
.She had dysplaysia and detrimental cancer stage 3c. Here she is a year later and she is cancer free. It was a lot of work taking those herbs but she did it without chem. Her Dr told her she’d be dead in a year, well with chemo she probably would have. Fight the fight and keep on fighting. still have the contact of herbal Dr if you want to give it a try. Blessings.
Hi Valerie-
Thanks very much for your story. Do you remember what herbs your mom took?
David Emerson
MM Survivor
MM Cancer Coach
I’ve had a reaccurence of lobular breast cancer. I am trying to avoid chemo and radiation. I had a nightmare experience with this last surgeon, which caused another tumor to appear within 6 weeks. I am using Aztec indian healing clay. This seems to make the area feel very sore. I had a biopsy on it 4 days ago. Could this be the reason for the pain. Could this be that its pulling out toxin? should I continue using the clay. Would it be possible to reply on my email? Presently, also, I am doing parts of the Gerson Institute program and taking Poly MVA. Bekk
Reply[…] Whether you want a different kind of “second opinion,” you are newly diagnosed, have just finished induction-therapy, have just come out of remission, or you want to learn about palliative or hospice care, you may want to talk to a long-term cancer survivor who has been researching cancer issues since 1997. […]
ReplyHI David,
I had a bilateral mastectomy Nov 25, it has been a roller coaster ride but I am feeling almost like myself now. Still waiting for incisions to heal they had to open me back up a couple of weeks ago and cut away dead tissue and relieve all the fluid in there. Much better though. I did have the Onca DX test and it came bake only 1% difference for re occurrence if I did the chemo with the hormone therapy. I did take the hormone therapy but turned down the chemo ( I am soon to be 59), my surgeons are ok with it but the onocologist insisted I need chemo, I still said no. Today I am going to talk to the radiologist because a couple of specs were seen in the lymph nodes. What are your thoughts/suggestions on this???
Hi Debbie-
Thank you for reaching out. I am sorry to read of your BC diagnosis though it sounds as if you are doing as well as can be expected. If I understand your post correctly, you underwent the Oncotype DX Breast Cancer Recurrence Score and “came back only 1% difference for recurrence.” I take you to mean that your chance of BC relapse is only 1%. Are you saying that Oncotype is only accurate if you have chemotherapy too? If you underwent a double mastectomy and if you underwent hormone therapy you will reduce your risk of relapse.
In answer to your question, “What are your thoughts/suggestions on this???” You must ask your oncologist if chemotherapy and or radiation will FURTHER reduce your risk of relapse that offsets your increased risk of side effects and secondary cancer. In other words, will chemo and or radiation be worth it to you?
My personal belief is that conventional oncology minimizes the risks of chemo and radiation. However I don’t know enough about your particular situation to advise you one way or another.
If your oncologist “insisted I need chemo” ask him/her to be specific. Will the benefits outweigh the risks?
Let me know if you have any questions.
David Emerson
ReplyThis is a great site. I did not read all of it but what I did makes lot of sence.
ReplyI have been diagnosed with an aggressive Lymphoma cancer based on pathology report on excised tumor removed from lacrimal gland. Have just went through PET, MUGA, Bone marrow extraction and MRI of brain and Eye sockets. I am totally against Chemo and oncologist says I can not survive without it. Are there other alternatives out there to consider. Any questions I need to ask Oncologist to get a better idea of what exactly is going on?
ReplyHi Lori-
I am sorry to read of your lymphoma diagnosis. Your therapy plan will depend largely on your specific stage at diagnosis. Meaning, what specific type of lymphoma have you been diagnosed with? And then what stage of that specific type of lymphoma? While there are many evidence-based types of therapies for you to consider, your challenge will be to find those therapies that research shows can produce a remission or a cure.
I can give you more info based on your type and stage of lymphoma.
Hang in there,
David Emerson
ReplyHello David :
at age 51,2002 diagnose Prostate Cancer. They removed the Prostate,(2003) a nick off the bladder, bed of the Prostate and the\Seminal Glands, along with some “other’ soft tissue. O.R. time involved, 10.5hrs. My Gleason was a score of 8 at the time. Two years later,(2006) 39treatments of Radiation.
2009 left Kidney removed, save the Adrenal Gland
Jan 2016 my PSA was 5.9 so March saw the start of Hormone Therapy. I got my first shot March, shot two June and at that shot Chemo Pills was brought up…but I told them I’m riding my bike to L.A., Cal., come mid July….felt I didnt have room on my bike for them…they are not happy, then my third shot was Sept and they were even LESS happy when I told them that shot was my last……freaking side effects I can tell ya. Sept PSA was .057. So I’ve decided to stop the Hormone Therapy…..at least until the PSA gets to a 6 or so ? Maybe ?
My Prostate was NOT saturated. It had cancer only but on one half of the gland. Eight samples were taken from the gland, 3were cancer. Yet every thing around and away from my Prostate was cancer, like my Sem Glands, the bed of, well….. you get the drift here right ?
Question : is it possible……the cancer started in my back area and traveled TO my Prostate ? Because……every one at the hospital I knew who had the very same as me, RE: Gleason Score our PSA’s….. are all gone now. In my class if you would, I’m the only one left, and the doctors are very surprised I’m 5yrs to the good at this point. I’m still working full time by the way, self employed, K ? 17,000K’s in less than 3weeks, on my Motorcycle in July/Aug
So ya Eh ? have you heard or talked to other guys who thought their cancer may have started else where first THEN moved into the Prostate ?
So there ya have me question Eh ?
ReplyHi Fraser-
I am sorry to read of all of your PCa challenges. To be honest, I am not qualified to offer comment on your question “? have you heard or talked to other guys who thought their cancer may have started else where first THEN moved into the Prostate?” Your situation is intricate. Conventional oncology should be able to look at your health history and offer more information.
Hang in there,
David Emerson
ReplyHello,
My good friend has cancer in the stomach, liver and bones. She had her ovaries removed because they had tumors. She is taking Traditional Chinese Medicine for this and Peruvian herbs. She is considering taking colloidal silver and B17. Is this a good idea? Is there anything else she can do? She is done with chemotherapy, it has poisoned her completely and the doctors tell her she is going to die.
She has four small children and her husband is hospitalized after surgery due to cancer as well. We desperately want her to survive!
Thanks,
Mariola
Hi Mariola-
I am sorry to read of your friend’s stomach cancer that has metastasized to her liver and bones. Re your question ” Is there anything else she can do?” Yes, but at this point your decision-making is difficult as there is little if any available research to support non-conventional therapies.
Your friend’s cancer is advanced. There are non-conventional therapies such as nutrition, supplementation, etc. Let me know if you would like additional research done on the available non-conventional therapies.
David Emerson
Cancer Survivor
Cancer Coach
I have recently been diagnosed with prostate cancer. I am at a loss as to which treatment to chose. My first instinct is to remove it, get rid of it…..surgery. I have been given the option of full radiation over 34-36 treatments or Brachytherapy with 15 treatments of radiation. I am overwhelmed at what choice to make. Surgery could involve incontinence etc. and of course an incision and longer recovery time. I will need three injections of hormone treatments before brachytherapy but it is less invasive to my body and has less side effects. Of course my one and only concern is making it go away. I don’t know which way to turn. I am 66 years old no in mid range of severity.
ReplyHi Keith-
I am sorry to read of your prostate cancer diagnosis. I understand being challenged by a dizzying array of therapy choices each with their own risk/reward or pro/con trade-offs. Keep in mind that there are evidence-based non-conventional therapies for each of the conventional therapies that you mention that may reduce your risk of side effects.
Meaning, for example, there are therapies for you to undergo with radiation that will reduce your risk of collateral damage. In addition, I encourage you to add evidence-based, anti-prostate cancer nutrition, supplementation, bone health and lifestyle therapies to your regimen.
I am both a cancer survivor and cancer coach. I work with cancer patients to research and design programs to manage their cancer based on their goals. You are relatively young as PCa patients go. You should be able to manage your cancer for years to come with minimal side effects.
What are your PSA and Gleason scores? Have you been given a stage?
Hang in there,
David Emerson
ReplyI was diagnosed with DCIS, stage 0. Don’t know which type yet. I have an appointment to speak with the surgeon tomorrow but this is frustrating because some say it’s abnormal cells that MAY become cancer and others day its precancerous. I Changed my diet and began exercising immediately. I’ve lost 10 pounds in 11 days. Not sure if surgery is the right things for this as it’s not really cancer and unnecessary surgery has its own side effects. Any information in this? Thx so much!
ReplyHi Tanya-
I apologize for the slow reply. Major holidays slow my cancer coaching.
I am sorry to read of your DCIS. Keep in mind that many consider a diagnosis of DCIS to NOT be cancer but a sort of PRE-cancer. First and foremost you should know that you have already reduced your risk of a full BC diagnosis by changing your diet, exercising and losing 10 pounds. A growing number of studies document frequent, modest exercise and weight loss to be effective therapies for BC.
Regarding surgery. You are correct when you say that surgery has it’s own side effects. Any therapy after a diagnosis of DCIS should be able to slightly reduce your risk of BC. Slightly. Many women have a lumpectomy after a DCIS diagnosis. It is an open question as to whether further therapy will improve your risk/reward outcome.
Let me know if you have any questions.
David Emerson
ReplyHi David,
My Dad is 75 and was recently diagnosed with Stage 2 esophageal cancer. I am interested in any information you can offer as to maximizing his treatment. He is meeting his oncologist tomorrow and the plan is chemotherapy and radiation for 4-6 weeks then his surgeon plans on removing the tumor after another 4 weeks following chemo. Is it possible to help open up his esophagus with cryoablation for example while undergoing his other treatments. I am concerned that with his esophagus blocked by the tumor 70% that this will start to seriously impact his ability to eat. I am interested in any information you might have to offer. Thank you so very much for your kindness and your efforts to help people educate themselves on the best options available.
Hi Monique-
I apologize for the slow reply. Major holidays always slow my cancer coaching. I am sorry to read of your dad’s EC diagnosis. I can provide evidence-based integrative and complementary therapies though it is difficult for me to know enough about your dad’s situation to be able to answer your question about his throat, cryoablation, etc. This is something his oncologist must speak to.
An example of an integrative therapy is curcumin in combination with the possible standard chemotherapy regimens cisplatin and 5-FU-
I encourage your dad to take integrative therapies for radiation as well. Let me know if you have any questions.
David Emerson
ReplyHi there,
I was recently diagnosed with Stage IV colon cancer with spread to the liver and I am already aware of the extremely low prognosis, I was wondering if you had any ideas of what I should do as a last resort? My oncologist told me that surgery would not be an option at this point and the best we can do is go full-out with chemo and hope for the best. I am very wary of this as, with the state I am in, chemo will most likely weaken my body even more. What would you recommend to me at this point? I am at a crossroads as I fully believe in natural therapies but I don’t want to take too much of a risk of making it worse. Also keep in mind that I am only 18 (which made my cancer diagnosis even more of a shock)
Thanks
Hi Sarah,
I apologize for the tardy reply. I am sorry to read of your metastatic stage 4 colon cancer diagnosis. As for your question ” I was wondering if you had any ideas of what I should do as a last resort?” I would use every evidence-based therapy, conventional and non-conventional, that I could identify. For example, I would combine evidence-based integrative therapies with chemo in an effort to enhance the chemo while moderating its toxicity, I would pursue nutritional therapies, I would take supplements that have been shown to be cytotoxic to colon cancer, etc.
I too believe in natural therapies as they are non-toxic for the most part however keep in mind that your cancer is advanced enough that you many not have enough time to allow natural therapies to work.
The fact that you are young (18) can be viewed as a positive… sort of. Meaning your body should manage the shot gun approach I outline above. The older average cancer patient (65-70) cannot handle the rigors of cancer therapy generally speaking.
I am both a cancer survivor and cancer coach. I work with cancer patients to design therapy plans like the one I am advocating for you. Let me know if you have any questions.
Hang in there,
David Emerson
ReplyHi Sarah-
I came across an article just now that may be of interest to you. I will link the article and also excerpt that content which I think applies to your. Keep in mind that your current oncologist/center may not provide this therapy. You may need to research those cancer centers that do provide this therapy. While you do not have “Peritoneal carcinomatosis” the therapy discussed below might be useful for you combined with nutrition, supplementation, lifestyle, etc. Again, you are young so go for it…
HIPEC in Colorectal Cancer With Peritoneal Carcinomatosis
“As CRS and HIPEC are still accumulating data, there are a limited number of clinical trials off which to base regimens. One study showed a median overall survival of 19.2 months in patients treated with CRS and HIPEC.4 The overall survival was increased to approximately 32 months when there was complete CRS. Another study demonstrated an overall median survival advantage when comparing CRS and HIPEC (22.3 months) to palliative surgery combined with systemic chemotherapy (12.6 months).5 A systematic review reported improved medial survival—33 vs 12.5 months—and 5-year survival—40% vs 13%—when comparing CRS and HIPEC to palliative surgery and systemic chemotherapy.6”
Let me know if you have any questions.
David Emerson
ReplyHi David: I was diagnosed with prostate cancer in 2006, biopsy, T2b and my PSA at 6.5. Symptome: Nocturna, getting up 6 or so times a night.
and taking a watch and wait approach. In 2015 my PSA 93 and in April
took hormone shot which dropped Psa to 5.Now Psa back to 23. I am not
in favor of doing another biopsy, risks involved. Do you know any other
way of dropping PSA then going back on hormone shot? Now, I’m 76 years old. Thanks for your suggestions.
Hi Clement-
If I read your post correctly you are in favor of balancing quality with quantity of life. Meaning you do NOT want to undergo aggressive therapies and run the risk of short and long term side effects.
There are a host of evidence-based, non-toxic prostate cancer therapies. Yes, these therapies are slow acting compared to therapies such as radiation or prostate removal. But there are few if any side effects.
Further, there are evidence-based therapies that integrate with hormone therapy (androgen deprivation therapy). I understand your desire not to have another biopsy but you should keep an eye on your prostate cancer. How about another PSA test?
David Emerson
ReplyΙ am sure this artiϲle has toucheⅾ all thee innteгnet visitors, its
reallү really nice paragraph on building up new blog.
My father was diagnosed only 2 weeks ago with stage 4 Metastatic Prostate cancer, spread into the bone and impacting the bladder. He was in medicine before his retirement, but always appreciated integrated medicine and had us on many naturopathic remedies as kids. I’m told that the proscribed regimen: hormone therapy, radiation, and later bone building therapy; will give him great relief of pain in the short term a great prognosis for recovery in long term. BUT it involves getting a bone biopsy he does not want. Now he is debating the whole regimen. What naturopathic or other treatments are available with some evidence of success? Currently he cannot walk unassisted due to size of prostate and impairment of bone, and I fear if he does not begin something ASAP he will lose what is left of his strength.
ReplyHi Caroline-
I am sorry to read of your father’s metastatic PCa diagnosis. This is a long reply so be sure to ask me anything that you find confusing.
I’m not sure but I think you left out the word “not” in the sentence about pain relief and long-term prognosis. I will be direct. Once prostate cancer grows outside of a man’s prostate gland, there is no conventional curative therapy. The therapies prescribed for your dad, hormone, radiation, bisphophonates (bone strengthening) are all therapies that slow your dad’s PCa but they cannot cure it.
Keep in mind that while these therapies are designed to “give him great relief of pain” they will also give him short and long-term side effects. Hormone therapy is also called Androgen Deprivation Therapy. Radiation may cause damage to surrounding tissue.
I don’t know what the bone biopsy is for. I don’t believe his oncologist will not allow the above mentioned therapies to proceed if your dad does not have a BMB.
There are many evidence-based, yet non-conventional (not approved by the FDA) therapies for PCa and for bone pain. All are complimentary meaning that they will not interfere with his conventional therapies.
MR imaging-guided focused ultrasound for treatment of bone metastasis.
What stage does your dad live in? CBD oil has been shown to be cytotoxic (kill) PCa while giving pain relief and helping people sleep.
Let me know if you have any questions.
David Emerson
Cancer Survivor
Cancer Coach
I was diagnosed with a benign brain tumor (on the left outside, next to my skull). they want to do surgery, I am using frankincense oil on the roof of my mouth for now and taking Keppra, have some swelling around the tumor. Having some headaches is all.
ReplyHi Terri-
I am sorry to read of your benign brain tumor. Good luck.
David Emerson
ReplyHi David,
I wonder if you have ever stumbled on anything useful regarding NF1.
My son is 3 y.o., and has this gene mutation making him prone to tumors. He has optic nerve gliomas on both sides, at present I am sticking to diets (as much as possible with such a small toddler), curcumin, reishi, organic sulfur, aloe gel, Hoxsey tonic, … my list is long. His last MRI shows no progression, which is a victory in itself. But I’m always looking for a fresh look on his protocol and ideas how to maybe make it even better. Have anything in your sleeve for gliomas or NF1? For toddlers?
Thank you in advance!
Have a wonderful weekend!
Rosie
ReplyHi Rosie-
If I understand you, your 3 year old son has optic nerve gliomas that are benign and not growing? If this is correct, yes, your efforts are in fact a victory in itself. By this I mean that conventional oncology has little to offer you. And you are managing your son’s situation successfully with non-toxic therapies. I know of no specific therapy for NF! gene mutation.
However I will say that I believe that genetic expression can be changes through diet, supplementation and lifestyle- like you are doing- aka epigenetic. Therefore you appear to be doing as much as possible in your situation.
I wish I could offer more info and therapies. Let me know if you have any questions.
David Emerson
ReplyI need a second opinion from a chemotherapy doctor. My chemo oncologist has told me that I would not be able to receive chemo here in Canada if I traveled abroad for immunotherapy and then had a later recurrence. In testing, immunotherapy has shown to be more more potent against my particular cancer than Xeloda. My cancer advisor has told me to get a second opinion but I don’t know where to start. Do I ask my family doctor to set it up or do I just start phoning around?
ReplyHi Derek-
I am sorry to say that I do not have an answer for you. I am not a medical doctor. Further, we have different rules here in the states.
I am sorry that I cannot be more help.
David Emerson
ReplyYou sһould take part in a contest forr one of the best websites on the web.
I’m going too hjghly recommend this web site!
Hi, David I just had surgery to remove a type 2 hemangiopericytoma it was total recession.
On August 31st. And now I am second guessing my self about radiotherapy (radiation) for the tumor bed. The questions is should I do this?
Hi Ericka-
I am sorry to read of your HP. I am sorry for my tardy reply. Several points for you to consider in answer to your question “And now I am second guessing my self about radiotherapy (radiation) for the tumor bed. The questions is should I do this?”
I will link and excerpt a study below that pertains to your situation.
Hemangiopericytomas grade II are not benign tumors.
“With respect to the available literature and our own experiences, the aggressiveness, especially of differentiated grade II HPs, seems to be underestimated…”
“Complete surgical resection could be achieved in 60% of cerebral and in 25% of spinal HPs”
“in this study, we could not detect a single patient showing any recurrences or systemic metastases after complete surgical resection of grade II HPs..”
“With respect to our results, radical surgical resection offers the best treatment option to control tumor progress. In case of subtotal resection or histopathologically diagnosed anaplasia (WHO III), radiotherapy seems to be indicated; however, chemotherapy did not show effectiveness to control tumor progress.”
This study concludes that grade II HP’s that achieve COMPLETE resection did not benefit from chemo or radiation. Keep in mind that this is a rare cancer and this is a small study of a rare cancer.
There are evidence-based, non-conventional therapies that are cytotoxic to various cancers including brain cancers. I would have to research/look for for specific therapies for grade II HP however. I mention this because I pursue non-toxic to manage my own cancer. As a cancer coach I research non-toxic therapies for other cancers.
Let me know if you have any questions.
David Emerson
ReplyI am 70 yrs and was diagnosed as Blood cancer patient in Aug.2016.I am avoiding chemo.(light dose)and taking Ayurvedic medicines and garlic and termeric powder.i am also doing yoga exercises and go for average walk.My neutrofils had gone to 0.2% on 25 Aug.16 then came to 0.3% on 6th.Oct.16.Yesterday i went for blood work and again neutrofils have gone down to.0.2%.What to do.My Doc.briefed me about side effects of tretment.
ReplyHi Gurbackan-
Can you tell me which blood cancer you have been diagnosed with? Leukemia, lymphoma, multiple myeloma?
David Emerson
ReplyDavid,
How fortunate can I be? I was looking for alternatives to MM treatment and look where I landed. It almost 10:30 out here in San Diego. I’m normally in bed by 7. So I’m getting sleepy. But I read your article and tomorrow when I not so tired,I’ll read it again. I don’t yet know how you can help, but hopefully I’ll find out tomorrow. I’ll try now to give a brief summary of where I’m at with MM.
I was diagnosed 2 years ago and they wanted to start me on Revlimid. When I read the history of the drug, I balked. I’m old enough to remember the Thalidomide babies and a classmate of mine actually had one of those children. She died at birth.
I got a second opinion from Mayo in Rochester and decided to delay any treatment but just be monitored.
This January, the ONC told me I couldn’t delay any longer. She thought my kidneys were being affected and in months I may need dialysis. So I started treatments that day. Because I was in very good condition for 83, she prescribed an “aggressive” treatment. I can’t remember the names but each Wednesday I got 40 mgs of a steroid, 14 capsules of some chemo drug and a shot in the belly. Side effects were minimal – a little bloating for a few days. But the s hit the f on Mother’s Day. The pain from my waist down my legs was so awful that I went to the ER twice before they knew I was really in a lot of pain. I hate to say it but the pain killers didn’t work.
But they released me and about 10 days later I saw my PCP who put me on both Morphine and Percocet. That finally relieved the pain. But I continued treatments despite the pain until the end of June. ONC decided that the bad was outweighing the good. I’ve spent the ensuing 4 months trying to get back to health. Last week was the first time since Mother’s Day that I can say I’m on the road back. I am walking 2 miles each day and I’m starting a program at the Y in November to get some strength in my muscles.
Last week I had a meeting with the ONC. The critical test (I don’t know what it’s called) but it went from a low of 0.9 in July, to 1.1 in August and to 1.7 in October. The next day she referred me to an associate who is Myeloma-only. After about 10 minutes, he said “you can’t wait any longer, you must start Revlimid next week.” The hated word Revlimid is back.
I haven’t met with my ONC since then but I’ve been thinking and I think I want to see if there’s something else that I should consider. Btw, I’m not afraid to die. The thought probably bothers my wife and children more than me. I just don’t want to die a painful death.
I’ll be back at your site tomorrow. thanks for being here.
bob
HI Bob-
I am sorry to read of your MM diagnosis and therapy side effects. While MM is a complicated blood cancer you do have options- both conventional and non-conventional. It is difficult for me to list your options with pros and cons so I will list a few general areas for you to think about.
Conventional FDA approved chemotherapy regimes such as Velcade (the shot in the belly), Dexamethasone (the steroid), and Revlimid (pills)”
While conventional oncology works to adhere to “standard” regimens (cocktails) and doses, you to not have to only choose yes or no. For example if a dose of Revlimid of 10mg daily causes a negative reaction than you can lower the dose to 5 mg.
Evidence-based integrative therapies:
There are a number of well-researched, non-conventional therapies that have been shown to increase the efficacy of a specific chemo (Revlimid again) while reducing possible side effects.
Complementary therapies:
Frequent, moderate exercise is an excellent example of an anti-MM complimentary therapy. As a MMer myself I have researched and practice an anti-MM program daily, weekly, etc. All non-toxic. All based on research studies.
The blood test that you refer to is probably a serum protein electrophoresis- while your numbers increased a bit they are still low relatively speaking.
My overall point is that you can focus on both length of life and quality of life by combining conventional and non-conventional therapies.
If you would like to talk more please switch to my email address David.PeopleBeatingCancer@gmail.com– email is easier for communication.
David Emerson
MM Survivor, MM Cancer Coach
[…] https://peoplebeatingcancer.org/ […]
Reply[…] Cancer Coaching- getting a different kind of second opinion – Please consider getting a different kind of second opinion from an experienced cancer coach. I have been living with multiple myeloma since 1994, and I would like to … […]
ReplyMy breast cancer recently came back after being in remission for 16 years, I am a 70 year old MALE, doctors say it is very treatable, been on two chemo pills for 6 weeks now, plus cannibals oil that was recommended by my oncologist, going for another petscan oct 3, will keep you updated !
ReplyHello and congrats on your survival! I was a 2 time cancer survivor. I am working on my 3rd time survival now. I must say this time I am not as optimistic and I’m letting it get to my head some days.
So, rare cancer at age 8. (Rhabodomyo sarcoma) treated with surgery, chemo (back in the 80s and it was PURE HELL) radiation.
age 28- diagnosed with ovarian cancer stage 3 (borderline-low grade serous micropapillary ). Hysterectomy, chemo (Carbo/taxol) 6 rounds. Then being deemed remission for 10 years and then “cancer free” once the 10 yr mark after chemo hit.
Flash forward to last year. At year 11 was diagnosed with recurrence of Ovarian cancer. Ca-125 at time was 129. I asked what stage and was told by onc.cancer isn’t ‘staged’ but considered ‘reoccurence’. Doing my homework I would be stage 4. It has spread throughout abdomen, onto lower lung and liver. My lymphnodes in neck and groin were tender-and enlarged- but no “masses” inside of them per CT. They were never biopsied. She said treatment would remain same even if nodes were positive.
She states Im resistant to chemo since it came back. ( I feel I wasn’t since it was maybe dormant for 10 years?). She started me on Avastin IV every 21 days. — CT scans after every 6 treatments. CA-125 dropped to 12 (Thank you Jesus!) and the ‘measurable’ tumors were shrinking 0.5 to 1 cm per 6 treatments. But, theyre still there. The last CT showed no shrinkage of tumors this 6 rounds of chemo and CA-125 went up 5 points (30%) which freaks me out. (they aren’t concerned with that number) I’ve read that Avastin only works short term and the cancer figures out how to get around it.
I am a “need proof” kind of person. I have never been into alternative treatments because I worked in med.field for so long and I know that drugs DO work in some cases. Now, I am open to different types of therapy. I just want my cancer to be (of course gone-but if not an option–) controlled so that I may continue living. I DO NOT WANT TO DIE OF CANCER OR ANYTHING RELATED TO IT (chemo etc).
I have essential oils people coming out of woodwork, total vegans saying I’m killing myself, people telling me “sugar feeds cancer as well as dairy”, convert to an alkaline state body etc. I am so torn and don’t know what to think because my Oncologist disputes all of these and has a “good” explanation of why they all wont work.
I have been looking at getting second opinions from John Hopkins, MD Anderson, Ketter memorial and then also possibly a holistic or natural approach dr.
I am open for new approaches for my type of cancer. Please advise what you would do.
I used to be in the “survivor” category. Now, I’m back in the “fighter” category. This fighting is wearing me out!!!
Sincerely,
Mich.
Is Mich short for Michelle?
HI Mich-
And I thought I had been through the cancer ringer. I am impressed with your survival history. I too get down sometimes. A pain in my lower back while getting out of bed will make me wonder if I have relapsed.
I too am a “need proof” person. While I live a non-FDA approved lifestyle every therapy I take is evidence-based. There is lots of research that supports various therapies that have nothing to do with the FDA.
Avastin is an anti-angiogenic chemotherapy. It is working. I believe that you should focus on this therapy. I follow an anti-angiogenic lifestyle through nutrition, supplementation, lifestyle and mind-body therapies. The mind-body therapies aren’t anti-angiogenic…
An example of an anti-angiogenic therapy that is non-toxic is curcumin. Curcumin is anti-angiogenic and is synergistic with avastin.
I am both a long-term cancer survivor and cancer coach. I work with patients and survivors to research and design evidence-based, non-conventional programs to manage their cancer.
Let me know if you would like to learn more about cancer coaching. Hang in there.
David Emerson
Reply[…] Cancer Coaching- getting a different kind of second opinion – I am a 63 year old male who was diagnosed with prostate cancer 2 years ago. the oncologists recomment surgery to remove prostate, or radiation or both as needed. […]
ReplyHi 63 year of male-
I am sorry to read of your PCa diagnosis. Do you have a question?
David Emerson
ReplyHi Ron-
This is a good question but there is no way to know for sure.
David Emerson
ReplySomeone recently mentioned that to me—that it has some evidence based outcomes? also CBD?? is that the same thing? I also heard about Turkey Tail Mushroom achieving some good outcomes in trials. Do you know about any truth to any of that?
ReplyYes, turkey tail mushroom extract has been shown to kill PCa.
As I mentioned in my previous email, there are a number of evidence-based supplements that are cytotoxic to PCa. And yes, Cannabidiol (CBD oil) fights PCa too. Great for pain management depending on the strain and ratio of Cannabinoids and THC.
The bottom line is that conventional oncology is designed to prescribe conventional FDA approved therapies. Evidence-based but non-conventional therapies such as CBD oil, mushrooms, curcumin, anti-PCa nutrition, lifestyle therapies, non-toxic bone therapies, etc. all are outside the expertise of conventional oncology. I am both a long-term cancer survivor and cancer coach.
Let me know if you have any questions.
David
Reply[…] Cancer Coaching- getting a different kind of second … – Cancer Coaching- getting a different … Seeking a second opinion indicates that you are … I remember having heard about curcumin being good for the health in … […]
Reply[…] Cancer Coaching- getting a different kind of second … – Please consider getting a different kind of second opinion from an experienced cancer coach. I have been living with multiple myeloma since 1994, and I would like to … […]
Reply[…] https://peoplebeatingcancer.org/ […]
ReplyHi, my dad has stage 2 bladder cancer it’s in the muscle now. First they said it would have to be removed along with the prostate. Then later another doctor said he has two options. Chemotherapy with 50%chance or remove it and wear a bag. He decided on removal. But last year he had 3 blocked arteries and had 3 stints put in. His heart doctor said he wouldn’t make it through the 5-6 hour surgery that he would die on the table. There has to be something else besides chemo.
ReplyHi Jerry-
If I understand your email, your dad’s recommended therapy for stage 2 bladder cancer was Radical cystectomy (bladder removal). Due to the condition of your dad’s heart function, his cardiologist has recommended against bladder removal surgery. You don’t like the chemotherapy option and are looking for other options/therapies for your dad’s bladder cancer?
The key issue for you and your dad is what his oncologist meant when he talked about “chemo” as a therapy. The study linked below refers to two different chemo cocktails. As you will read, both cocktails are valid treatments for your dad’s cancer. However, there are different integrative therapies available depending on which chemo your dad has.
An example of an integrative therapy would be a chemo drug called cisplatin and an antioxidant called curcumin. Integrative therapies will enhance the effectiveness of the chemo regimens (depending on which chemo you choose) as well as reduce the toxicity which is important for your dad.
Curcumin reduces cisplatin-induced neurotoxicity in NGF-differentiated PC12 cells.
Let me know if you have any questions.
David Emerson
ReplyI been diagnosed with cervical cancer. The doctor told me I have only a few months. I do not have any side effects which told me. I am looking into
LRHT hyperthermica, high dose vitamin c, mistletoe.
Could you please answer me and tell me what you think or maybe you know
other options. Thank you
Hi Bella-
My apologies for this tardy reply. I am sorry to read of your cancer diagnosis. Personally I don’t believe oncologists should give dire prognoses. I was told I was terminal in 1997. Boy was she wrong…
Ironically, by giving you a grim prognosis your oncologist may have done you a favor. It meant that the standard of care techniques for your cancer and stage would not have resulted in a positive outcome.
As the two articles linked below indicate, a combination of intravenous vitamin C therapy and deep tissue hyperthermia may result in the positive outcome that you are looking for.
Your challenge will be 1) to find those cancer centers that have expertise in these two therapies and 2) getting your health insurance to pay for these therapies.
According to my research Mistletoe helps people cope with side effects more than it actually fights cancer.
I am both a long-time cancer survivor and cancer coach. My value would be in finding institutions with the experience you are looking for as well as researching and presenting those evidence-based therapies that are cytotoxic to cervical cancer. Among other therapies I will recommend anti-angiogenic nutrition, supplementation, anti-cancer lifestyle therapies and mind-body therapies.
Let me know if you would like to learn more about Cancer Coaching. Hang in there,
David Emerson
Intravenous Vit. C and chemotherapy
Cervical cancer: radiotherapy and hyperthermia.
ReplyHi David! I’m a 45-y.o. male who has been diagnosed with colorectal cancer (stage 4, metastasized to liver) 7 mos ago and after 6 months of chemo, my colon has returned to normal appearance and function and the tumors I have in the liver have also responded to treatment, but my liver surgeon wants me to have radioembolization soon, as my liver still has enough tiny calcified spots of cancer interspersed throughout to make surgery / resection impossible at this time. So he wants to go after the handful of tumors on both sides of the liver.
I’m looking for a second (or third) opinion on whether this is the right way to go.
Scans have shown no cancer outside of the liver; I’d rather not go thru more chemo but I imagine I will eventually. I’ve been taking a couple of supplements (Renafood, Drenamin) but that’s about it so far. Been feeling good throughout the treatments and have been maintaining a positive attitude from the beginning, I just wanted to make sure radioembolization is the correct next step to take. Thanks for your help!
ReplyHI Eric-
Several things. First of all, I need a little more time to research your questions. I am amazed that you are doing as well as you are considering your original diagnosis. Next, you know that I am not a certified onc. I am a knowledgable cancer survivor but not an oncologist of any kind. Lastly, what were the names of the chemotherapies that you underwent?
Yes, you should get a second opinion- ideally from an oncologist who will understand you cancer and your therapies. And yes, I will give you a different kind of second opinion. Get both.
This may be a stupid question but are the “handful of tumors on both SIDES of the liver” on the outside of the liver? Is so why can’t the onc. cut them out with regular surgical techniques?
I will do some more research. Please answer the questions above.
thanks
David Emerson
ReplyHi David, thanks for the quick reply!
I looked at my notes and here’s what I was taking during the first round of 6 treatments (infusion every 2 weeks):
500mg Avastin
900mg Adrucil
896mg Leucovorin
190 mg Eloxatin
and then I’d have about 300ml of FU-5 (fluorouracil) in a pump that dispenses over 46 hrs afterwards.
In Jan, I had CT scans done and it was determined since I handled the chemo without too much trouble, that I should do another round of 6 infusions with additional chemo, but I still need to find out what was added along to the above list.
To clarify, I meant both halves of my liver, not sides. Sorry about the choice of words there.
There are small tumors interspersed throughout and that seems to be why my liver surgeon is recommending radioembolization, after all the chemo I’ve had. I’ve learned that this procedure will rule out surgery in the future, so after speaking with an oncologist at Sloan-Kettering last night, I am getting a sense that my case might need a surgeon with more experience to review my scans and determine whether I truly am currently inoperable, or whether my current surgeon is just uncomfortable with the state of my liver.
it doesn’t matter whether you have capital letters after your name, the energy you’re giving freely to other cancer patients with your research and this blog is much appreciated and noted.
Thanks again, Eric
Hi Eric-
To summarize- stage 4 colon cancer has been satisfactorily managed. I don’t want to use the word cure but you underwent a great deal of toxicity and your original cancer seems to be under control. Further, your supplementation of Renafood and Drenamin, also seems to be helping (don’t stop).
The last piece of your therapy picture is how best to further remove small tumors in your liver. Surgery is out. More chemo is out. Based on the studies below, radio embolism seems to be a reasonable choice meaning should eliminate the tumors with few side effects.
Radioembolism for liver mets in BC patients
The only other therapy I can think of is to research and undergo evidence-based non-toxic therapies. I supplement with milk thistle to keep my liver healthy. There are other liver therapies for you to consider.
Thank you for your kind words about me helping cancer patients. Keep in mind that I run this non-profit both with corporate, grand making foundations couple with revenues from my cancer coaching. Thanks.
Let me know if you have any questions. Thanks.
David Emerson
ReplyI was recently diagnosed with Stage 1c Epithelial Ovarian Cancer, with two tumors. One on left, called Serous high -grade carcinoma and one on right called Endometrioid adenocarcinoma. Both were large and removed, along with uterus, cervix, 9 groin lymph nodes and 5 periaortic lymph nodes and peritoneal lining. Nothing else showed up anywhere else. Lucky, huh?! The doc wants me to do 6sessions of chemo.
So I want to go alternative ways, but am open to what you have to say.
Thanks, NB, CA
Please leave my full name off when you respond.
Hi Nora-
I am sorry to read of your ovarian cancer diagnosis. If I read your comments as well as the study excerpted below I believe your risk of relapse is extremely low. Further, it doesn’t seem as though chemotherapy will reduce the risk of relapse enough to offset the collateral damage aka side effects.
When you say “I want to go alternative ways…” I take you to mean that you want to undergo non-toxic or “natural” therapies that will both enhance your immune health while reduce your risks of relapse? I couldn’t tell if you were serious when you said “lucky, huh?” But in a way, you may be lucky. The clean living you follow in the coming years, if you choose to, may result in a better, longer life…
If this is the case then you can research and undergo those therapies that you believe will help you or you can follow those nutritional, supplement-based, lifestyle and mind-body therapies that I research and present to you. I say “present” because I try not to tell cancer patients what to do. I present studies and make recommendations based on research and my own experience as a long-term cancer survivor and you then decide what is best for you.
I am both a long-term cancer survivor who lives an anti-cancer lifestyle based on my research, as well as a cancer coach. Let me know if you would like to learn more about my cancer coaching.
Thanks,
David Emerson
Prognostic Factors in Patients With Stage I Epithelial Ovarian Cancer.
“We analyzed factors predictive of relapse risk in patients with stage I invasive epithelial ovarian cancer: 252 patients from the Princess Margaret Hospital provided a data base for hypothesis generation, and data on 267 patients from the Norwegian Radium Hospital were used for hypothesis testing. The outcomes in most analyses in the two series were very similar, validating the following conclusions. Differentiation (grade) was the most powerful predictor of relapse, followed by dense adherence (which resulted in outcomes equivalent to those in stage II) and, finally, large-volume ascites. When the effects of these three factors were accounted for, then none of the following were prognostic: bilaterality (stage Ib), cyst rupture (stage Ic), capsular penetration (stage Ic), tumor size, histologic subtype, patient age, year of diagnosis, and postoperative therapy. These results allow simplification of stage I substaging, as only differentiation, dense adherence, and large-volume ascites (? peritoneal cytology) need be considered. The 5-year relapse-free rate was 98% in patients with grade 1 tumors in whom both dense adherence and large-volume ascites were absent. These patients are adequately treated by operation alone. Although the relapse risk was high enough in the remaining patients to warrant postoperative treatment, a significant benefit could be shown only for a small subset of patients, namely those with densely adherent tumors treated with abdominopelvic radiotherapy. In grades 2 and 3, none of the therapies used in either series was superior to pelvic radiotherapy or operation alone.”
ReplyHi I’m 23 years old just recently relapsed from hodgkins lymphoma. They want to give me a potent intense chemo along with astem cell transplant. I’ve decided to seek other alternative options. Do you have anything in mind specifically for lymphoma?
ReplyHI Stephanie-
Your choices of therapies be they conventional or non-conventional, will be based somewhat on your stage and symptoms. In other words I need to know more about your NHL situation to do more research and to then give you some choices. You are way ahead of the game currently simply by being young and otherwise healthy.
What stage are you based on your relapse? What, if any symptoms are you experiencing?
thanks
David Emerson
ReplyHi, I am a 48 year woman diagnosed with stage 2A TNBC in left breast, no lymph involvement and clear margins, in Nov. 2015. I had a double mastectomy in Dec., followed in Feb. by chemotherapy 4xDD AC and then planned for 12X weekly paclitaxel. Unfortunately, after the third treatment of paclitaxel, I had the side effect of lung toxicity reaction that resulted in infection – pneumonia (no sign of cancer) and am currently being treated by steroids to treat the lungs and everything is on hold. I have been told that there may not be any other options for chemo treatment if the paclitaxel is deemed to be too risky to retry from a lung perspective (they are looking at pab-paclitaxel) which is a concern for me from TNBC perspective. Radiation is planned after chemo.
Do you have any other suggestions? I am also interested in other therapies – I have already switched to cancer-fighting diet, moderate exercise, meditation and had been coping well with chemo up until pneumonia. Thanks
ReplyHi Julie-
I am sorry to read of your TNBC diagnosis. To confirm, your triple negative BC was localized aka no node involvement? You had 4 time dose dense adriamycin and cytoxan? And after the third round of paclitaxel you developed pneumonia and are on hold?
Yes, I have several suggestions. Before I begin, I am going to have to be honest with you. Julie, you have undergone a TREMENDOUS amount of chemotherapy aka toxicity. I know that at 48 your are pretty young as cancer patients go but jeez. Understand that my perspective and experience is that of a long-term cancer survivor who has experienced many long-term and late stage side effects from my own chemo years ago.
My approach as a cancer coach is to manage chemo toxicity where ever and when ever possible. Meaning, if you choose to continue with paclitaxel I would suggest taking those non-toxic interegrative therapies that studies have shown enhance the efficacy while reducing toxicity of paclitaxel. I will link an example below.
Your other option is based on the idea that your oncologists are giving you so much chemotherapy because TNBC relapses more often than other forms of BC do. The trouble is, as I see it, by giving you so much chemo NOW, your TNBC may become chemo resistant, giving you no options later.
There are are many evidence-based BC supplements that are cytoxic to BC. I believe your therapy plan should include anti-BC nutrition, supplementation, lifestyle (yes moderate but frequent exercise for example) and even mind-body therapies. My cancer is different from your but I do all the above and I have been in CR since 1999. Myeloma survivors (my cancer) learn to live with their cancer for years. Please read the article about this idea in the medscape article below.
An Evolutionary Approach: Learning to Live With Cancer
Potentiation of paclitaxel activity by curcumin in human breast cancer cell by modulating apoptosis and inhibiting EGFR signaling.
“Overall, our data described the promising therapeutic potential and underlying mechanisms of combining paclitaxel with curcumin in treating breast cancer.”
Julie, I am a long term cancer survivor and cancer coach. Let me know if you would like to learn more about cancer coaching for you.
thanks and hang in there,
David Emerson
ReplyI’ve recently (6 mos ago)been diagnosed with metastasized kidney cancer in my lungs after having had a radical nephrectomy. It’s very small right now and my onc doesn’t foresee any treatment for 6-12 mos. I’ve given up red meat, sugar and most carbs. I’m exercising daily and taking fish oil, curcumin, CoQ10, green tea extract, quercetin, D3, milk thistle extract and resveratrol. I have another CT scheduled in a couple of weeks. My question is, do you see any health benefits in adding flaxseed to my diet? What other additions or deletions would you suggest?
ReplyHi Jeff-
I am sorry to read of your metastatic kidney cancer. However I have to say you are doing everything I know of to reduce the spot in your lung? And a relapse of kidney cancer too.
Your questions “do you see any health benefits in adding flaxseed to my diet? What other additions or deletions would you suggest?” Flax seed is another form of omega 3 fatty acids. Since you are already taking fish oil I don’t see the need to take more.
According to the study linked below, yes, omega 3 fatty acids reduce the risk of kidney cancer (scroll down about half way…)
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2863302/
In order to speak to adding or deleting any of the supplements that you are currently taking I would have to research each. However I take most every supplement you mention so my guess would be that each provides some anti cancer benefit.
Let me know if you have any questions.
David Emerson
ReplyI HAVE BEEN DIAGNOSED WITH GLEASON 6 PROSTATE CANCER WHICH THE MRI INDICATES IS CONTAINED WITHIN THE PROSTATE GLAND. MY PSA ON FEB 4 WAS 6.0. MY UROLOGIST SUGGESTED “WATCHFUL WAITING” AND NO ALARM OR ACTION. ON APRIL 27 WAS PSA WAS 8.1. I WILL GET A SECOND OPINION.
QUESTION: SHOULD I CONSIDER PROTON THERAPY INSTEAD OF SURGERY?
ReplyHi Michael-
Without knowing too much about your case I have to agree with your urologist that observation is the best path for you at this point.
Regarding your question “QUESTION: SHOULD I CONSIDER PROTON THERAPY INSTEAD OF SURGERY?” Please consider the issues below-
1) if by “surgery” you mean a complete prostatectomy or removal of the prostate, please understand the risks of urinary incontinence (about 50%) and erectile disfunction (again about 50%). How old are you? Do you live in a state where medical marijuana is legal? CBD oil has been shown to by cytotoxic to prostate cancer.
2) Radiation can be a possible therapy, again, if you understand the risk of side effects and take steps to minimize them.
3) most importantly, please consider undergoing non-toxic therapies that studies have shown reduce your risks of prostate cancer. Please read the links below.
1) Green Tea Extract-
Green tea polyphenols for prostate cancer chemoprevention: A translational perspective
2) Curcumin-
Curcumin-based anti-prostate cancer agents.
3) Vitamin D3
Vitamin D for the Management of Prostate Cancer
4) Milk Thistle-
Let me know if you have any questions.
David Emerson
Replymy son is 14 and diagnosed with Pre-B ALL he started chemo treatment on Dec 31 2015.Doctors told us at the begining of Feb.he was already in remission but protocol calls for intense treatment for 6,8 mths then 2 years of maintenance.As any parent Im scared of what the chemo can do and realy i dont understand why they have to hit my son so hard with chemo. can you help me to understand why if hes in remission cant the chemo stop
ReplyHi Karen-
I am not an expert on pediatric pre-B ALL so this is my opinion as an long-term cancer survivor of an adult blood cancer. I believe you have reason to be scared.
My experience with conventional oncology is that specific protocols have been tested and approved by the FDA. Only by following the protocol for pediatric B ALL are the oncologists able to be relatively sure of the outcome. This outcome is a long-term remission I assume.
Yes, “intense treatment” of chemotherapy will increase the documented risks of late-stage and long term collateral damage. I cannot sugar coat this as I myself suffer from long-term and late stage side effects from my own therapy in ’95-’97.
I will say however that I follow a regimen of non-toxic therapies that research shows will reduce the risk of relapse or manage my side effects. In other words, there are a variety of non-toxic therapies that your son can undergo once his active therapies stop.
Let me know if you have any questions.
David Emerson
ReplyMom had breast cancer 2 years ago and it’s come back last week as a secondary distant cancer in the fluid around her lung and no where else at present. The original cancer was triple negative breast cancer stage 2 in March 2014.
It’s now been diagnosed as Stage 4 Adenocarcinoma and Metastatic with a Malignant Pleural Effusion. According to her doctor, it’s incurable and patients survive from a few months to up to a year or sometimes 1 year and a half.
Any suggestions are welcome.
Hi Shona-
I am sorry to read of your mom’s stage 4 BC relapse. Triple Negative BC is difficult because it relapses more than other cancers. Once BC relapses it cannot be cured.
However I would like to present an approach to managing your mom’s cancer that is common with my cancer, multiple myeloma but NOT common with your mom’s cancer. Since it is difficult to discuss complicated therapies in emails, I hope that you will ask me lots of questions in future emails.
Did your mom have a chemotherapy called paclitaxel when she was first diagnosed with BC? The article linked below talks about controling your mom’s cancer with a series of low-dose administrations of paclitaxel.
An Evolutionary Approach: Learning to Live With Cancer
Further, the study linked below talks about how an antioxidant called curcumin ENHANCES the efficacy of paclitaxel.
At the same time your mom undergoes low-dose paclitaxel and curcumin I would like you to consider having your mom also undergoing several non-toxic therapies shown to also fight triple negative breast cancer.
Shona, I was told I was terminal in 1997. Had I listened to my oncologist at the time I would be dead now. Please don’t listen only to your mom’s oncologist.
Let me know what you think.
David Emerson
Cancer Survivor and Cancer Coach
Hi David,
It is a case of 28 year old woman, diagnosed with cervical/uterus cancer, who underwent surgery 2 weeks ago. Biopsy showed cancer cells in lymph nodes. Doctors advised she would have to undergo radiation therapy after about 1.5 months, and possibly chemotherapy, too. She wants to try any possible alternative methods to avoid these two. She has already started some with soda bicarbonate. She is considering also high dosages of Liposomal Vitamin C (e.g., Lypo-Spheric by LivOn Labs), but is concerned that they can interfere because of opposite pH (alkaline vs. acidic).
Your advice is much appreciated!
Thank you!
ReplyHi Alex,
I agree that there are non-toxic therapies to undergo before chemo and radiation. However I also recommend integrative therapies to those cancer patients I cancer coach. In other words, my research and personal experience has taught me that both enhancing chemo/radiation while reducing collateral damage aka side effects of toxic therapies should be a cancer patient’s primary focus.
Thanks and hang in there,
David Emerson
Long-term Cancer Survivor and Cancer Coach
I have two types of Leukemia. One is Essential Thrombocytosis, where my platelets are manufactured like crazy. This seems to be getting under control. The second kind is CLL (chronic Lymphatic Leukemia) With that, I am at stage 0. I have been trying a ketogenic diet, coffee enemas, and infra-red sauna. I am still losing too much weight, but could that be from all these things I’m doing? I’m also hearing way too many conflicting arguments on what the best diet is. SO confused and getting pretty scared. What do you think?
ReplyHi Scott-
I have to be honest with you. Your diagnosis of two types of leukemia is complicated enough that it is over my head. My experience would say that a ketogenic diet, coffee enemas, etc. are excellent forms of therapy. However, I just don’t have any experience with a person with two leukemias.
If, as you say you feel as if you are getting the ET under control and then if the CLL is stage 0 then I think you are doing well. I am not surprised that you are confused. Blood cancers are complicated.
David Emerson
ReplyI am a 50 year old female diagnosed with colon cancer after routine colonoscopy. I had a right hemi colectomy where colon lymph nodes were removed. Should I have chemo if only a few lymph nodes end up being positive? Chemo seems like such a toxic option if it’s only a few lymph nodes.
ReplyHi Eileen-
I am sorry to read of your colon cancer diagnosis. Cancer therapies are based on cancer diagnoses- a certain therapy for stage 1, stage 2, etc. If a cancer is contained in an organ such as your colon, then it is contained and may not required therapy beyond surgery. Once a cancer shows up outside an organ, in a lymph node for instance, it means that the cancer has spread.
The bad news is that your cancer has spread beyond your colon. The good news is that there are non-toxic therapies that work to enhance and or reduce the toxicity of whatever chemotherapy you undergo. An example would be a common chemotherapy for colon cancer called 5-fu (5-fluorouracil) and the integrative therapy would be curcumin-
Those two therapies are examples but there are others. Keep in mind that there are other completementary therapies that studies have show to reduce the side effects of chemotherapy.
My point is that chemotherapy does not need to by a toxic, side effect causing horror show. I’m not saying that integrative/complementary therapies make chemo easy. I’m saying that there is a middle ground.
If you would like to learn more please ask your oncologist what chemotherapy regimen he/she recommends for you. I will research integrative therapies for you to consider.
Let me know if you have any questions.
David Emerson
Cancer Survivor, Cancer Coach
Hi David,
I have begun chemo for stage 3 colon cancer, stage 2 removed tumor. 3 of 31 lymph nodes had cancer. Doctor has said I can take curcumin, but I don’t know what form or how much it is recommended to take. It’s not an official recommendation from the doctor, so wondering if you can give me insite. On 5-fu,oxaliplatin, and leucovorin.
Thanks,
Eileen
My grand daughter was diagnosed at Children’s Mercy Hospital in Jan 2015 with stage 3 & 4 Hodgkin’s Lymphoma. Witching the 1st month they gave her MRSA n a month long hospital stay that made her deathly ill. She completed her 1st round of Chemo n 6 months later diagnosed as “Cancer Free” but still has a 10 X 11 cm mass on her heart. She has never wanted to take any of the horrible Cancer drugs that traditional medicine has to offer. Problem #1 Children’s Mercy has hot lined many families for seeking second opinions or deciding to decline their treatments. Often these children are being taken away from their families, and parents being arrested. Problem #2 How can my grand daughter be Dx.. As “Cancer Free” if she still has a mass on her heart? Problem #3 The hospitals suggestion is now “Radiation” I know as a nurse the Radiation is a “Death Sentence”. How can we protect my grand daughter from Children’s Mercy Hospital n not have her taken by DFS and get her cancer cured naturally? Plz help! I am desperate! Thanks in advance!
ReplyHi Venessa-
I am sorry to read of your grand daughter’s health challenges. While I have some understanding as to how complicated and difficult your decision-making must be I am afraid I am not experienced enough with pediatric blood cancers to offer any help.
Good luck,
David Emerson
ReplyI went to see my oncologist april 11-2016;this is 2 years now that he has been seing me.After i got really upset about his very poor communicative skills,becouse after 1 1/2 finally he told me that i had MGUS-,next visit he said i had multimyloma,
2 months later i had myloma;yesterday he gave me a death penalty”YOU HAVE STAGE 4 LYMPHOMA AND WE MUST START CHEMO++++ IMMEDIATELy,BECOUSE THE LONGER WE WAITH-THE WORST IT WILL GET!!!!!!””I told him,that this is a very poor way of incompetence and communication;i am going to try the IPPOCRATIS WAY(NATURAL CURE AND REMEDIES) and i will take as long as i need,and if i die………..”BETTER THE IPPOCRATIS WAY THEN THE”CHEMO” WAY!!!””” I have ordered a 3 month supply of “” STEMCELLS””I am a vegetaeian and a firm beliver of natural health remedies………..i take an average of 16 vitanins a day……I don’t yet know what to use to cure and maybe destroy ..this lymphoma………ANY HELP WOULD BE VERY MUCH APPRECIATED..THANK YOU ONE AND ALL…………MARIO PS> I AM SEING A NEW ONCOLOGIST EARLY NEXT MONTH.
MY Mum had agressive chemo to treat cervical cancer, they also removed some of her bowel…6 months later its now in her bones and liver and her oncologist has told her that there is nothing else they can do – she wanted to try the Holt method of radio wave therapy but no one seems to practice this – what can you suggest – she is 64, always been fit and healthy -please, please can you help us, suggest something, anything
kind regards – Adele
ReplyHi Adele-
I am sorry to read of your mother’s metastatic cervical cancer. Since you expressed interest in the Holt Cancer Therapy and since you sound like you live in England, I have linked the Holt Foundation below. If you go to the website you can get the address and phone number of the foundation in Warrenton, England.
If you choose not to pursue the Holt therapy I can research and provide anti-colon therapies to include nutrition, supplementation, lifestyle and mind-body therapies all evidence based, researched to confirm they are cytotoxic (kill) colon cancer. I am a cancer coach as well as a long-term cancer survivor.
http://www.jhcancersupport.com
Thanks and give my best to your mom.
David Emerson
ReplyHi David,
My fiance has been diagnosed with adrenal carcinoma. It is in his esophagus and more. He is 62 yo.
Kim
Hi Kim-
I am sorry to read of your fiancee’s cancer diagnosis. If I read your email correctly, the cancer began in his esophagus and metastasized (spread) to one of his adrenal glands.
If the above it true then your situation is rare. Your fiancee is relatively young compared to the average cancer survivor and therefore has a lot to live for. However, the two of you may want unbiased support in thinking through the decisions you will face in the days and weeks ahead.
I am not experienced in this type of cancer. I do however encourage you to get a second opinion. Let me know if you have any questions.
David Emerson
ReplyI have recently been told about UMAC CORE phyton plankton to be effective but am still learning about it, are you aware of this product. It comes from British Columbia. I have had a ct scan on my left lung as they have found a small lump, but have not recieved the results yet, also lymph nodes in my throat are enlarged. I will not be doing any traditional cancer treatments as I don’t think the pain and suffering is what I want to do. I do know someone who was a client of mine who had stage 4 in her back and lung, she was on supplements and ate organic, and stayed away from proteins and sugar. She passed 1yr ago but had 7yrs of great quality of life with only one round of radiation, I want to follow her path. Her Dr. was Dr. Gonzales in New York and he uses supplements and purges.
ReplyHi Deb-
Please let me know if you are diagnosed with lung cancer. While phytoplankton, blue green algae, etc. are important immune boosting superfoods, there are supplements that research has shown to be cytotoxic to lung cancer. An example is milk thistle/silibinin.
While I understand not wanting to undergo traditional chemotherapy of any kind please understand that there are many integrative therapies that can both enhance the efficacy of a chemotherapy while reducing its toxicity.
My point is that you need to know your opinions to make the best decisions.
Let me know if I can help.
Hang in there,
David Emerson
ReplyMy mother is 85 years old and was in excellent health until 2/8/16 when she was found to have lesions/tumors in her brain. We opted for radiation of the brain, she does not want chemo and we did not want surgery before the radiation, the 2 tumors were large and causing confusion/dymentia like symptoms for her. They told us she could stroke out during surgery and we had to shrink the tumors quickly. After 14 radiation treatments, she is mentally back to normal, but is failing fast physically. The doctors were not sure if the tumors were lymphoma or an aggressive cancer. She had a body scan done and no other tumors were found in her chest, abdomen or pelvic areas. I find it difficult to do nothing as she continues to fail, what would you suggest to get her stronger? How would you procede from here as far as treatment? We do have an MRI scheduled next week to look at her brain to see if the tumors are gone, we were told we had to wait until 2 months after her radiation ended so the brain could heal a bit.
ReplyHi Anne-
I am sorry to read of your mom’s cancer diagnosis. Without a specific diagnosis (brain cancer or lymphoma) it is difficult for me to give you any advice. I don’t believe there is any curative therapy available to you. Therefore your focus should be on quality of life-in my opinion.
I will not speak to you as a cancer coach but as a son/caregiver. If it was my mom I would work to do three things.
First of all, radiation is debilitating even to young people. I would try to boost her energy and immune system in every way. Healthy foods, immune boosting non-conventional therapies, restful sleep (melatonin), mild exercise if possible (walks around the block?). Lifestyle therapies.
Secondly I would learn about and pursue palliative therapy for my mom. There are physicians who specialize in managing the side effects of cancer. This is NOT hospice though you may need hospice care at some point. A growing number of studies show that early palliative care can result in longer lives.
Lastly I would try to figure out how my mom wanted to spend her time. I don’t think most people want to specifically talk about “end of life” pursuits but this is what I am thinking about. It might be as simple as spending time with family and friends. It might be something like talking to a sister or family member that your mom had a falling out with a long time ago.
Anne, I’ve worked with people who push toxic therapies on the parents they are caregiving in the hope for a “cure.” While I understand the desire or intention, I know enough about cancer to understand the limits of conventional cancer care. Aggressive treatment is highly toxic.
I hope this helps. Let me know if you have any questions.
David Emerson
Replydavid my wife has stage 4 colon cancershe had an mri and a cat scan and was found to have spread to her liver they want to give her 5 radiation treatments then cemo she is 76 and was very healthy and active.we need help
ReplyHi Jerry-
I am sorry to read of your wife’s metastatic colon cancer. Your wife’s health and active lifestyle should help her in the coming weeks and months.
I will be direct. I encourage you and your wife to take an integrative approach to her therapy. This means that she take supplements that research has shown can enhance her chemo and radiation while reducing its toxicity.
An example would be “integrative” therapy for a possible colon cancer chemotherapy called 5-FU.
Chemotherapy and radiation are needed to attack an advanced cancer and stage such as colon cancer stage 4. Yet, with out integrative therapies the toxicity that you wife endures will be difficult.
I would also recommend anti-angiogenic nutrition, lifestyle therapies and mind-body therapies, again, all evidence-based.
Let me know if you have any questions.
David Emerson
ReplyHi
Your responses are worthwhile intelligent guesses. My review us from having just gone thru treatment for prostrate cancer. And still getting ADT therapy and your comments to people with this cancer.
So after I get my mm diagnosis I will contact you.
Thanks. Steve
Hi David,/
I had breast cancer three years ago and had a mastectomy and four rounds of chemo. All seemed well. In February of this year I was diagnosed with colon cancer. Twelve inches of colon was removed, as well as, 23 lymph nodes which were all determined to be “clear.” Since I had had breast cancer before, a PET scan was performed to see if any other areas of cancer showed up. Sure enough, there is a small spot on my lung. The current plan is to do radiation for the lung.
A friend of mine told me about 35% food grade hydrogen peroxide taken with distilled water. Are you familiar with this? Another friend recommended alkaline water, and my cousin swears by a tea that he brews from a product he can only get on line. What are your thoughts?
Hi Nancy-
I am sorry to learn of your original BC diagnosis and doubly sorry to learn of either your BC metastasis (spread to your lung/colon) or secondary cancers. The good news is that the colon and lung cancers appear to be contained.
Since you asked, I will give you my thoughts. In short, you have a lot of work to do. It is my belief that you will need to employ both conventional (FDA approved) and non-conventional therapies in order to maintain the highest quality of life while you work for the greatest length of life. Any cancer can be curable.
As you can see from the links below, you have lots of information to consider.
I am both a long-term cancer survivor of an “incurable cancer” and a cancer coach. I can help you figure out your options. Yes, I ask for a reasonable donation to PeopleBeatingCancer, a 501c3 non-profit. This is a tax deductible donation and is fully refundable.
Beat cancer with 35% hydrogen peroxide
Is Alkaline Water Extra Healthy or a Hoax?
Let me know if you have any questions. Hang in there,
David Emerson
Replymy wife ( age 47 ) was diagnosed with stage four non small cell carcinoma lung cancer ,1 1/2 years ago. she has had some radiation, and has been on dna targeting ( one pill a night ) she is mostly stable, how ever she has some growth in her bones that gives her pain. they told us they cant cure her. ive been reading about linus pauling, but I cant find anything about the dosages of vitamin c she should take interveiniously. if you can help me , I will be greatful.
ReplyHi Chris-
I am sorry to read of your wife’s NSCLC diagnosis. It is good to read, however that she is responding to DNA targeting therapy. I understand that conventional oncology does not have therapy that is curative for your wife but as a person who was also told he was terminal (in ’97), I believe that it is important to research and identify non-conventional (non FDA) evidence-based therapies.
Intravenous vitamin c therapy is one such therapy. Yes, there are studies citing its success yet it has not been approved by the FDA. The clinic that provides int. vit. c therapy will determine the doses for your wife based on her weight.
Anti-lung cancer supplementation, nutrition, lifestyle therapies, mind-body therapies, should all have a place in your wife’s treatment. I am a cancer coach who has been providing this type of research to hundred’s of cancer patients for years.
Let me know if you have any questions.
David Emerson
Replyfemale, 72 , breast cancer + lymph nodules in armpit. Metastasis to head of femur, radiation and FASLODEX +BONEFOS FOR 2 YEARS. Mid 2014process of metastasis reactivated, to other places of thje skeleton.
2015 frustrated attemts with PALBOCICLIB, XELODA, FEMARA.
Since December 2015 TAXOL, which after 9 sessions of reduced dosis (137mg), reduced a bit the level of absorption of the stuff ingested/inoculated before the PET-CT. Was told to go on with treatment until it stops working OR my body can not bear the side effects anymore. Any suggestions? Thanks
Hi Flora-
I am sorry to read that your breast cancer has metastasized to your bones. I don’t mean to sound alarmist in any way but I encourage you to think beyond conventional oncology. I do not mean for you should chase therapies that are not evidence-based. I will offer therapies and studies below.
My primary suggestion is that you take an “integrative” approach to your treatment. Supplement with those antioxidants that studies have shown will enhance chemotherapy (taxol in this case) while reducing its toxicity. An example of this integrative approach to taxol (paclitaxel) would be curcumin.
Further, please learn about and consider anti-BC lifestyle, nutrition, and mind-body therapies. Again, those supported by studies. I can send you information about all the above. I am a long-term cancer survivor myself and coach cancer patients. Yes, I charge money but the registration fee modest ($149) and is a tax-deductible donation to PeopleBeatingCancer, a registered 501c3 nonprofit. The fee is one time only and is fully refundable.
Let me know if you have any questions. Hang in there,
David Emerson
Cancer Survivor, Cancer Coach
Hi David
My name is Kimberly and I have been diagnosed with breast and Lymph node cancer, grade 3, stage 3A. My chances of it reoccurring without treatment I am told is 70% and half that if I get Chemo and Radiation. My treatment would be 8 treatments of Chemo aggressively and 25 treatments of radiation after Chemo. I am scared. I have had surgery and he took out the tumor from the breast 1.7 cm and 20 lymph nodes and 4 lymph nodes where cancer as well and 1 lymphnode had a tumor of 1.8 both oncologists, and my natural path doctor is saying I need to do this or its a great possibility that this cancer will come back. 🙁
HI Kimberly-
I am sorry to learn of your breast cancer diagnosis. While I agree with your staging of 3A your diagnostic specifics (tumor size, lymph node involvement) indicate that you are early or just barely 3A. Yes, you have a significant risk of recurrence but with the right multimodal mix of therapies you will greatly reduce your chances of relapse.
Chemo and radiation are toxic therapies and will lead to side effects if you do not learn about integrative therapies to both enhance efficacy and reduce toxicity.
Examples of integrative therapies for a typical breast cancer chemotherapy, docetaxel for instance, is curcumin.
In addition I recommend evidence-based nutritional, anti-BC supplementation, anti-BC lifestyle therapies- all evidence-based meaning all these therapies have been researched and provide studies to read.
My point Kimberly, is that your oncologists and naturopath are correct. Your stage does have a high risk of relapse. That is why I am encouraging you to include those therapies that studies have shown are cytotoxic to breast cancer and reduce the risk of relapse.
Let me know if you have any questions.
thanks and hang in there,
David Emerson
Cancer Survivor, Cancer Coach
Hi David
My name is Kimberly and I have been diagnosed with breast and Lymph node cancer, grade 3, stage 3A. My chances of it reoccurring without treatment I am told is 70% and half that if I get Chemo and Radiation. My treatment would be 8 treatments of Chemo aggressively and 25 treatments of radiation after Chemo. I am scared. I have had surgery and he took out the tumor from the breast 1.7 cm and 20 lymph nodes and 4 lymph nodes where cancer as well and 1 lymphnode had a tumor of 1.8 both oncologists, and my natural path doctor is saying I need to do this or its a great possibility that this cancer will come back. 🙁
Thank you for the information, I really do appreciate it. Can you tell me how you’ve become so knowledgeable about the different types of cancers. And I will be looking at the therapies you have sent me. My Natural path has set me up with
Theracurmin-Pro 600 Melatonin working up to 20mg, Coriolus, and a multistrain probiotic. Before surgery she set me up with 4 homeopathy remedies, and after I was on arnica and a couple of others. For emotional support. Also I use essential oils and a good diet, alkaline diet. When I first found out about my cancer, I tried to shrink the tumors with DMSO and a mixture of sodium clorite and citric acid. There was a small difference in size. This method seems to do something but it takes time. This type of cancer doesn’t have that time, but I did what I could until conventional kicked in. Again thanks for the advice. Everything helps.
Hi David
Are the therapies you are talking about a multi b source, I looked it up on google and I got lost in the language. Can you explain to me a little clearer the supplementation and lifestyle of anti BC.
ReplyHi Kimberly-
I would have to do more research but examples would be supplementation or nutrition that studies indicate are cytotoxic to BC. Your nat. path. recommended theracumin because it kills BC. Actually, curcumin kills BC. Theracumin is a specific formula that studies show is more bioavailable that other curcumin formulas.
Curcumin induces apoptosis in human breast cancer cells through p53-dependent Bax induction
An example of a lifestyle therapy that reduces the risk of BC relapse would be frequent, moderate exercise. Both of these therapies are true for MM as well.
David
ReplyHit with a PSA of 1,666 first week of 2016. Obviously been growing for a while, metastasis
of spine, legs, neck, etc.
Taking Degarelix (Firmagon) got PSA down to 8.4. Dr. is now saying chemo is next step, which I want to avoid at all costs (only as last resort).
Where is a good place to go for immunotherapy? Suggestions regarding diet? I am a vegetarian. Eat eggs and fish for protein.
Supplements?
ReplyHi Frank,
I will be direct with you. I am a cancer coach. Your situation is complex. Not impossible but there is a lot to do.
I am sorry to read of your prostate cancer (PCa) diagnosis but I am glad to read that you have responded so well to Degarelix. I agree that you should avoid the toxicity of chemotherapy “at all costs” but keep in mind that your options will be limited with a diagnosis of metastasized prostate cancer.
My point is that you may want to throw all evidence-based therapies at your cancer as you can in an effort to live as long and as well as you can. In my experience, the spectrum of therapies can include chemo, nutrition, non-toxic supplementation, and maybe even some careful local radiation.
Since you are currently undergoing a chemo treatment your next steps are to:
1) Understand the possible FDA approved chemotherapies for PCa- Docetaxel (Taxotere) Cabazitaxel (Jevtana) Mitoxantrone (Novantrone)
Estramustine (Emcyt) for example. All have strengths and weaknesses. All cause short, long-term and possibly late stage side effects. Understanding the possible side effects will enable you to take therapies to either reduce or prevent the collateral damage caused by a specific chemotherapy. An example would be the peripheral neuropathy (tingling, burning) caused by taxotere. Supplementing with omega 3 fatty acids may reduce or eliminates the damaging affects of taxotere.
2) Understand those therapies that are “integrative” to those FDA approved anti-PCa chemo therapies. An example would be the supplement curcumin enhancing taxotere (docletaxel).
3) Understand those non-conventional therapies that studies have shown are cytotoxic (kill) PCa. An example would be green tea extract
4) Understand anti-PCA nutritional therapies- again evidence-based.
5) Understanding those lifestyle based therapies that either promote bone health or are cytotoxic to PCa.
6) Understanding evidence-based mind-body therapies that are anti-cancer. These therapies may seem a bit touchy-feely to some people but my role as cancer coach is to do the research, present the information to you and let you decide.
If you would like evidence-based research about the above therapies please consider hiring me as your cancer coach. To learn more go to-
PeopleBeatingCancerCoaching.org
Let me know if you have any questions.
thanks and hang in there,
David Emerson
ReplyI have DCIS with microinvasion 1 had lumpectomey and lymph nodes removed everything looks good…Is there stilll a need for radiatin? Thanks
ReplyHi Karen-
Your question ” lumpectomey and lymph nodes removed everything looks good…Is there stilll a need for radiation?” continues to be debated. My personal belief is that local radiation causes as many risks as benefits. But I am not a BC survivor so I can’t say. Please consider having an Oncotype DX assay performed. You will receive a score that will help you decide whether or not to undergo local radiation.
Please consider undergoing those antioxidant supplements, anti-angiogenic nutritional and lifestyle therapies that studies have shown reduce the risk of breast cancer relapse.
David Emerson
Survivor, Cancer Coach
I am 67 and had a hysterectomy 1 year ago, went through radiation last summer and now cancer has spread to other organs. Trying to find a good place in US for alternative cancer treatments to get rid of this nasty disease. Can you help?
ReplyHi Pat-
I am sorry to read of your cancer. I’m not sure what you are asking me. Yes, I can research and identify US clinics that administer therapies such as Insulin Potentiation Therapy (IPT). The first step however is for you to consider those conventional and non-conventional therapies to help you manage your cancer.
In order to provide this information I need to know what cancer and stage you have been diagnosed with/at. Let me know if you want to talk further.
thanks,
David Emerson
Survivor, Cancer Coach
Hello I have a prostate 17 count. A biopsy shows cancer. Doctor says removal of prostate and potential radiation. Whats your opinion as I know a bit about herbals as my wife is a herbalist retired. I am 64 yrs old in good health otherwise.
ReplyHi Eugene-
When you say “prostate of 17 count.” I will assume that you mean you PSA test (prostate specific antigen) indicated a score of 17. The 3 forum post linked below convey that this PSA level is high but not that high.
When you say that a “biopsy shows cancer” it’s important to note two things. First, most of us over the age of 50 have some cancer growing inside our prostates. Second, the issue then is 1) how MUCH cancer is inside your prostate and 2) how FAST is the cancer growing.
To determine how much cancer and how fast is your cancer growing, your physician should be able to tell you how many of the cores taken during your biopsy showed cancer. For example, if half of the cores taken during your biopsy showed cancer then your cancer is half as big as your prostate.
To speak to your question about herbals, yes there are many non-conventional therapies, including herbal supplements that studied show slow or kill prostate cancer. Further, there are studies that also cite anti-prostate cancer nutrition and lifestyle therapies to also kill cancer.
Eugene, please understand that there will be considerable collateral damage caused by prostatectomy (prostate removal) and radiation. Permanent damage such as urinary incontinence and or erectile disfunction among others.
The issue then, is to balance your risks with potential side effects. If you can tell me how many “cores” showed cancer I can provide studies that will offer several different therapies to you all that have different levels of risks/ collateral damage.
If the amount of cancer that is in your prostate then you can watch and wait and undergo non-conventional therapies such as herbal therapies, antioxidant supplements, nutrition and lifestyle supplements.
My point is that I will provide studies so that you and your wife can make the decisions.
Let me know what you think. David Emerson
ReplyThanks for your caring David, 54 year old male, could loose 20 pounds. On digital exam urologist found a small lump on my DRE. I freaked and paid for a MRI (I am Canadian and didnt want to wait in line so I paid). The findings in my MRI:
Radialogist IMPRESSION: 9×5 mm focal lesion seen in the medial right base peripheral zone could represent tumour. PI-RADS 4
I had biopsy – non-specific and all negative.
One year later, no change in the tumour, PSA in NOV2014 0.39/DEC2015 0.26
Now they want me to go have a direct biopsy of the tumour. Is there a chance the needle poke can cause spreading of the cancer cells (
I feel I should leave it for now because everything seems so fine, but I have a lot of living to do and don’t want in 5-10 years someone tell me that I should have had it removed.
Being this small what do you think about that radiation pin pointing ray thing-a-ma-bob work?
your opinion)?
Also In 5 years they can be disclosing NEW treatments rather than radical prostate removal surgery.
Thanks for your time David!!!
Rick
All other blood work is spot on NORMAL 🙂
ReplyHi Rick-
Normally I begin my cancer coaching comments with the words “I am sorry to read of…” but in your case you have not be diagnosed with cancer. Frankly I don’t think you have anything to worry about but let me present my thinking below.
Let me respond to several of your diagnostic issues and then reply to your questions below. As you probably know, all of your diagnostic testing pointed to little if anything for you to worry about. Your PSA of 12/15, 0.26 is lower than 11/14 and is lower than mine…Granted, a PSA test is not a perfect test. But a PSA level of less than 1 is pretty good. Also a non-specific biopsy and normal blood work is pretty good news too.
It is important to note that most men over 50 (I’m 56) have some sort of lesion growing in their prostate. The question for all of us is whether or not the cells in our prostate will turn aggressive…in our lifetime. Will we die of prostate cancer or something else?
The only diagnostic indicator that possibly raises a red flag in this regard is your PI-RADS level of 4.
“PI-RADS 4: high (clinically significant cancer is likely to be present)”
I will lay out your therapy choices below:
1) Watchful waiting. No side effects other than possibly worrying. There are a host of inexpensive, evidence-based, non-toxic therapies shown to reduce the risk of prostate cancer. I take several of these myself. I have prostate cancer in my family…
2) HIFU therapy- this form of therapy was recently approved by the FDA in the US. I don’t know about Canada. Minimal side effects, non-toxic. Worth understanding. I can research the who, what and where is you are interested in learning more about this therapy.
3) Radiation- yes, several possible long-term side effects. You need to understand the pros and cons of this therapy.
4) “direct biopsy of the tumour” another diagnostic test depending on the course of therapy. Unlikely to spread cancer but yes, there are documented side effects from biopsies. Further, the main benefit of prostate biopsies is to measure growth of a tumour over time. One biopsy only tells you how big the lesion inside you is. Not how aggressive it is.
Rick, I think you are okay for now but if you would like to learn more about any or all of the issues in 1-4, please register to become a cancer coaching patient by clicking the blue button-
I hope to talk with you further. Thanks and hang in there.
David Emerson
ReplyMy father was diagnosed with bladder cancer on new years eve. He had a kidney transplant year and half ago. We are not exactly sure what to do for treatment, can you please help in determining who would be the best person to talk to for conventional and non conventional treatment?
Thank you
ReplyHi Sap-
I am sorry to learn of your father’s bladder cancer diagnosis. Your choices of both conventional and non-conventional therapies will depend on several factors. I can make specific recommendations based on your answers to the questions below.
1) what stage is your dad’s bladder cancer? As you can read from this explanation, early stage bladder cancer is treated much differently then late stage bladder cancer.
2) what, if any, are his symtoms? How does he feel?
3) You mentioned that your dad has a kidney transplant 1.5 years ago. What is health like? How old is your dad?
To put my questions into perspective, I talked with a man recently who had his bladder removed. Tom had extensive surgery but has recovered well. On the other had, if your dad diagnosis is early stage bladder cancer (see the study linked and excerpted below), your dad’s treatment options will be much different.
Non-muscle invasive bladder cancer risk stratification.
“Non-muscle invasive bladder cancer (NMIBC) comprises about 70% of all newly diagnosed bladder cancer, and includes tumors with stage Ta, T1 and carcinoma in situ (CIS.)…”
I will try to address your questions based on the info you relay to my questions. Thanks.
David Emerson
ReplyHI THERE
i have Papillary thyroid cancer for one year so far and i did blood test which is CEA and back normal,nothing in my blood , but biopsy said i have cancer I’m on natural bath and doing good. tumor was 2.3 now 1.7 .i have anther one but not cancerous .same size .nodule.
But doctors keep pushing me for surgery and radiation which im not going with ,and saying tumor will not go away .
your advice pleae .
what do you have for this cancer .
and biosey can be wrong ?
I dont believe it is cancer .im doing very good.
Thanks
sue
Hi Sue-
While a normal CEA blood test is positive it is not completely conclusive. Please read the content about CEA levels linked and excerpted below.
I’m not sure what you are saying in the sentence ” but biopsy said i have cancer I’m on natural bath and doing good. tumor was 2.3 now 1.7 .i have anther one but not cancerous .same size .nodule.”
I think it is possible that you have a small tumor that may never be a health issue. Please understand that I cannot tell you what to do. I am not a medical doctor. Please read the article linked below that cites several studies that examine over diagnosis and over treatment in thyroid cancer.
Thyroid cancer over-diagnosis and over-treatment- do you care?
“What are the limitations of CEA testing?
CEA is not an effective screening test for hidden (occult) cancer since early tumors do not cause significant blood elevations. Also, many tumors never cause an abnormal blood level, even in advanced disease. Because there is variability between results obtained between laboratories, the same laboratory should do repeat testing when monitoring a patient with cancer”
Let me know if you have any questions.
Thank you,
David Emerson
ReplyThank you for your website.
I was diagnosed in 9/22/15 with Adenocarcinoma after losing 30 lbs since May 2015 (thought stress).
Since diagnosis I have had 23 treatments of radiation and 5 rounds of chemo. I was on a feeding tube for 2 months.
After the 30 day waiting period, my new scan showed a couple of new cysts on my liver.
My oncologist has now ruled out the esophagectomy and intestinal resection that had been planned.
She wants to start a new palliative rounds of 3 types of chemo on Jan 4, 2016.
She says worst case is a few months but 1-2 years with the new chemo.
Should I go somewhere else for a second opinion? Should I try hemp oil as an alternative? How can I find out if there are trials/options overseas?
Many thanks in advance.
Also, I am 55 y/o and had a gastric sleeve in March 2011. I apparently suffered from silent acid reflux and had absolutely no clue of my problems until I started throwing up. The first biopsy in July came back benign.
Hi Anita-
I am sorry to learn of your adenocarcinoma. In order for me to research possible therapies for you I must confirm a few things.
1) Am I correct in thinking that your diagnosis is “esophageal adenocarcinoma (EAC)?
2) What stage was your original diagnosis?
3) How is your health otherwise?
Answers to your questions above until I get additional info are 1) therapies to boost your immune health such as CBD/Hemp oil, frequent, moderate exercise, anti-cancer nutrition/diet, antioxidant supplements in general are good therapies for cancer patients undergoing aggressive therapies such as chemo and radiation. 2) a second opinion is always a good idea. Your prognosis is difficult to determine at this point in time. Talking to another oncologist may help you think through your options.
Thirdly, palliative therapies, in general, are a good idea at this stage in your cancer experience. Please keep in mind that palliative therapies do NOT preclude curative therapies if you choose. Palliative therapies are simply directed at managing your side effects or symptoms.
As for overseas therapy options, I can research possible options if you would like. As an example, I researched clinics in Germany and Mexico when I was told that my onc. had nothing more to offer me back in ’97.
Please answer the questions above if you would like me to provide more info for you.
In the meantime, hang in there.
David Emerson
Replythank you for responding so quickly!
My esophageal cancer is located at my lower esophageal sphincter…the reason for my feeding tube for the two months. The treatments shrunk the tumor and I am able to eat soft foods and some other limited things. I was told not to eat meat because it would be too hard but wonder if I could purée some chicken salad…
I was staged at Stage 2 with 0 node and 0 metastasis is. I was told at my follow up that I was not told originally that I had a couple of liver cysts but that a couple of more had developed and that concerned them. The biopsy revealed the cancer had metasticized to my liver and she wanted to start the palliative chemo Jan 4.
I tend to be weary. Before diagnosis, I worked almost 70 hours a week – 8-4:30 day job and 5:30-11:00 at my night job. After 15 years of this schedule, I thiught I was just wearing out!
After the feeding tube was removed, I was told to drink Boost and anything else I could tolerate for the calories….no specific diet to increase my immune system nor “fight” cancer.
I have purchased a Ninja to blend kale and berries that my ex-husband brought me so as soon as I send this I will add that to my diet….mashed potatoes and green beans can only add so much! And it’s so weird, some days I can keep the beans down, some days I can’t.
would I have to go to Colorado for hemp oil? I know both Alabama (residence) and Tennessee (Vandy hospital) have seizure studies for hemp oil but which states have cancer studies?
I appreciate your site and responses to everyone and can only tell you that I want to be around for my grandchildren (13,8,3) for a while longer….my 3 y/o grandson would only know from pictures. So thank you for the information and the hope….I do know it’s not guaranteed but hope is a wonderful thing 🙂
Hi Anita-
Thank you for the additional information about your EC. I will enumerate the issues below in my attempt to answer your questions.
1) “The biopsy revealed the cancer had metasticized to my liver and she wanted to start the palliative chemo Jan 4.” Yes, the liver cysts indicate that your EC has spread. Palliative chemo is given to minimize side effects or the symptoms of your EC. What side effects or symptoms is your onc. worrying about?
2) “I tend to be weary. Before diagnosis, I worked almost 70 hours a week – 8-4:30 day job and 5:30-11:00 at my night job. After 15 years of this schedule, I thiught I was just wearing out!”
In my humble opinion you should not be trying to work long hours while you are healing from cancer therapy all the time trying to rid your body of cancer…
3) “I have purchased a Ninja to blend kale and berries that my ex-husband brought me so as soon as I send this I will add that to my diet” I too have a ninja. I recommend a smoothie at least once a day. If you cannot eat solid foods you must figure out a way to get nutrition into you system.
4) “would I have to go to Colorado for hemp oil? I know both Alabama (residence) and Tennessee (Vandy hospital) have seizure studies for hemp oil but which states have cancer studies?”
The hemp oil that we can purchase online does not have either the CBD or THC content that studies have shown will fight cancer. You are correct, only states where medical marijuana is legal will sell CBD oil with CBD and THC.
5) “I appreciate your site and responses to everyone and can only tell you that I want to be around for my grandchildren (13,8,3) for a while longer”
I encourage you to fight your cancer with every tool you can find. Nutrition (smoothies), antioxidant supplementation such as curcumin, resveritrol, green tea extract, omega 3 fatty acids, milk thistle (I take these supplements myself-daily). I recommend daily, moderate exercise, plenty of sleep (melatonin) and laugh a lot.
Please reply with any/all questions.
Hang in there
David Emerson
ReplyHi David;
My 30 year old brother was diagnosed with Follicular Mycosis fongoides 2 years ago. At first they though it was Mycosis fongoides but after 6 months of therapy which includes phototherapy there was no result (he was told there is no need for chemo in his case) and he was told that was an aggrassive form which is called Follicular mycosis fongoides. He started having big patches all over his body including some tumors on the bottom of his leg. then they put him on Acutan and interferon for another 6 months yet the result was not impressing. After all this time now he is asked to start radiation for 3 weeks on a daily basis following that he would need a chemoteraphy and then stem cell transplant. I was wondering what your opinion would be on that? ! I honestly don’t know who is right and can’t trust them no more. I appreciate your help. Thanks alot
ReplyHi Lida-
I am sorry to learn of your brother’s Follicular mycosis fongoides. A cancer diagnosis is difficult and a diagnosis of a rare cancer is even more so. The reason why you don’t feel as if you can trust your oncologists, in my opinion, is because this is a rare form of cancer. As such, there is little research, little experience for your oncs. to follow.
The therapy path that you describe- phototherapy, acetone, interferon and then more aggressive therapies such as radiation and chemotherapy and possibly a SCT is the path of therapy that is outlined in my research of this form of t-cell lymphoma.
The only opinion I can offer is to find an oncologist who is as experienced with Follicular mycosis fongoides as possible. My suggestion would be to talk to a cancer center with experience in blood cancers (hematology/oncology). My suggestion would be to search the Dana-Farber website for oncs who have experience with your brother’s cancer.
To be clear, I am not saying that your current oncs are incorrect with their therapy recommendations. If a phone consult with an experienced hem/onc. at Dana-Farber reveals similar info as what you have already done then you can have confidence in your current oncs.
Please don’t hesitate to ask me additional questions.
David Emerson
ReplyMy mom has colon cancer. She had about a foot of her colon removed. She is now going thru chemo. I saw a video about a drug that is quit old, called DCA. In tests done in mice, it showed that DCA forces the cancer cells to basically commit suicide. The problem is that no drug company owns the patent for it. I was wondering what could be done to have the cancer foundations to research this drug. They keep advertising on TV all these cancer foundations and such. Yet noone actually want a cure. So what could be done, through petitions etc., to have people act on these easy cures?
ReplyI meant the foundation to act on funding research for those easy cures.
ReplyHi Borbor-
When you talk about “easy cures” or specific therapies such as DCA you are highlighting one of the greatest debates in cancer care today. You are correct when you say that Foundations frequently talk about “research” but then don’t do any research on those therapies that are controversial.
As for your question “So what could be done, through petitions etc., to have people act on these easy cures?” I can only tell you what I do in response to my own cancer, multiple myeloma.
Though I have been cancer-free since ’99 I live with the idea that my cancer may relapse someday. I pursue many lifestyle therapies and I suggest that your mom pursues these anti cancer lifestyle as well. Your mom’s risk of relapse after her chemotherapy ends will continue to be significant for years to come.
The anti-cancer lifestyle therapies that I do and recommend are 1) daily, moderate exercise (brisk walk around the block each day kind of thing…), 2) anti-cancer nutrition (no smoking, no alcohol, little processed sugar, etc.), 3) antioxidant nutritional supplementation with curcumin, resveritrol, green tea extract, omega 3 fatty acids (all can be purchases on Amazon.com), some sort of mind-body therapy such as yoga, mediation, sleep (melatonin), spirituality, etc.
All the therapies that I talk about above are evidence-based with studies to support their anti-cancer action.
Yes, I wish there was more research on non-conventional therapies like DCA. Until there is your mom and I will have to do our own research and pursue our own therapies.
Let me know if you have any questions. Good luck and hang in there.
David Emerson
ReplyHi thank you for your work and guide to lost souls like me. Tomorrow it will be 5 years I had surgery for the removal of my stomach ..entire stomach. It has been a journey as the side effects, constant pain , loss of 65 lbs as I was not that over weight to begin with 165 lbs. , loss of appetite and many others making it difficult to work thus loss of clients.
In any event I had an endoscopy done about 6 months ago and based on those results my oncologist has advised I am cancer free. I am not convinced though I would like t be. When should I have my next endoscopy, or scan or whatever objectively determines that the cancer is gone. How do I know I d not hhave cancer of the stomach and or any kind of cancer in the event that it may have spread on attacked differ organs or part of the body.
I would like to be worrisome free , if possible and thus what should I do to firmly say : I AM CANCER FREE.
Thanks in advance for your time and interest. Gaetano
ReplyHi Gaetano-
I am sorry to learn of your cancer issues but I disagree with your appraisal of yourself as “…lost souls like me.” You have managed to weather five years with a difficult “new normal.” In my book this fact puts you above most healthy people.
In answer to your questions above, I will innumerate and address each below-
1) “When should I have my next endoscopy, or scan or whatever objectively determines that the cancer is gone” The frequency of your testing is up to your oncologist. He/she has the full knowledge of your cancer- diagnosis, treatment, etc.
2) “How do I know I d not hhave cancer of the stomach and or any kind of cancer in the event that it may have spread on attacked differ organs or part of the body.” I do not know of any cancer that is guaranteed not to relapse. My own cancer, multiple myeloma, always relapses and is considered to be incurable by conventional oncology.
I live my life as if my cancer may relapse someday though I have been cancer-free since 1999. Please understand me. I do consider myself to be CANCER-FREE. However I think you and I must live an anti-cancer lifestyle.
There are many studies that cite the fact that moderate, frequent exercise (walking, swimming, etc.) reduces the risk of relapse. Your weight loss, while difficult, also greatly reduces the risk of relapse. Antioxidant supplementation with curcumin, omega 3 fatty acids, green tea extract, and resveritrol all lower the risks of many cancers. These nutritional supplements probably lower your own risk of relapse too.
I do all the lifestyle therapies above and I encourage you to do the same to lower your own risk of relapse. Lastly, in your case, I would add nutritional support. I have no study to point to for cancer survivors who have had their stomach removed but I have to believe that your body’s ability to get nutritional support from the food you eat has been seriously impaired. As such you may be nutritionally deficient. I suggest WHOLE FOOD supplementation. Not synthetic vitamin supplementation.
I recommend Standard Process Supplements.
Please let me know if you have any questions. Hang in there.
David Emerson
ReplyNeedle biopsy of left kidney produced only a few ‘cells’. Ultrasound and CT scans used. Needle may have gone in a little ‘off’. Surgeon advises ‘keeping an eye’ on it. By ultrasound in 3 months. Small tumour. Your thoughts, please, would be so appreciated.
ReplyHi George-
I’m not exactly sure of what you are saying in your email so let me tell you what I think you are saying.
A needle biopsy of your left kidney indicated a “few cells (cancer)” and a small tumor. Since your surgical onc. did find a “few cells” he/she wants to keep an eye on you. You will have more diagnostic testing in three months.
if this thinking is correct, I want to share with you a regimen that I researched and sent to a RCC survivor who had recently relapsed.
The excerpt is below:
“Please consider quitting smoking if you do. Consider frequent, moderate exercise which over time may help you lose weight and lower your blood pressure. I don’t know what your job is but if you coming in contact with the chemicals listed above figure out how to avoid them.
My general point is that exercise, lifestyle, environment, etc. may slow or even reverse your RCC. I’m big on plan B thinking. If you do need chemo someday, you will be “pre-habilitated.” Meaning, you will be in better physical condition and therefore will handle chemo better.
Molecular mechanisms of curcumin-induced cytotoxicity: induction of apoptosis through generation of reactive oxygen species, down-regulation of Bcl-XL and IAP, the release of cytochrome c and inhibition of Akt.
Influence of curcumin on HOTAIR-mediated migration of human renal cell carcinoma cells.Modification of Antitumor Immunity and Tumor Microenvironment by Resveratrol in Mouse Renal Tumor Model
Please let me know if you have any questions about any of the information above.
David Emerson
ReplyHello Dr. My great grandmother is 87 years old and this year recently, 2015 she has been diagnosed with abdomen cancer. The cells are in all her organs, liver, cervix, kidney, etc and it’s spreading. The doctor says at her age she would be uneligible for surgery/ treatment. What is your opinion on this matter? I really want my great grandmother to live as long as possible and help please.
ReplyHi Ndia-
I am sorry to learn of your great grandmother’s (G.G.) cancer diagnosis. When you say “The cells are in all her organs, liver, cervix, kidney, etc and it’s spreading.” I take you to mean that your great grandmother has evidence of cancer, perhaps tumors or lesions, “all in her organs. I am saying this only to confirm that your great grandmother’s cancer has spread significantly. This evidence of metastasis indicates that her cancer is advanced.
When her onc. tells you that your G.G. is ineligible for surgery or other treatment he/she is saying that conventional cancer therapies will be too hard on your G.G. physically but the onc. is also saying that any conventional cancer treatment will do nothing to increase your G.G. length of life and will certainly decrease her quality of life.
Certainly I don’t know your G.G. Therefore it is impossible for me to give you any sort of prognosis. I based my thinking above only on what you have told me in your email. Yes, there are non-conventional therapies for you and your G.G. to consider. What I am saying, and what your onc. is saying is that advanced, metastatic cancer is extremely unlikely to be stopped, slowed or managed in any positive way.
Please believe me, if there where any therapies that I knew of that offered any reasonable hope of success I would be the first to offer them.
This is not my opinion but rather my experience based on many example of advanced cancers.
Please let me know if you have any questions.
David Emerson
ReplyI had a kidney removed in Feb of this yr due to papillary cell renal cell carcinoma. I was just diagnosed with metastatic rcc on my lungs. The nodules are too small to biopsy right now but it appears to be slow growing. My onc thinks treatment won’t begin for 12-18 months. I am pretty much in shock as my onc indicated a max 10 yr prognosis once he starts treatment. I’m 63 yrs old now and I feel like time is closing in on me. I have no idea how to deal with this dx. Can you give me some suggestions?
ReplyHi Jeff-
I am sorry to learn of your RCC diagnosis. I understand the shock of a cancer diagnosis or of a metastatic cancer diagnosis, however you have a number of factors in your favor. Read the info below with the understanding that in my own cancer case chemo/radiation/surgery did little for me. It was the pursuit of non-toxic therapies coupled with lifestyle therapies that put me into complete remission where I remain today. Being told that a cancer is incurable (as my cancer is, multiple myeloma) is depressing to be sure. But keep in mind that this statement only means that the onc. sitting across from you doesn’t know how to treat your cancer for the long term.
Take a deep breath and begin learning about those therapies that are available to you.
First and foremost “small, slow growing” nodules is a positive. You can use the 12-18 months to learn about and pursue non-toxic therapies. As the studies linked below indicate, there are numerous antioxidant supplements that show evidence-based RCC killing ability. Further, all of the antioxidants discussed below are low-cost and can be purchased through Amazon. I buy all my supplement online…
I take all below though at a lower maintenance dose as I have been taking them for years now.
“…Lifestyle[edit]
The greatest risk factors for RCC are lifestyle-related; smoking, obesity and hypertension (high blood pressure) have been estimated to account for up to 50% of cases.[13] Occupational exposure to some chemicals such as asbestos, cadmium, lead, chlorinated solvents, petrochemicals and PAH (polycyclic aromatic hydrocarbon) has been examined by multiple studies with inconclusive results.[14][15][16] Another suspected risk factor is the long term use of non-steroidal anti-inflammatory drugs (NSAIDS).[17]”
Please consider quitting smoking if you do. Consider frequent, moderate exercise which over time may help you lose weight and lower your blood pressure. I don’t know what your job is but if you coming in contact with the chemicals listed above figure out how to avoid them.
My general point is that exercise, lifestyle, environment, etc. may slow or even reverse your RCC. I’m big on plan B thinking. If you do need chemo someday, you will be “pre-habilitated.” Meaning, you will be in better physical condition and therefore will handle chemo better.
Molecular mechanisms of curcumin-induced cytotoxicity: induction of apoptosis through generation of reactive oxygen species, down-regulation of Bcl-XL and IAP, the release of cytochrome c and inhibition of Akt.
Influence of curcumin on HOTAIR-mediated migration of human renal cell carcinoma cells.
Modification of Antitumor Immunity and Tumor Microenvironment by Resveratrol in Mouse Renal Tumor Model
Milk Thistle
Omega 3 fatty acids and RCC-
Please let me know if you have any questions about any of the information above.
David Emerson
ReplyDavid,
Thanks so much for the information. I have never smoked, can’t take nsaids because of an allergy and am now retired. I will be getting the supplements you recommend and begin my own journey to beat this disease. I will be a regular reader of your site.
Hi Jeff-
All good. Please read all the studies that I linked. I try not to simply tell people what I do and what I think they should do. I think it is important for cancer patients and survivors to understand what they are doing and why they may or may not follow a given therapy.
Good luck and please keep in touch.
thanks
David
ReplyHow do I know what dosage of these supplements are right for me? It appears there are a myriad of choices. Should I just pick one at random or choose the largest dose? How do you decide?
ReplyDavid thank you for all the good advice you give to help others think about dealing with their cancer another way. My friend was diagnosed with breast cancer a little over 2 years ago. She underwent chemo and had a mastectomy of one of her breast. Back in January she developed a bad cough and her doctor ran test and did a chest X-Ray to rule out lung cancer. It came back negative. However six months later she still had the cough. She finally changed doctors and the new doctor discovered she had neck cancer. She started back with chemo and was responding very good. Just a couple of days ago she started complaining of headaches and was not able to get up. Her family took her to the hospital. After running test she was diagnosed with brain cancer. It is all over in her brain, everywhere. Do you have any suggestions as to some other alternatives she can do. The doctors have told her and the family that radiation therapy will buy her about 2 months fo live. Please help.
ReplyHi CS-
I am sorry for your friend’s cancer difficulties. Based on your email I have to make a few assumptions. I am assuming that your friend’s breast cancer (BC) was treated but has metastasized. I am assuming that your friend’s original doctor missed the early spread of breast cancer to her lungs. A second opinion found your friend’s BC had metastasized to esophageal cancer. Treatment for metastatic BC was going well but she found out a few days ago that the BC has spread to her brain.
Your question to me is if there are any therapies available to your friend?
I agree that radiation to your friend’s brain will buy little if any length of life while causing extensive collateral damage severely limiting her quality of life. Surgery is out as a therapy as well.
At this point I can only confirm what you already know. And that is your friend’s situation is very serious. While you and her family’s instinct is to push more therapy on your friend, such as chemo and radiation, the reality is that toxic therapy will only limit quality of life while minimizing quantity of life.
It is important for me to tell you that I have no personal experience with those systemic or whole body therapies that I can discuss with you. I do a great deal of research on the Internet and have read about several non-conventional therapies that may or may not help your friend.
You may want to learn about and consider pain management in the form of both opioids as well as medical marijuana- both cannabidiol and THC. My understanding is that MM helps manage pain as well as has anti-cancer properties. Since I don’t know where your friend lives I cannot speak to where or how you might source the MM.
Also, please learn about and consider a systemic or whole body therapy called PolyMVA.
Please read up on and consider Ketogenic Diet and Hyperbaric Oxygen Therapy as Cancer therapy-
Please read up on and consider Avemar cancer therapy
Please read up on and consider Intravenous Vitamin C therapy-
CS- the above non-conventional therapies are relatively simple, depending on where you live, and should be relatively cost-effetive. Again, much depends on where you live.
Please let me know if you have any questions.
Hang in there,
David Emerson
ReplyHi, David. I’m wondering if you have any suggestions for me. I was diagnosed with malignant melanoma. A 7mm tumor was removed from my hairline (behind my ear and directly above my shoulder). My hairdresser noticed a bump there 10-15 years ago. I’ve had it checked over the years, but the doctors thought it was a plugged hair follicle. I had terrible pain going down my shoulder and into my bowel on my right side for all those years. I would ask if something could be pressing on a nerve, maybe even that little bump, and the doctors always said no. Finally I decided to get it removed because I was noticing it when I combed my hair. I thought I was being vain. I had a pre-op and ultrasound to check it and everything pointed to a plugged hair follicle or cyst. The results came back malignant melanoma. Interestingly I had no pain in my shoulder or bowel after it was removed. I needed a larger surgery and skin graft because the margin was positive, but no ulceration. That neck surgeon said that the tumor had indeed been pressing on a nerve. My oncologist suggested interferon (only a 5% or less chance to boost immunity) and possible radiation. The CT scan did not show any masses, as they expected, and it did not get into the lymph system. I live in western Canada. I do not want to do the interferon as my surgeon told me I would be offered but it would make me very sick and would not extent my life. I think my husband understands my decision. I just think there are other options. Any suggestions would be helpful!
ReplyHi Bren-
I am sorry to learn of your malignant melanoma diagnosis. I have limited experience with the Canadian medical system so my suggestion may or may not be available to you. I hope that’s okay with you. Further, I am not a medical doctor. I am a long term cancer survivor who has been studying cancer since 1999.
You should read about and possibly undergo several new immunotherapies- Opdivo, Keytruda,Yervoy Your response will depend on the genetic or molecular make-up of your melanoma. I will link info below. All these therapies are new and not well understood by oncology.
Further, I understand that Cannabis oil or CBD oil is legal in Canada. This therapy is not well researched here in the states. I am only offering CBD oil as your therapies are limited and you may want to learn more about this option.
FDA Approves Nivolumab (Opdivo) for Advanced Melanoma
As for non-conventional therapies,
Cannabis Oil for melanoma
There benefit of antioxidant supplementation for melanoma is controversial. Therefore I cannot recommend anything here.
Let me know if you have any questions.
thanks
David Emerson
ReplyIn August 2015, my 64 year old husband was diagnosed with Stage 4 Melanoma metastized to the stomach. He had malignant chroidal melanoma (ocular) cancer in 2001, which resulted in the removal of his left eye. They followed him for 5 year to check to see that there was no leakage of any cancer from the optic nerve. When none was ever found, the oncologist released him and life has been good. So when it reappeared in August, we were stunned. They gave him 10 weeks of Opdivo/Nivolumab and when they did a follow-up cat scan, they said the medicine did not work at all, he had more tumors and now some fluid in the lungs. Again stunned as they said this was a miracle drug, though they were careful not to promise anything. They did assure us that it was not genetic, and just a freak of nature. It may as well have been water. Plan B, and the last option, is to try Mekinist/Trammetinib, but so far the insurance company has denied it, so we are now in the appeal process. We were able to do some research and get some of the CBD oil and he has been using it for 2 days now. Any thoughts, suggestions you can provide would be appreciated.
ReplyHi Karen-
I am sorry to read of your husband’s cancer diagnosis. In response to your question “We were able to do some research and get some of the CBD oil and he has been using it for 2 days now. Any thoughts, suggestions you can provide would be appreciated” there are several difficult issues regarding medical marijuana, cannibis, canabidiol, CBD, etc.
As you know MM is still illegal on the federal level in the US. Therefore, there is little if any cancer research being conducted. In cases where there is little if any evidence-based research cancer patients and survivors often look to anecdotal evidence. I have linked an entire page of Internet results that you may learn from.
I wish that I could provide more info for you. Please note that there are antioxidant supplements that studies have shown work to enhance conventional chemo will moderating side effects. If your husband is planning to undergo a specific chemo or combination of chemotherapies, please let me know and I will research possible integrative therapies for you.
Do you have any questions?
David Emerson
ReplyHi again Dave and thank you for your prompt reply! Much appreciated! I guess Bill should not have asked his doctor how long do I have? Who REALLY knows,right? How much should he take of all or any of the supplements or enzymes you mention here? I have been using Healthforce antioxident extreme for the last few months. Is it advisable for Bill to take that also? He did for awhile, then I got nervous about it and made him stop. I will buy the NOW stuff right away, but need to know how much he should take. Do you personally feel he is at the end of the line? His doctor said his lung is currently 90% healthy. I guess if that changes a lot he can always live with one lung. Thank again,
Mindy
Hi Mindy-
You are correct. Asking “how long do I have doc?” doesn’t do anyone any good.
Without knowing Bill I can’t really talk about supplement doses. I suggest you work with a Naturopath or dietician in your area. After going through my own “terminal” experience I never think anyone is at the end of the line. But turning things around will require effort on your and Bill’s part.
Good luck
David Emerson
ReplyThank you so much! I have now subscribed to your newsletter.
Mindy
ReplyHello David- I am a 64 year old wife of a 57 year old husband Bill who has been battling GIST cancer since 2004. He had surgery at Fox Chase in Philadelphia in early 2005 to remove a very large tumor near his stomach and lost 20% of his stomach and the frontal lobe of his liver. He went on Gleevec and it worked wonderfully (with one or two small but manageable recurrences) until late last year when his doctor found another tumor growing in his pelvis (very rare place for a rare cancer like GIST to occur) and they felt Gleevec was no longer working. They tried radiation which worked for about one month and then he went on Sutent. He was on Sutent till early July when they decided it was not working and they gave him Stivarga. This drug nearly killed him, with very high fevers and a leper-like rash all over his body. Around this time it was also found that there was a 1 cm GIST tumor in his right lung. This is a lot more serious than the pelvis,although his ability to walk is now being compromised by pain from the pelvic tumor. He spent several weeks of the summer in the hospital between his lung biopsy and his adverse reaction to Stivarga. They decided he could go on a clinical trial but until then, put him back on Sutent and added Rapumune to it. As of today, the tumors have both grown and these 2 drugs will be discontinued. We are now going to start Pazopanib (although Dr Von Mehrens does not expect much from it). He cannot start the clinical trial till January. Dr. Von Mehrens feels his life expectancy is definitely NOT 10 years and possibly not even 5. I am of course, totally devastated by this news. I do not know what to do–should we contact MD Anderson, or should we go to a Mexican clinic? Thanks for any advice. He is just too young!
Sincerely,
Mindy Paquin
Hi Mindy-
I am sorry to read of your husband’s cancer diagnosis. Though I have to say that Bill has done well to manage a serious cancer for more than 10 years. Yes, you two have been through the ringer. But depending on Bill’s stage at diagnosis, he appears to be beating the averages.
As for your next therapy steps, based on your email it appears that conventional chemotherapy and radiation have run their course. I don’t believe that MD Anderson or any other conventional cancer center will be able to offer curative therapies.
Therefore you may want to consider integrative therapies. By integrative I am referring to those nutritional supplements and lifestyle therapies that may enhance your next chemo, Pazopanib, while trying to reduce the side effects. Pazopanib inhibits angiogenesis. This means it tries to stop the growth of blood vessels to the tumors.
There are several antioxidant supplements that act similarly and can act integratively with Pazopanib. These nutritional supplements include curcumin, resveritrol, green tea extract and others. I have linked a blog post about systemic enzymes (Wobenzyme N and n-acetyl carnatine) as well for you to read and consider.
At this point in Bill’s therapies I believe that pursuing nonconventional therapies may provide possibilities.
Gastrointestinal Cancer- Think Non-Conventionally
Let me know if you have any questions.
Hang in there
David Emerson
ReplyDear David:I am a 71 year old male. I have a defibrillator and sever COPD. I have just undergone three surgeries for throat cancer. They removed 42 lymph glands. Finding three with tumors. One 6 cm the other two in the 1.5 cm range. They removed my tonsils took a number of biopsies from my tongue and throat. Did not find any thing else. The pet scan does not show any more tumors. A fourth surgery had to be done to repair bleeding from the previous surgery.I have difficulty talking can not eat. Feeding myself through a feeding tube. All within 50 days. I am not recovering very well at this time. My question is what are the advantages and /or the disadvantages in my taking Chemo and Radiation? I have and am still a very sick man.This is not quality life. They assure me my speech will most probably get worse and not likely to improve afterwards. It will take somewhere from 5 to 6 months to get through it and a lot more pain than what I have already gone through. IS there any real numbers that show reason why someone would want to put themselves through it?
Thank you.
ReplyHi Owen-
I am sorry to read of your health challenges. I have to say that though you call yourself “a very sick man” I have to add that you are both a very sick man and an incredibly TOUGH man. I am not an oncologist I am a cancer survivor like you do take what I say accordingly.
To answer to your question “My question is what are the advantages and /or the disadvantages in my taking Chemo and Radiation?,” while there may be long-term benefits (maybe) to chemo and radiation, there are many more short term disadvantages.
The tone of your email indicates that you already understand the basic equation.
From a cancer standpoint, by surgically removing your cancer you have already “debulked” your cancer. You have greatly reduced the amount of cancer in your body. Chemo and radiation may kill a few more cancer cells but at the same time chemo and radiation will surely cause a great deal of collateral damage.
I encourage you to take the steps necessary to heal yourself. Moderate exercise (walking daily), nutrition (when you can eat solid foods) etc. all will make you feel better, live better. Healing is good, more pain is bad.
Finally, “is there any real numbers that show…?” I knew an accountant once that said that she could make the numbers look ANY WAY she wanted them to look. Yes, there may be numbers out there that recommend chemo and radiation. However I can make a convincing argument for NOT doing any chemo or radiation and working on healing yourself. This will result in quality and length of your life.
Let me know if you have any questions.
David Emerson
ReplyHi David,
I was diagnosed with multiple myeloma going on 5 years ago. My body is quite healthy with all I have been through up to now. | am now on Revlimid and the side effects are horrible. I try to tell this to my mm specialist but he tells me the side effects are caused by stress. I really don’t agree with him however, he wants me to go on medication for anxiety or depression or…. I just feel stuck with the whole situation. I was under the impression there was no cure for mm. I just looked up Dr B website to help a friend and saw he was treating mm.
I know he has had success treating your mm. does he have success with a lot of people who have mm? I am desperate to find a solution but am not having much success with the medication I am told I have to take.
Hi Ovila-
I am sorry to read of your MM diagnosis and therapy-related side effects. Yes, living with cancer does cause stress but I agree with you that chemotherapy, including Revlimid, causes very real collateral damage aka side effects.
Before I talk about antineoplaston therapy (ANP) through the the Burzynski Research Institute (BRI), I would like to mention those anti-oxidant supplements that research has shown to ENHANCE the efficacy of revlimid and velcade while REDUCING the toxicity.
By supplementing with omega 3 fatty acids, curcumin, resveritrol, green tea extract and vitamin D3 studies show that your chemo will work better while you feel better. And you may choose to reduce your daily or weekly dose of chemo.
Let me know if you would like to see the studies and or would like brand info and dosing information. I can tell you what I take…
Regarding ANP, yes, I was terminal in ’97 began ANP in 11/97 and over the next 17 months became MM free where I remain to this day. There are many issues that you should understand before going to the BRI to begin ANP. If you would like to learn more we should talk on the phone. Too many issues to try to email, too much Q and A.
The main issues are that your health insurance probably will not pay for ANP and the fact that there are only three MMers who have written about their experiences on the Burzynski Patient website, me being one. Though there are several other blood cancer testimonials.
We should talk is my point. Let me know if you would like more info.
thanks
David Emerson
ReplyI turned 61 right after being diagnosed, good health, so they said at the center. I have been diagnosed with invasive ductal carcinoma. The lump in left breast is quite large (size of med. egg). I’ve had 2 drained of fluid in previous years that were fibrocystic breast disease. They do not show on mammo or ultrasound. Biopsy came back positive. MRI showed clear in lymph nodes and right side. It is slow growing, estrogen fed, I’m taking Letrozole to shrink tumor, oncologist is leaning toward mastectomy anyway after it shrinks. And I am candidate for double mastectomy with or without reconstruction due to density. I do not want to take chemo due to poisoning that I keep reading and hearing about. Also, I’ve gone to a leading cancer center yet friends and family encourage me for 2nd opinion. Are you familiar with the documentaries showing last week and this on “Truth about Cancer” which is alternatives to Chemotherapy in most cases ie: diet, hbot therapy, red light sauna, micronutrients, etc. Thank you for your opinion.
ReplyHi Dianne-
I am sorry to read of your invasive ductal carcinoma diagnosis though there are several positives in your email.
1) “MRI showed clear in lymph nodes and right side.”
2) “It is slow growing, estrogen fed, I’m taking Letrozole to shrink tumor,”
3) and you are in good health.
When you say “They do not show on mammo or ultrasound.” I will assume you are referring to your breast cancer.
Regarding your questions:
1) A second opinion is always a good idea. Most health insurance plans cover the cost. You may simply confirm what the first oncologist said or you may learn of options or alternatives that you didn’t know about before.
2) “Are you familiar with the documentaries showing last week and this on “Truth about Cancer”” Yes. I am a long term cancer survivor myself who pursues diet/nutrition, sauna (had one this a.m.), I supplement and moderately exercise 6 mornings weekly. I do not consider these therapies to be replacements for surgery, chemo and radiation but complimentary or therapies to go along with conventional therapies.
Yes, chemotherapy and radiation are toxic and may cause collateral damage aka side effects. The decision you must make is about the RISK of breast cancer relapse. When you undergo a certain therapy, what are the chances that the cancer will return?
Several things for you to consider_
1) single or double mastectomy or surgical removal of your cancer greatly reduces the risk of cancer relapse.
2) according to your diagnosis your cancer has NOT spread. “Clear lymph nodes.”
3) please consider the oncotype DX test for invasive estrogen positive (you) BC- The test results will give you more information about the risk of relapse.
http://breast-cancer.oncotypedx.com/en-US/Patient-Invasive/GettingTested/AmIEligibleForTheTest.aspx
Feel free to email me with questions and please contact me again after you have the oncotype DX test and you want to talk over your next
steps.
Hang in there, good luck and let me know.
thanks
David Emerson
Survivor, Director, PeopleBeatingCancer
There are so many different natural ways to help to destroy or prevent cancer it can be over whelming.How do we know which ones are scams and which arent?I have been diagnosed with stage 3 colorectal cancer.I got a second opionion from the cancer center of america in newnan georgia.the doctors here in augusta wanted to give me a colostomy bag and start chemo right away.when i got second opinion from cca they said they could take care of it with chemo and 6 weeks radiation which i did.there was also a mass that light up on the pet scan that the surgically removed in feb along with one of my ovaries.both were benign.there was a spot on my lung that had showed up on the pet scan as well it was 5mm went i went back for scan in july it had shrunk to 3mm they are watching it.they have not taken a biopsy of that spot yet.I have since had a spot on my face that was cancerous and i had it scraped off 2 weeks ago.my question is which protocol would you recommend and what web sites could we go on for this info.I do take zeal apricot seeds with zinc so the body can absorb the vitamin b-17, baking soda vitaminc and greens on the go kambucca.I rub my feet with frankinsense oil and have thought about the cannibus oil. I pray every night that God would give us wisdom.could you please recommend a homopathic doctor near aiken south carolina?thank you in advance for your information.
ReplyHi Kim-
I am sorry to read of your colorectal cancer diagnosis though it sounds as if you are working to take control of your health. A second opinion, debulking other possible cancers, complementary therapies, and your spirituality are all forms of evidence-based therapies that will help you fight your cancer.
Several things. Yes, a diagnosis of cancer is overwhelming. It is difficult to be certain about any therapy be it FDA approved or not. Much of it depends on the personal judgement of the cancer patient. In this case this is you.
Sometimes qualified oncs. can differ on treatment options for a given cancer diagnosis. I wrote a blog recently when I read an article that talks about a situation similar to yours. Much of the treatment discussed below is up to the patient. The answer to your question “my question is which protocol would you recommend and what web sites could we go on for this info?” is my blog post below. There is two sides to the outcome for a diagnosis such as your. Some people will do anything to avoid a colostomy bag but others in the article linked below talk about how they have gotten used to one.
http://peoplebeatingcancer.org/rectal-cancer-diagnosis-read-this-to-learn-the-challenges/
As I mentioned above, all of the complementary therapies you mention above, b-17, vitamin c, kambucha, essential oil, etc. are all good. The evidence on these is controversial but I think complementary therapies to boost one’s immune system is important.
I will add info about several specific anti-oxidant supplements that have proven to by cytotoxic to colorectal cancer. If you choose to undergo chemo please note those supplements that are proven to enhance the efficacy of your chemo in the post linked below.
Colorectal cancer non-conventional therapy supplementation-
Lastly, regarding a homeopath near you, I have no personal experience with any of the referrals below.
http://www.handsonhealth-sc.org/golocal/golocal.php?nid=L55®num=0&mcity=0&county_id=2&filter=L55
My homeopathic doctor that I highly recommend is named Dr. Douglas Falkner. douglas falkner
Kim, please read over this info and reply with any questions you may have. You are at the start of a long journey and education and information is the best way for you to make the best decisions for you.
thanks and hang in there.
David Emerson
Survivor, Creator and Director PeopleBeatingCancer
Hi David,
Question:
What supplements do you recommend for Mets BC?
I am currently taking:
– Vitamin D
– Magnesium
– Multi-vitamin
– Fish Oil
– Tumeric
Thoughts?
ReplyHi Susan-
Did you reply to one of my emails asking me to provide supplement recommendations? If so I apologize.
About your question for nutritional supplementation for BC that has metastasized, there majority of research that I have found is directed at reducing the” risk of breast cancer.” There is little if any research for supplementation for metastatic BC. My belief is that anti-oxidant supplementation that reduces the risk of a FIRST BC diagnosis is cytotoxic to BC. But I have no research to support my thinking. Also, there is the idea of supplementation and lifestyle to strengthen bones. In addition to nutritional supplementation I would add bisphosphonate therapy. This prescription must come from your oncologist.
Yes, all of your current list is supported by research. Actually, the multi-vitamin is debatable but I feel strongly that a healthy immune system fights cancer. I believe in whole food vitamins not synthetic vitamins but again, this is controversial.
1) vitamin D- the issue is what serum blood levels to reach. Most studies cite a minimum of 20 nanograms/milliliter- Other studies cite 50 ng/ml to be the best level. I have to admit that if I were metastatic I would consider 50 ng/ml to be the level I would want to reach but again, I have no research to support my thinking. I have my vitamin D blood levels tested through Life Extension Foundation’s blood testing service. I have my blood drawn locally and the results are emailed to me. I can give you more info if you want.
FYI. I supplement with 2000 mg daily. My blood serum levels as of last fall was 32 ng/ml. vitamin d blood levels
2) Magnesium- I supplement with mag. because a) bone density, 2) heart health, 3) nerve health and 4) brain health. I recommend this for bone density.
3) Selenium- I have no personal experience with selenium but this research says it helps met. BC- http://www.ncbi.nlm.nih.gov/pubmed/23613334
4) Omega 3 fatty acids- I just blogged about fish oil and met. BC. Very thorough article citing much research- Plus I link to the amazon entry for the fish oil that I use. PBC is an amazon affiliate- if you purchase we get 5%- I feel strange saying this but I believe in transparency.
http://peoplebeatingcancer.org/omega-3-fatty-acids-reduces-breast-cancer-relapse/
5) curcumin/turmeric is another supplement with thorough research. Please consider supplementing with the formula that combines both curcumin and ginger.
http://peoplebeatingcancer.org/?s=curcumin+breast+cancer&submit=
6) green tea extract- http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4127621/
If my cancer had metastasized I think I would supplement aggressively. Further I believe strongly in frequent moderate exercise. If you are able I highly recommend something daily.
I do all but 3) but at maintenance doses. Please let me know if you have any questions.
thanks
David
ReplyI was clinically ( gynocology ) diagnosed with cervix cancer .
Laboratory tests , confirmed cervix and vaginal cancer ( no diagnosis ) as to which one was primary
Further tests revealed specifically CT scan and MRI …. Revealed swollen lymph nodes in two areas
One liver and one around rectum
Colonoscopy … Find one polyp . ( no lab results ) clinical look … No cancer
Present team at Princess Margaret in Toronto … Speared headed by radiologist ( wanting / intending to treat radiate lymph node as cancer , w/ diagnosis
1. Iam undergoing a Ct pet scan and my question is what other tests if any should I undertake to diagnose this nymph node issue …. And should I not and why can I note obtain a concise and clear diagnosis
Can you assist me and how …
Maria
Sent from my iPad
ReplyHi Maria-
I am sorry to read of your cervical cancer. I will address your question below but before I do I want to offer information, research, etc. with respect to possible therapies, possible side effects from those therapies and ways to minimize those side effects (aka collateral damage from chemo and or radiation).
In other words, I have learned from my experience as a long term cancer survivor that knowledge is power- the more you know, the better decisions you will make, the better you will feel.
Your question ” my question is what other tests if any should I undertake to diagnose this nymph node issue …. And should I not and why can I note obtain a concise and clear diagnosis?.”
Your goal is to determine if your cancer has metastasized or spread. This is what your onc. is trying to confirm. A CT. PET scan should determine this. Good news that you do not have colon cancer.
If you are interested in more info, let me know what your onc. says about your CT/PET scan, possible therapy, surgery, chemo, radiation possibly. Based on your feedback I can provide research for you to consider your options.
Hang in there.
David Emerson
Survivor, Director PeopleBeatingCancer
I am a 62 year old female who was diagnosised with breast cancer 15 years ago. I had a lumpectomy with chemotherapy and then radiation. about a year ago I was diagnosised with stage 4 breast cancer that has mets to bone liver and maybe lungs. I changed my diet and have been taking sacred franchinsence drinking esiac tea jasmine ands enchanted tea . I also take fresh ginger mixed with fresh turmeric and then mix them with honey. I eat it teaspoon 4 times per day. take about 5000 mg vt. C. Avoid sugar and eat primarily meats with no hormones or antibiotics . Drink a plant based protein shake every morning and add vt. D cells forte max 3 . I do see onogoligist monthly for an injection that is suppose to keep cancer in the bone from spreading and I take a daily pill to suprpress estrogen as my cancer is estrogen fed. My cancer counts have been going up the past few months. Do you have any suggestions to help me ? MD is not giving me any hope and does not know I am doing alternative therapy. I have thought about trying B17 or maybe peach extract.
ReplyHi Kathy-
My apologies for taking so long to reply. You are doing so much that is right,(by my way of thinking), that it took me a couple of days to think about offering ideas or therapies that may be useful to you. First and foremost, please try not to think about your dr. not giving you any hope. My onc. told me I was terminal back in 1997. Conventional oncology is limited in it’s thinking.
For the sake of my input below I will state my assumptions. The injection you refer to is a bisphosphonate or bone hardening therapy. You are supplementing with vitamin C, curcumin and vitamin D3. Your diet is good. You are suppressing your estrogen production.
I would continue all these therapies. I will list therapies below with links to the evidence-based research. I have found a number of studies that cite nutritional supplements acting synergistically with each other. By taking curcumin, resveritrol, omega 3 fatty acids together their apoptotic effect may be enhanced.
Please consider supplementing with resveritrol. I’ve been taking resveritrol (I can email my brand dose if you would like) for more than five years now.
Please consider supplementing with omega 3 fatty acids- Again, I can email the brand I take.
Please consider supplementing with green tea extract-
Please consider supplementing with milk thistle-
The last therapy is both well studied as a breast cancer therapy yet is not really pushed by BC oncologists. I am linking a study below authored by Dr. Dean Ornish. Dr. Ornish studied prostate cancer patients but I believe that the ability to change gene expression holds for breast cancer patients as well as prostate cancer patients.
Dr. Ornish advocates DAILY, moderate exercise. I work out six days a week but moderately. I spend 30 mins. on an elliptical every other day and I lift weights moderately. The weights are so light that you may think they are TOO light. Do multiple reputations until you get tired.
Here is the study by Dean Ornish-
Lastly, regarding the last sentence about B17 aka apricot seeds, while I don’t know much about this therapy other than what we all have read, I am happy to research this therapy if you ask me to.
Let me know if you have any questions.
Hang in there.
David Emerson
ReplyDavid I have prostate cancer and my scores were 8-9 very aggressive. My scans show that it has not spread yet. My Urologist said I must have my prostate removed because I am only 50. My friend knows Laurens Pierce who used Tomo Therapy and has been cancer free for nine years without all the side effects. If this works why would they want to remove my prostate? What do you think?
ReplyHi Bill-
I am sorry to read of your prostate cancer diagnosis. I will assume that by “scores were 8-9” you are referring to your Gleason score. The fact that your PCa has not spread aka metastasized is good. Have you been given a stage of your cancer? A stage will help you make a decision as well.
With aggressive therapy there is always the risk of side effects. The question is whether or not a radical prostatectomy (complete prostate removal) will result in greater collateral damage than tomotherapy.
Tomography is relatively new as a prostate therapy. Therefore you and I have limited studies on which to base our decisions. I have linked and excerpted a Pubmed study below that I think applies to your situation. I will list issues that you must deal with if you choose to proceed with tomotherapy. I have read many studies citing the collateral damage of a radical prostatectomy and you are correct in your thinking- surgical prostate removal can cause a great deal of collateral damage.
1) It is clear from my research that the specific tomotherapy device is important in your therapy.
2) Further, it is important to find the radiation oncologist with as much tomotherapy experience as possible.
3) lastly, it is important to confirm with your health insurer that they will pay for tomotherapy at whatever facility you go to if you choose tomotherapy.
Keep in mind that if your Urologist’s hospital (where he works) does not offer tomography then they won’t offer it to you as a therapy.
I can research tomotherapy locations for you if you are interested.
Lastly and most importantly there are several nutritional supplements such as vitamin e (broad spectrum) and resveritrol that have been shown to reduce radiation damage. Again, if you are interested I can provide studies and specific brands that have been evaluated and approved. Let me knw.
“Based on radiobiology evidence, hypofractionated radiotherapy has the potential of improving treatment outcome in prostate cancer patients. In this study, we evaluated the safety, in terms of acutetoxicity, of using moderate hypofractionated radiotherapy delivered with Helical Tomotherapy (HT) to treat prostate cancer patients…
Acute toxicity was acceptable, independently from the system used to score side effects. Moderate genitourinary toxicity was more frequent than gastrointestinal toxicity. No correlation between acute side effects and patients’ characteristics or physical dose parameters was registered. EPIC evaluation showed a negligible difference in urinary and bowel function post-treatment, that did not reach statistical significance…
Our experience confirms the safety of moderate hypofractionation delivered with HT in prostate cancer patients with low, intermediate and high risk.”
Bill- my research into tomography has been interesting. Thank you.
David Emerson
ReplyHi David:
I just came across your site, and it is excellent!
David, I am an otherwise fit middle aged man, 56 years old, who was originally diagnosed with Mgus four years ago, on a routine blood test, here in Canada, that showed an abnormally high level of protein in my blood (IGM levels).
My IGM level at the time was 10 g/L, and had stayed around that level for two years.
However, in late 2013, the IGM m spike level started increasing even more, and in subsequent blood tests the last couple of years, the levels started rising to 12.30 g/L, to 15.40 g/L, to 19.10 g/L, and now at 21.70 g/L.
The IGM levels are supposed to be between 0.46-3.04 g/L!
The Oncologist now said that short of doing a biopsy, she firmly believes that I have lymphoplasmacytic lymphoma, or Waldenstroms, and no longer, unfortunately have Mgus.
I went to another Oncologist here in Canada, and she too, confirmed that I have smouldering Waldenstroms.
While all the other blood tests over the last few years of testing have always been normal, with normal readings of the white blood cells, red blood cells, platelets, etc, I also have never had any symptoms at all, and have always been asymptomatic.
I take care of myself, eat organic foods, and have always been interested in the field of alternative health (vitamins, herbs, etc).
Lately I have tried sauna treatments, coffee enemas, and experimented with vegetarian diets, paleo, raw, macrobiotic diets, until recently just having a varied diet of everything.
My concerns are that, although I am not experiencing any symptoms, I am at wits end as to why the IGM levels have steadily climbed over the last two years, and that, not one, but two Oncologists believe that I have smouldering Waldenstroms, or lymphoplasmacytic lymphoma.
David, it is very frustrating for me, and upsetting, to know, that now with this ticking time bomb of an illness, it seems that it is only a matter of time before one experiences symptoms according to these Oncologists.
Yet I feel fine, enjoy working out, however, am depressed to hear that I have the dreaded ‘C’ according to these doctors.
I have also heard from them, that if one is not experiencing symptoms, and even if a biopsy shows that I have this disease, since I have no symptoms, there is no treatment.
Interestingly enough, a friend of mine had Waldenstroms, and although recently he died unfortunately, he would always tell me that the Oncologists should only treat ones symptoms, and not a number (IGM reading) on a blood test, no matter how abnormal that reading might be.
David, although friends may say to just ‘live your life’, yet receiving news that one has Cancer, is not easy at all.
Due to my anxiety levels, and although I am not experiencing any symptoms at present, what are your views on mindfulness meditation?
David, again, I feel good, and am curious to also ask you your opinion on other supplements, other then the Vitamin D, Curcumin, Resveratrol, Co-Q10, grape seed extract, NAC, and a few others you have suggested on your website, would you recommend any other supplements with someone allegedly who has this condition?
Further, you mentioned that you do a sauna once a week, (I have also used a sauna, however used it every day) and am wondering if you think I should continue the sauna sessions, or stay away from it?
In closing, I would like to know, what I can do, if anything, to prevent the IGM levels from continuing to rise?
I mean I would like the levels to say at a stable reading, and to stay around that level, and not having to continue to rise or ascend to the present high level it today.
Any words of advice, would be appreciated,
Thanks David,
Regards,
Lawrence
Hi Lawrence-
Thank you for your kind words. I am sorry to read that you are so frustrated with your health. I will excerpt your email below in an effort to provide experience and research that may help your situation.
1) “I went to another Oncologist here in Canada, and she too, confirmed that I have smouldering Waldenstroms.” A second opinion is always a good idea. Coming out of any pre-cancer is difficult but you lead a healthy lifestyle and you appear to be open to learning about additional lifestyle therapies that may reduce your pre-cancer indicators.
2) “David, it is very frustrating for me, and upsetting, to know, that now with this ticking time bomb of an illness, it seems that it is only a matter of time before one experiences symptoms according to these Oncologists.” Yes, being diagnosed with cancer is extremely difficult. However I look at your situation differently than you do. You appear to be willing to eat, sauna, moderately exercise, supplement, etc. which I would argue is the best series of non-conventional therapies for your situation currently. You may prevent your blood cancer from further advance to WM.
3) “although friends may say to just ‘live your life’, yet receiving news that one has Cancer, is not easy at all.” I agree that living with a cancer diagnosis is difficult. My solution (just mine) is to focus on non-conventional therapies. This focus helps me think that I can control my cancer. I say “think” I can control because I don’t really know if I control it.
4) “I have also heard from them, that if one is not experiencing symptoms, and even if a biopsy shows that I have this disease, since I have no symptoms, there is no treatment.” Oncologists are saying only that Conventional oncology cannot offer any therapies. Frankly, this is a good thing right now. Your non-conventional therapies can be more effective.
5) “Due to my anxiety levels, and although I am not experiencing any symptoms at present, what are your views on mindfulness meditation?” I do not practice mindful meditation though I believe strongly in the mind-body connection in cancer care. Yes, learn this therapy and practice it.
6) “David, again, I feel good, and am curious to also ask you your opinion on other supplements, other then the Vitamin D, Curcumin, Resveratrol, Co-Q10, grape seed extract, NAC, and a few others you have suggested on your website, would you recommend any other supplements with someone allegedly who has this condition?”
While all those supplements are supported by research as therapies to slow or kill MM, I can’t find much research about nutriceuticals and WM. The only study for your situation is linked below-
My guess is that there is little research going on since WM is relatively rare blood cancer. I cannot say with any surety if those supplements will benefit you.
7) “Further, you mentioned that you do a sauna once a week, (I have also used a sauna, however used it every day) and am wondering if you think I should continue the sauna sessions, or stay away from it?”
My reason for sauna is that 1) studies show that whole body hyperthermia kills cancer, 2) sauna improves endothelial function ( I have heart issues…) and 3) sauna detoxifies you (causes heavy metals to be excreted). Not to mention my sauna relaxes me.
I think everyone should sauna. Yes, check with your doctor and drink plenty of clean water before but sauna’s are excellent therapy.
7) “In closing, I would like to know, what I can do, if anything, to prevent the IGM levels from continuing to rise?” I think that if you continue your nutrition, exercise, mind-body therapy, read and perhaps add resveritrol and simvastin, sauna, etc. then yes, I think your IGM levels could stabilize.
I hope I have addressed your main concerns. Let me know if you have any questions.
David Emerson
ReplyHi David:
Thank you so much for the quick reply.
David, a couple of more questions if that is okay.
David, I was thinking, that if I did end up having a biopsy done in the near future, to appease perhaps these Oncologists perspectives, and maybe confirm their evaluation observations that I do indeed have smouldering WM, to a more formal diagnosis, I have also heard that having a biopsy could also stir something up, in the body, and if one is not experiencing symptoms at present, is it really necessary then to have one at all at present?
The Oncologist did say to me to consider having an ultrasound of my spleen, since an enlarged spleen is a sign that it could be WM, however, an ultrasound of the spleen was done in the past, and it was fine.
I will though get another ultrasound to check it again.
David, in terms of your answers, one thing I forgot to mention to you with regards to the sauna, was that I had purchased a ‘near infrared sauna’, from ‘Sauna Space’ (www.saunaspace.com) not a far infrared sauna.
The owner of the company is a wonderful man, and appreciated all his support on the phone when placing the order a year ago.
It is not a far infrared sauna, rather it is a low emf near infrared sauna.
I have used it, and enjoyed it, however, unfortunately as mentioned, since my IGM levels went up yet again on the most recent blood test result the other day, this is one of the reasons why I have been questioning everything lately to see why the IGM levels have gone up so much this past year and a half.
One friend of mine, suggested taking very hot baths, as opposed to saunas, as a way of helping the lymphatic system, and body, (hyperthermia) fight the cancer.
The other ‘new’ alternative therapies that I have looked into recently, were also the consumption of raw milk, from a local farmer, however, I will stop that, since I have heard that perhaps a little dairy is okay, yet every day, some studies have shown not to consume dairy at all, if one has ‘C’.
So, the consumption of raw dairy, may or may not have also be a contributing factor as to why the IGM levels have gone up?
Further, according to the former Dr. Kelly, and his metabolic diet protocol, they had recommended coffee enemas, which I have also tried these last few months, however, it is hard to say if they too may or may not have contributed to the ascension of my IGM levels.
So, in your opinion, do you think I should continue the near infrared sauna treatments, and coffee enemas, and or, perhaps give them a rest for the time being, or use them from time to time, and, or don’t use them at all until the next scheduled blood test results in December, to see if the IGM levels have stabilized let alone continue to go up?
Further, an information piece for yourself, and your readers, is that have you heard of the Buteyko method? This method of breathing was invented from a former Russian scientist. It is a very interesting discussion of looking at our breathing, and the fact that one should breathe through their nose, and not through there mouths.
David, if you want more information about this, google, the name ‘Buteyko’ breathing on the Internet, and let me know your views on this, if you wish?
David, it is a form of breathing, or reduced breathing by holding your breadth, as a way of improving the oxygen in your body. I tried it in the past, and had gotten away from it, due to my busy schedule, however, will now give it a shot again, and will try the breathing exercises as a way of calming down my body, and mind, as well as improving one’s oxygen levels.
Wouldn’t it be nice if that contributes to the stabilizing of the IGM levels?!
David, with reference to your answer about my inquiry about additional supplementation in point #6) you had mentioned with regards to the supplement question to you, that from one study with Waldenstroms, it had stated the use of the drug ‘simvastitin’, to try and bring down the IGM levels.
Yet I am not taking any drugs, and am nervous about drugs, and have only taken alternative forms (vitamins, herbs, homeopathic remedies) and although I hugely appreciate your findings into nutrition supplements for me, and for people with WM, as opposed to MM, should I ask my Doctor about the simvastitin, or try and find the ingredients of that drug, and see if there is a reasonable equivalent of a supplement to be used, or a homeopathic remedy?
Further, some alternative doctors in the United States, have recommend mega doses of Pancreatin supplements, for people with Cancer, yet for blood cancer, this is a difficult one to try to figure out.
David, thank you again so much for your help, support, and assistance in this area, as I am so pleased that I came across your site, and ‘met you’ through your responses to my inquiries, however, the one thing that keeps bothering me David, is trying to figure out why my IGM levels have continued to rise (and although I am not experiencing any symptoms) am so torn inside, as to why this keeps happening to me?
I understand the importance of being positive, and appreciate your support in my quest to looking into the alternative ways of doing things, such as supplements, breathing, sauna, perhaps coffee enemas, etc, yet am still puzzled that my levels keep rising.
Hopefully by the next tests in December, I can hear from the Oncologist(s) that the level did not go up next time. Wouldn’t that be nice?!
Thanks David,
Looking forward to your response when you have a moment,
Take care,
Lawrence
Hi Lawrence-
Again, I will excerpt your questions in order to address as many of your questions as possible.
1) “David, I was thinking, that if I did end up having a biopsy done in the near future, to appease perhaps these Oncologists perspectives, and maybe confirm their evaluation observations that I do indeed have smouldering WM, to a more formal diagnosis..”
Assuming that a diagnostic test is covered by your insurance and has no side effects I think that the more info you have to make decisions the better.
2) “I have also heard that having a biopsy could also stir something up, in the body, and if one is not experiencing symptoms at present, is it really necessary then to have one at all at present?”
I have read about the general concern that biopsy’s can “stir something up” but I have never found studies to verify this. I don’t know enough about your possible cancer but are there other diagnostic tests (blood or urine) to give the same info?
3) “David, in terms of your answers, one thing I forgot to mention to you with regards to the sauna, was that I had purchased a ‘near infrared sauna’, from ‘Sauna Space’ (www.saunaspace.com) not a far infrared sauna.”
Yes, many people are concerned about EMF’s- again, I have found no studies to confirm anything. I,myself take an old-fashioned low tech approach by using a sauna with electrical heated rocks. I cannot offer any info, either way, about near or far.
4) “One friend of mine, suggested taking very hot baths, as opposed to saunas, as a way of helping the lymphatic system, and body, (hyperthermia) fight the cancer.”
I think whole-body hyperthermia is an excellent therapy for people with blood cancers (systemic cancer)
5) “So, the consumption of raw dairy, may or may not have also be a contributing factor as to why the IGM levels have gone up?”
After reading both pluses and minuses about raw dairy (and red meat too) and cancers, my feeling is that each person metabolizes these differently and as such, may need them (dairy/red meat) or not. The book “Eat right for your blood type” makes this case.
6) “So, in your opinion, do you think I should continue the near infrared sauna treatments, and coffee enemas, and or, perhaps give them a rest for the time being, or use them from time to time, and, or don’t use them at all until the next scheduled blood test results in December, to see if the IGM levels have stabilized let alone continue to go up?”
I think detoxification and whole body hyperthermia are both therapies that fit a healthy lifestyle- including nutrition, frequent, moderate exercise, hydration, mind-body therapies, sleep, etc.
7) “Further, an information piece for yourself, and your readers, is that have you heard of the Buteyko method? This method of breathing was invented from a former Russian scientist. It is a very interesting discussion of looking at our breathing, and the fact that one should breathe through their nose, and not through there mouths.”
I don’t know of the Buteyko method however deep breathing is also a good general therapy- when I find myself getting tense in say, traffic, I breath deeply in order to relax myself. I will learn more about this therapy. I have an oxygen concentrator and give myself 100% oxygen from time to time. I consider increased oxygen to be similar to sweating and detoxifying.
8) “…should I ask my Doctor about the simvastitin, or try and find the ingredients of that drug, and see if there is a reasonable equivalent of a supplement to be used, or a homeopathic remedy?”
Yes, I think that talking to your doctor about simvastintin would be a good idea. Resveritrol as well though this is a nutritional supplement.
9) ” Further, some alternative doctors in the United States, have recommend mega doses of Pancreatin supplements, for people with Cancer, yet for blood cancer, this is a difficult one to try to figure out.”
As I mentioned earlier I am a product of what I research and read. I have read specific studies that cite a combination of enzymes that included pancreatin called Wobenzym N to reduce both multiple myeloma and blood clots (DVT). I take Wobenzym N. I don’t mega dose, I follow what directed on the label. Yes I think Wobenzym N is an excellent therapy for blood cancers.
Wobenzyme N
10) “David, thank you again so much for your help, support, and assistance in this area, as I am so pleased that I came across your site, and ‘met you’ through your responses to my inquiries, however, the one thing that keeps bothering me David, is trying to figure out why my IGM levels have continued to rise (and although I am not experiencing any symptoms) am so torn inside, as to why this keeps happening to me?”
I can see how and why you would be torn inside, as you say. I can only offer my own thinking. I have an incurable cancer and I study to learn as much as I can about non-conventional therapies to manage my cancer.
Please keep me posted about your testing, any symptoms, etc. keep in touch. Thanks
David Emerson
ReplyHello, I am Esther Squires. My father has been diagnosed with prostate cancer matastasized to liver.
Here is a brief synopsis of what he has undergone to date. His cancer is the typical adenocarcinoma with very aggressive NEPC. He has taken radiation mostly to help with colon discomfort due to enlargement of prostate. He has undergone 3 rounds of Chemo. They have stopped his chemo because after his CT scan it has shown that it was not effective. He has 1 tumor that was at 10 cm but shrunk to 9.7. He has 2 others that were 1 cm but grew to 3 cm. during the chemo treatments. Those must be the aggressive cancer tumors. He had been on CBD oil and THC but found the high just too much for him. He eats well. There is nothing left for them to do. I would love to find some clinical trials that might fit his diagnosis. Any help would be incredibly appreciated.He is 77 years old. We live in Newfoundland, Cananda.
Hi Esther-
I am sorry to learn of your dad’s prostate cancer situation. I will try to offer therapies but I don’t understand the Canadian medical system and therefore I don’t know what is available, paid for, etc.
Regarding radiation and your dad’s colon discomfort and radiation. If you can find a clinic or hospital that offer hyperbaric oxygen therapy please read the study linked below and consider HBOT to help your dad with his pain. Please scroll down the page to read about HBOT and radiation.
Secondly, regarding your dad’s cancer metastasizing. Please consider bisphosphonate therapy BEFORE your dad’s cancer metastasizes to his bones. The study linked talks about breast cancer but your dad may find himself in the same situation soon.
As for therapy to slow your dad’s PCa cancer, if your doctor’s say that both chemo and radiation are not working and if they have not offered other therapies such as a prostatectomy (complete prostate removal) then I am not sure what I can offer.
RE clinical trials, are you saying that you want to enter into clinical trials in the U.S.? I am happy to research possible clinical trials if you are interested though I don’t know anything about Canadian clinical trials.
I will I could offer more assistance. Let me know if you have any questions.
David Emerson
ReplyHello David: I was diagnosed with breast cancer in May of this year(2015). I underwent a lumpectomy on May 26th. My first visit with the oncologist was on July 29th. At that point in time he recommended chemo…radiation and hormone therapy. Prior to this visit I had been told that the surgery was successful and that I only had to take radiation…every day for 5 weeks and hormone therapy for 5 to 10 years. I refused the chemo at which point the oncologist said he would send the pathology away to determine risk factors of my cancer returning. I have my results and the risk is low..(20) I am as healthy 61 year old woman and I do not want to do any of the other treatments because I think I will be OK. I have never taken very many drugs, only a ton of vitamins!!! My question is, after all that info…Where do I begin to find the information that I would need to battle my cancer naturally?
Thank-you
Gabrielle
Hi Gabrielle-
I am sorry to read of your breast cancer diagnosis though I am happy that you are reaching out to me to confirm your thinking. I have been working with a husband and wife team recently who have been working through what I believe is a very similar situation.
I will list my assumptions below-
1) “hormone therapy” aromatase inhibitors or tamoxifen-
2) “determining the risk factors of my cancer returning” is the Oncotype DX breast cancer test. A result of 20 indicates that the risk of relapse is low.
To answer your question “Where do I begin to find the information that I would need to battle my cancer naturally?” I will link a blog post I wrote awhile back that lists 14 different natural therapies each to reduce the risk of BC relapse. I’m sure that you know of many such as vitamin D3 or curcumin supplementation. Regular, moderate exercise is probably the most effective therapy to reduce the risk of BC relapse though conventional oncology rarely promotes it.
My point is that the therapies listed in the link below work. And you are choosing wisely to pursue the steps listed in your post to me in addition to the steps listed in the link below.
Slash Your Breast Cancer Risk of Relapse Now!
I can recommend specific brands and doses if you are interested- I can relay what I brand/dose of vitamin D3 and curcumin, etc. I take.
I hope I have answered your question. Let me know if you have any other questions.
thanks
David Emerson
ReplyHi David: I am not adverse to the radiation….probably because I don’t know a whole lot about the process. If you have any further information please share. The thing that I absolutely do not want to do is take that drug(forgot the name but it is an estrogen blocker)for 5 to 10 years. I can visualize myself coming apart within this western medical system. I know the doctors mean well but I am listening to my body screaming NO DO NOT DO IT!! Again I am rather chatty so the question is How hurtful to my system is the Radiation? Thanks David
ReplyHi Gabrielle-
Arimidex/Tamoxifen (estrogen blockers) and local radiation to your breast all have toxicities and therefore cause collateral damage. The key to your decision is that your Oncotype DX BC score means that you have less chance of relapse. I cannot say with any specificity “how hurtful to my system is the radiation” because everyone reacts differently.
If you are interested I can recommend nutritional supplementation that studies have shown reduce collateral damage and melatonin skin cream that again, research has shown reduces damage to your skin. I’m not sure my own radiation burns are fully healed after 17 years…
If you choose to reduce estrogen naturally please talk to a naturopathic doctor.
Let me know if you are interested in any of the info above or have any questions.
Hang in there
David Emerson
ReplyGood morning David; Please send me a list of the supplements that you recommend for my treatment and also more info on how to care for my skin before, during or after my radiation treatments.
Hanging in there but wobbly;
Gabrielle
Hi Gabrielle–
In addition to talking about supplements that may protect you from toxicity I want to send you excerpts/links from studies about supplements and radiation so that you can think through what supplements you take. I am not a dr. and I am not comfortable telling cancer patients what to do.
These supplements are linked to the brands that I take but you can buy anything you prefer at Amazon or your local health food store.
Let me know if you have any questions. You are shaky but you will do better (statistically) by learning, taking control of your health, taking charge…
David
1) Melatonin skin cream-
2) vitamin E- full spectrum of tocotrenols, tocopherols-
3) Resveritrol-
4) Curcumin-
Resveratrol reduces radiation-induced chromosome aberration frequencies in mouse bone marrow cells.
Radioprotection and radiosensitization by curcumin.
The excerpt below is from a book by Ralph Moss. I recommend buying his ebook on breast cancer.
“Protection From Radiation Damage
Are there specific foodstuffs or nutrients that can protect against the harmful effects of
chemotherapy and radiation? There is growing evidence that this is so, as you can see
from the following examples of research on specific antioxidants.
Vitamin E studies
• A 2012 study of 132,000+ individuals in China showed that a high level of
consumption of vitamin E either from diet or vitamin supplements lowered the
risk of liver cancer. It was published in the Journal of the National Cancer
Institute. The study was conducted by investigators from the Shanghai Cancer
Institute, Vanderbilt-Ingram Cancer Center and the National Cancer Institute.
“We found a clear, inverse dose-response relation between vitamin E intake and
liver cancer risk,” the authors wrote.
• A 2010 study showed that vitamin E-like tocotrienols “inhibited the growth” of
breast cancer cells by their effect on the body’s cytokines. “Hence, we report that
tocotrienols have potent antiangiogenic and antitumor effects….”
(Selvaduray KR, Radhakrishnan AK, Kutty MK, Nesaretnam K. Palm tocotrienols inhibit proliferation of
murine mammary cancer cells and induce expression of interleukin-24 mRNA. J. Interferon Cytokine Res.
2010;30:909-916)
• A 2009 study from England demonstrated a way of delivering a vitamin E-like
compound (tocotrienol) that seems to have profound anticancer activity in animals…”
I am looking for opinions on proton therapy for prostate cancer. I am in the very early stages of the disease and was thinking about surgery. I have been told that if you start with radiation therapy and the cancer comes back, you can not have surgery. Is there enough data on proton therapy to raise its “cure” levels above traditional radiation?
ReplyHi Frank-
By “very early stages of the disease” I take you to mean that your diagnosis was either stage 1 or 2.
If this is the case please undergo any active therapy only after you fully understand the probable side effects. Radiation, any kind, and or surgery will undoubtedly cause collateral damage aka side effects.
There are several therapies to undergo if the prostate cancer has not grown OUTSIDE the prostate with few if any side effects. I will link studies below.
Prostate
Cancer-“Normal Erection After Prostatectomy Is ‘Rare’”
Vitamin D may keep low-grade prostate cancer from becoming aggressive
Early stage Prostate Cancer? Know how aggressive your PCa is with Oncotype DX
New York Times article followed by pubmed study below-
Despite Doubts, Cancer Therapy Draws Patients
Frank- I understand that I included lots of info aka articles/studies. But the decision you are making is worth taking the time to understand more of your options. Please reply if you have any questions or if you would like more info about integrative therapies such as vitamin D, curcumin, green tea extract, etc.
thanks
David
ReplyMy husband has lymphoma. Was diagnosed in 2012, had 6 chemo treatments, was supposedly cancer free, but has now been diagnosed with it in the soft tissue in lung, etc. What herbs or vitamins can he take? This second round of chemo is really rough on him. The first time he did fine, but not this time. Please help, any suggestions appreciated. I have also seen and heard that apricot seeds can cure cancer. Do you have any knowledge, thoughts or evidence on this? Thank you, and God bless you.
ReplyHi Joy-
I am sorry to read of your husband’s relapse of lymphoma. The key for his treatment will be to learn about and consider “integrative” therapy. Taking and integrative approach to your husband’s therapy means to pair antioxidant supplementation with whatever chemotherapy he is taking.
An example would be curcumin and resveritrol supplementation with velcade or revlimid. I don’t know if this is one of your husband’s chemo, I’m simply giving an example. I would find and email you specific supplements supported by specific studies.
What chemotherapy is your husband taking or will take?
thanks and hang in there
David Emerson
Reply[…] You owe it to yourself to get a second opinion. […]
ReplyHi david, i am veteran my name is Jonathan mico diaz, and I live in san antonio tx, being 40 years old, my first language is spanish but I will do my best to tell you in shorts words what is happened to me. I was bleading while having bowel movement for several month, then I got a clonoscopy, when they found a tumor at list 40cm, after that, they sent to lab a 1.5 cm and it was possitive as a malign cancer but not stage or level have been secured yet because they are not sure. Right after that the Doctor change my nutrition and I start to juice vegetable and somebody talked to me about a product that is called transfer factor pluss, I start use this for few days before a cam scann. then my numbers came significant better, no was activity of spread cancer, but the doctor going to do a left hemicolectmy to remove the area that is damaged and reconneted the leftover to rectum. I was asking why They do not have a stage level cancer but he told me that it seems like an early stage cancer and it was necesary this surgery to see using little cuts and camera how severe can be. Since I change my nutrition my bleeding stop, today somebody was talking about flor essence and barley green, there is to much opinions so you are a survivor, and I respect what you have to tell, what can I do to prevent spreads cancer, my surgery will be on august 7 2015 but the doctor told me that if want I can delay it for about 45 days. God bless you more.
ReplyHi Jonathan-
I would like to clarify some of your email before I offer suggestions.
When you say “it was positive as a malign cancer but not stage or level have been secured yet because they are not sure.” You are saying that
1) you have been diagnosed with colon cancer but you don’t know what stage?
When you say “then my numbers came significant better, no was activity of spread cancer,”
1) you are saying that your colon cancer has not spread beyond your colon? If not, this is good for your prognosis.
When you say “I was asking why They do not have a stage level cancer but he told me that it seems like an early stage cancer and it was necesary this surgery to see using little cuts and camera how severe can be”
1) you are saying that you were not given a stage because your surgeon wanted to do “Laparoscopic” surgery to determine if your cancer had spread outside your colon?
So your question is “what can I do to prevent spreads cancer?” Your laprascopic surgery is on August 7th? I will assume the above and that your colon cancer has not spread beyond you colon. Also, I will assume that since you are a veteran that you can accomplish what I suggest. What I am trying to say is that if you had the discipline to become a veteran the you will have the discipline to accomplish the below.
1) Moderate exercise six days a week. Find some form of physical movement that you enjoy. Walking, swimming, golf, tennis, etc. but get your heart going six days a week. Start today. Go for a long walk daily to get in shape for your surgery on 8/7/15.
2) Your diet- your doctor will give you specific instructions for you you can and can’t eat after your surgery but once you heal, build lots of fruits, veggies, and whole grains into your daily diet.
3) Read the article that is linked below. I take each of the five supplements that help prevent a cancer recurrence and my cancer has NEVER recurred. I can suggest specific brands if you need me to.
These three things are the most effective therapies to reduce your risk of relapse.
5 Supplements That Help Prevent Cancer Recurrence
Good luck and let me know if you have any questions.
thanks
David Emerson
ReplyMr David Emerson thanks a lot for your time answering these questions. I will put on march your advise and I will feedback to you. Is there is something that I can do to support your dedication to this work that you are doing, let me know what to do, I respectfully wish to you a prosper and healthy life, God bless America and people like you! sincerely. Jonathan Mico
ReplyHi Jonathan-
Yes, there are two things that you can do. First, please follow my advice and remain cancer-free- and yes, please give me your feedback. Second, In May 2016 I hand-cycle in the Cleveland Marathon. I will email all the cancer coaching contacts to ask them to support me and PeopleBeatingCancer. If you feel like it, a donation will support future cancer patients.
To see me hand cycling please click this 6 second video- IMG_0694.MOV
Good luck and stay healthy.
David Emerson
ReplyAloha David,
My mother has been diagnosed as of last Monday with small cell lung cancer / extensive stage – mass rt lung, upper abdomen, lump under jaw, lump at collar bone. As of Friday MRI, it has not spread to brain. Note she is going to be 81 soon but does not look it. She is still climbing trees, looks very healthy, eats well, weighs 117 (in this case her small frame sounds like a detriment for what’s about to happen). I am not seeing any comments on this site regarding the type of cancer my mother has. I understand this is very aggressive and chemo was suggested not as a curative but palliative care. She is scheduled for her 1st chemo treatment tomorrow in attempt to stop or slow the spread for now and perhaps shrink it to buy her more time. If the 1st round is successful in achieving that, I have read how MDR cells will kick in to overdrive and other chemo treatment will have no effect.
SO educate me on boosting her immune system instead of destroying it and having better quality of her remaining life. I am seeing terms of – immunotherapy, integrative therapies, Protocel. As time is of the essence, there is not a lot of time to do thorough research of everything I am seeing on internet. Point me in in a direction if there is a direction to point me in.
God Bless you and your family for caring and sharing with complete strangers.
I appreciate your honesty and your time. jess
Hi Jess-
I am sorry to learn of your mother’s NSCLC diagnosis. I agree with your placing a priority on quality of life rather than quantity of life for a late stage NSCLC patient. I have worked with a number of late stage nsclc patients- several of whom where friends or family. My personal experience of aggressive late stage therapies such as chemo and radiation were…the results were less than the caregivers hoped.
The challenge you and your mom will face are two. First of all, alternative therapies such as protocol are relatively slow acting. Secondly when considering non FDA approved therapies there is the lack of credible information.
Do you and your mom have any interest in learning about and considering “integrative” therapies? The blog post linked below talks about nutritional supplements such as curcumin, resveritrol, grape seed extract and omega 3 fatty acids that ENHANCE conventional chemo while reducing toxicity.
In my experience, taking an integrative approach may get you and your mom the best combination of both quality and quantity of life. Please read the post and studies linked below and let me know what you think or if you have any questions.
The case for integrative therapy in stage 4 adenocarcinoma lung cancer
Hang in there,
David Emerson
ReplyRe: David Emerson’s wife
I too have stage 4 colon cancer – diagnosed in 2012 and given a two year prognosis. I understand your wife’s position and have gone through the conventional treatments…surgery (colon resection, liver resection twice and hysterectomy), chemo (folfuri, folfox, currently panitumumab). My original onc told me “absolutely not, you should not do anything but conventional treatment” That made me angry because I felt there had to be something more that I could do. I decided to research and pursued alternative therapies to use alongside the chemo. I met with a Naturopath who has trained in the treatment of cancer and we determined what would be best for me in terms of my cancer. I have been using the following since July of 2014: curcumin, vitamin C infusions, Cytocalm, B12, B6, and Melaton 5. I also changed my diet by cutting out red meat, processed foods and sugar. Recently I began mistletoe therapy. My current onc keeps telling me how wonderful I look and when I finally asked him how exactly I should be looking given the extent of my cancer, he said typical patients at my stage are jaundiced and their eyes are usually yellowish. Unfortunately he is not familiar with naturopathic treatments and believes it’s the panitumumab, which, by the way, is not working and my tumours continue to grow.
I don’t believe there will ever be a cure for cancer. I do however believe that you can alter your life to make the diagnosis/prognosis a better one. My thoughts and prayers are with you and your wife as you travel though your cancer journey. Stay strong and positive even when the going gets tough!!
Hi Janet-
It looks as though you have managed your health challenges with grace and spirit. Thanks very much for this post. I’ll be sure to pass along your sentiments to my wife. Do you mind if I ask you a couple of questions?
1) Do you continue to get intravenous vitamin C? If so, where do you live?
2) what brand of curcumin do you take? Daily dose?
3) did you have a hysterectomy because of mets from your colon cancer?
If you choose not to answer, no problem. Thanks again for your words.
David Emerson
ReplyFirst, I must apologize as it was Ron’s posting that I was referring to, so should have read “Ron’s wife”. Can I blame that on chemo brain??
1) Do you continue to get intravenous vitamin C? If so, where do you live?
– Yes I do continue to get IV-C and I live in Ontario, Canada
2) what brand of curcumin do you take? Daily dose?
– Thorne Meriva-SR, 4 capsules/day
3) did you have a hysterectomy because of mets from your colon cancer?
– Yes, the mass was 18cm (7 1/2″) when finally removed in June. Apparently it was the size of a golf ball when discovered in January and why it was not removed then is beyond me. I have since changed oncologists because of that incident.
Are you familiar with juicing and, if so, how many times a day does one juice and are regular meals also eaten?
ReplyHi Janet aka Ron’s Wife-
While my own chemobrain has improved over the years I continue to blame lots on it. Yes, you can blame chemobrain.
Thank you for providing the info above. As for your question “Are you familiar with juicing and, if so, how many times a day does one juice and are regular meals also eaten?”
Yes, I am familiar with juicing. I will assume that you are asking about juicing as a serious therapy and not about juicing for general nutrition.
When I have communicated with or read about cancer patients juicing as a therapy, there has never been any mention of eating regular foods. I have always assumed that people also eat solid foods. In particular, a multiple myeloma patient named Michael Gerin-Tosh juiced carrots daily for years. Lots of carrots… He wrote a book about it. Perhaps there is talk of solid foods.
I hope this helps. Thanks.
David
ReplyI would like to know if my wife has a fighting chance she has stage 4 colon cancer and after surgery they said she has 21 spots in her liver she,s been on chemo for 1year and 9 months they had gave her 2 years to live.she still looks the same the only thing is she lost her hiar,and very stressed,sometimes I wonder if they missed diagnoused her.recently they started a stronger chemo,they said the cancer is not responding to the chemo she was getting,now I,m worried maybe they want to put her down faster,i am very frusterated,I even googled the doctors name and found that there is not too much good to say about her.
ReplyHi Ron-
I am sorry to read of your situation. Cancer, any cancer, is difficult. Stage 4 colorectal cancer is an especially difficult situation. Let me know if you have any questions.
Hang in there- David Emerson
Several issues.
First of all, I always believe that all cancer patients “have a fighting chance” as you say. I was terminal back in 1997 and my cancer is considered incurable by oncology.
Like me, you and your wife face long odds. By this I mean that conventional oncology has little to offer you. As you know, the five year survival rate of a stage 4 colon cancer patient is not great.
The challenge you describe in your email, that your wife’s cancer is not “responding” to chemo not unusual in colon cancer. The key, in my experience, is identifying “integrative” therapies. I’ve listed some examples below. Curcumin is a nutritional supplement that has been shown to ENHANCE 5-FU while it reduces toxicity.
The challenge that you will face with your wife’s onc. is that while these integrative therapies are evidence-based, they are not approved by the Food and Drug Admin. and therefore may not be prescribed by your onc.
5-FU and green tea extract-
5-FU and omega 3 fatty acids-
Oxaliplatin and curcumin-
https://www.google.com/search?q=5-Fluorouracil%2C+curcumin&ie=utf-8&oe=utf-8&aq=t&rls=org.mozilla:en-US:official&client=firefox-a&channel=sb#channel=sb&q=neuropathy+curcumin+oxaliplatin&rls=org.mozilla:en-US:official
Oxaliplatin and omega 3s” target=”_blank”>Oxaliplatin and green tea extract-
Hello David,
I am from the province of Québec, Canada, near Montréal. I’ll start by saying that, English not being my native tongue, there may be words or expressions that can seem a little strange, please forgive me in advance.
Last January, my husband was diagnosed with multiple myeloma, with total kidney disfunction (caused by the proliferation of cancer cells within). January 6th, he began a chemio treatment (along with daily dialysis), Velcade with dexamethasone. After 4 months of contiuous treatment by injection, the counts were down to 1700 (14000 at the beginning). The treatment stopped functionning suddenly, in May. It had taken 4 months to go down from 14000 to 1700, but only one to jump back to 9000. Jean (translated by John, in English) was then started on Revlimid, also with dex. First cycle, excellent news, looks like it’s working, counts are down to 500. I have to mention that plasmacytomas were regularly appearing, for which he had to undergo radiation therapy, 9 on a 5 month period. The one on his face disapeared totally, the other one, on his chest having reduced by more than half.
In the middle of June, I noticed that pain was coming back to his limbs, he was increasingly tired, and the mass on his chest seemed to increase in volume. On June 15th, he was back in the hospital, for a severe pneumonia. The second cycle coming to an end, he encountered a delay in treatment, which was resumed on June 18th. Back at home, the situation got worse (fatigue, loss of appetite). The appointment with the oncologist was scheduled for July 15Th. I asked that it was moved, I wanted to know, really, which, of the desease or the treatment, was to win the battle…
For a few months now, Jean was back to three dialysis treatments per week, on Mondays, Wednesdays and Fridays. I asked to see the doctor on either a Wednesday or a Friday, days on which I work from home. The other option was to see her at the dialysis department on one of those days while Jean was being treated.
This last Friday, when I went to pick up Jean after his treatment, I learned that she came to see him alone, despite my instructions to be called. I wanted to be there… Jean would not tell me immediately what she told him. We went to have lunch and, back at home… well, my world fell apart. Revlimid also stopped working. Prognosis: 3 to 6 months, at best.
What I don’t quite understand is that dialysis is still on, three times a week. The doctor told Jean that there could be an experimental treatment in Montréal, but that he probably wouldn’t be eligible, not residing on the island. How can geography dispose of a human’s life?
I read about compound 11, also about virotherapy, those being tested in the States, but in Canada?
I also heard about cat’s claw, a remedy from Peru, which is starting to be quite reputed to eliminate cancer cells and regenerate the immune system. I have some at home, but I refreaned from using it up until now, having been told that since it can boost cell regeneration, it can boost the cancer cells as well. I don’t know what to do. If I do nothing, he dies, if I do the wrong thing, he dies…
Please help!
Hi Lynn-
It is clear from your communication that you and Jean have had a tough past seven months. I will try to address your questions below but please remember that I too went into partial remission, relapsed, etc. and was given only months to live. Back in 1997. So it is important to remember that myeloma is a tricky cancer that is not well understood.
1) “What I don’t quite understand is that dialysis is still on, three times a week.” Keeping Jean’s kidney’s functioning is important. Keep up the dialysis treatments.
2) “Prognosis: 3 to 6 months, at best.” As I mentioned above, this is conventional oncology’s thinking. Yes, Jean’s situation is serious. But please do not give up all hope.
3) “The doctor told Jean that there could be an experimental treatment in Montréal, but that he probably wouldn’t be eligible, not residing on the island. How can geography dispose of a human’s life?” I have little experience with the Canadian health system.
4) “I read about compound 11, also about virotherapy, those being tested in the States, but in Canada?
I also heard about cat’s claw, a remedy from Peru, which is starting to be quite reputed to eliminate cancer cells and regenerate the immune system.”
With regard to all experimental therapies at this point. Yes, there are a number of non-conventional therapies for MM. Without studies it is difficult to know what may be effective and what may be a scam aka fake. My experience is proof that there is more to MM treatment than what conventional oncology offers but you are on your own at this point.
I will send you several non-conventional therapies that I take myself and have studies that support their efficacy against myeloma but you and Jean need to talk to each other to decide how to proceed.
Please look for my email to your gmail account. Thanks
David Emerson
ReplyThank you so much!
I will do some research on what you wrote in your message. I remember having heard about curcumin being good for the health in general, but never looked into it. Thanks for the links, also…
Lyne
HI Ron-
Yes, I received your email-complicated situation, doing research, will reply asap- David
ReplyHi David
I just found this site. I was diagnosed with state 4 lung cancer which has spread to the bone in my neck. I have had 10 rounds of radiation and now going through chemo. Have had 3 treatments so far and one more is scheduled. I would like to forget the chemo because the way it makes me feel, this is not living. CT scans after the 2nd chemo treatment showed the tumors had gotten smaller. I would rather have quality life than to feel this way what time I have left. Do you think I will be in a lot of pain with my cancer if I do nothing else?
Hi Sandy-
I am sorry to read of your stage 4 lung cancer diagnosis. I agree that quality of life is more important than quantity of life. And yes, aggressive chemo can make anyone feel awful.
Your question “Do you think I will be in a lot of pain with my cancer if I do nothing else?” is difficult for me to answer without knowing anything about you (age, health status, etc.) and your cancer. For instance, cancer metastases can be very painful.
I can certainly provide information about palliative and hospice care if that’s what you want. However, before we go there I would like to provide information and therapies that may make your chemo, radiation or bone mets. more livable. I am saying that I will offer evidence-based therapies that you may prefer.
Cryosurgery for lung cancer
In addition to thinking about cryotherapy for your lung cancer and possibly your bone mets, please consider integrative supplementation for your chemotherapy. For example, the nutritional supplement curcumin has been shown to both enhance certain chemotherapies as well as “chemosensitize” your lung cancer cells- you can then reduce the dose of the chemo and feel better.
http://www.ncbi.nlm.nih.gov/pubmed/?term=curcumin%2C+oxiliplatin%2C+lung+cancer
My point is, your onc. will only discuss what his/her hospital provides and what the FDA has approved. This does not mean that there are not other evidence-based therapies for you available.
Let me know if any of this interests you or if you have any questions.
thanks and hang in there.
David Emerson
ReplyDavid
I am a Canadian who was diagnosed with adenocarcinoma in the distal common bile duct two weeks ago.
I am now waiting for a PETscan and then (things move fast..?) they say my only chance is a Whipple surgery, which is dangerous and life shortening on its own, so any alternative therapies and thoughts are welcome.
I have given serious thought to trying “Phoenix Tears” an edible cannabis oil. What do you think?
thanks
Mark
ReplyHi Mark-
I am sorry to read of your cancer diagnosis. Several things for you to think about re your questions-
1) First and foremost, bile duct cancer is rare and therefore not much is known about it. The page linked below talks about the
Whipple procedure as being potentially curative. I understand your concern about surgical procedures such as this being dangerous but considering the seriousness of your cancer, you are doing well to have the option of a therapy that may cure you.
2) Even if you choose to have the surgery, your five year survival rate is still limited as the second article linked below discusses. The PET scan may help determine if your cancer has spread.
3) Again, even with the surgical removal of the tumor and therefore reducing your tumor burden, you may want to consider complimentary therapies to further reduce your risks of relapse. I will link any and all evidence-based therapies below- I will include those therapies that apply to pancreatic cancer as it is closely related to bile duct cancer.
Treatment of distal bile duct cancer
“Regardless of node status, most patients receive chemotherapy, radiation, or both after surgery. However, cancer specialists have differing opinions on the best combination and the best drugs to use.”
Bile duct cancer/Cholangiocarcinoma- curcumin as therapy
Integrative therapies may be the answer in pancreatic cancer-
The research I did for CBD or cannabis, etc. for both bile duct and pancreatic cancer returns many patient testimonials though I could not find any large trials. Therefore it is difficult for me to give you any real info or opinion. If there are therapies that you believe are relatively inexpensive and come with few side effects then, in general, I think it is okay to pursue them.
Let me know if you have any questions. Thanks and hang in there.
David Emerson
Reply[…] These are all questions that will need to be answered– hopefully you’ve gotten a second opinion first– and an important but often overlooked facet of this decision making process is an […]
ReplyHello David Emerson,
I am 70 yrs young and have a recent diagnosis of Multiple Myeloma (MM).
Apparently the common kind (IgG). I had a cancerous prostate removed last sept 2014 with no complications.
The hematologist who gave the diagnosis told me at my last visit that he would plan for chemo for 1-per-week for a whole year. I still don’t have a stage number but he said he was happy with my bone survey for now (good news I gather).
I asked if he could put the treatment off till I did a 20 day HBo2 (100% oxygen )therapy to increase my stem cell count and that I would also be doing some natural herb intake (Red Reishi Mushroom extract and essence), Flor-essence liquid detoxifier (includes about 8 herbal extracts),and Immunocal powder. These are daily intakes at a minimum.
He told me that I could do whatever I wanted but that HE would not be doing the chemo my way. It was his way or the highway. We parted amicably enough and he will have an oncologists call me to set up a plan.
I am a new member of a non-profit, alternative health organization called “Inspire Health” in Vancouver Canada and look forward to a visit with their MD next week. They apparently have Oncologists that work with them on alternative treatment plans (through The Canadian or British Columbia Cancer Societies I think..?)
My question for you is:
1) If you have current knowledge of the most favorable treatment for MM with Stem cell harvesting and transplantation in mind for elderlies;
2) If you have any positive regard for Hyperbaric Oxygen Therapy (20 treatments for 1.5 Hours Daily at 2.5 ATA) in order to increase stem cell population for harvesting (before chemo) and transplanting (after high dose chemo to kill cancerous bone marrow)?
3) What is the most common MM chemo combination used with Stem cell transplant in mind..? ( may be answered in number 1 above).
Thanks David,
Sincerely, Sanford
ReplyHi Sanford-
I am sorry to read of your MM diagnosis though it sounds as though you are in good spirits and that you have no bone involvement (“I still don’t have a stage number but he said he was happy with my bone survey for now (good news I gather).”
Just my opinion but regarding your onc. “my way or the highway…” you are better off without this dr. An onc. who does not put your needs first is bad.
I agree with your thinking to “prehabilitate.” This means that you are preparing for therapy. Studies show that you will do better with this preparation. I have no experience with Inspire Health but their website sounds as though they will be more open-minded.
Regarding your questions-
1) Treatments to enhance stem cell harvesting- Yes, HBOT has shown the ability to stimulate stem cell harvesting–
2) Yes, I have both personal experience and research experience with HBOT. see the link and studies above- is HBOT covered in Canada?
3) Re chemo combinations for ASCT- as you can see from this link there are many combinations. My understanding is that different cancer centers use different combos- MDAnderson, MSK, Mayo, etc. I don’t know about Canada…
Lastly, if your MM is not severe, please consider managing your MM rather than undergoing aggressive chemo- this is called the “cure vs. control” debate-
With less chemo, less aggressive therapy, you may live longer, enjoy higher quality of life with fewer side effects. Especially if you understand non-conventional therapies such as flor essence, etc.
Let me know if you have any questions-
David Emerson
ReplyGood Morning David:
I was diagnosed with stage 3 triple negative breast cancer in November 2014. I have had 8 rounds of chemo, surgery (left breast mastectomy and removal of 12 nodes) and will be starting radiation shortly.
What do you recommend as supportive altertive therapies or suppliments that have some scientific evidence in reversing this type of cancer or preventing metastisies?
Triple negative breast cancer is the most aggressive breast cancer and is HER2 , ER and PR negative so few treatment options.
Thank you
Carol
ReplyHi Carol-
I an sorry to read of your triple neg BC diagnosis. However you appear to be working hard to manage your cancer. Regarding your question of supplementation to reverse or prevent mets, I will link the info below-
Flaxseed and vitamin D for triple-negative?
Omega-3 Fatty Acids Slow Triple-Negative Breast Cancer Cell Proliferation
Curcumin and TNBC-
Distinct roles of different forms of vitamin E in DHA-induced apoptosis in triple-negative breast cancer cells.
Please read the info above and let me know if you have any questions. I will do more research tomorrow.
thanks
David Emerson
ReplyHi Carol-
I wanted to follow-up with another therapy for you and your onc to consider. I have been researching the effect of bone health, bone mets in various cancers. Intravenous bisphosphonate therapy is standard for multiple myeloma patients like me.
Please read and consider bisphosphonate therapy BEFORE you have bone involvement. You are already thinking about this in your question “or preventing metastisies?” The studies linked in the post below discuss this possibility in breast cancer. This therapy is not standard so I don’t know what your onc is going to say. Can bisphosphonates PREVENT bone mets for early Breast Cancer simplifying treatment?
“Conclusion Low-dose oral bisphosphonates administered for prevention or treatment of postmenopausal osteoporosis were associated with lower risk of skeletal metastasis in patients with early- or more advanced-stage breast cancer.””
Please let me know if you have any questions.
David Emerson
ReplyMy husband was diagnosed with Esophagus cancer, Stage 1 with a level of T4. The first Dr said total removal of esophagus and partial stomach. 2nd Dr said chemo and radiation to shrink it and then we will see what type of surgery. 2nd Dr referred us back to our hometown for treatment but will take a week to get an appointment. Any thoughts or any sites I should be reading up on. Thanks for helping so many.
ReplyHi Jennifer-
I am sorry to learn of your husband’s cancer diagnosis. Seeking a second opinion indicates that you are learning about his situation and choices and studies indicate that your decision-making will improve as a result.
While EC stage 1 level 4 is a lot of info there are other issues that both oncs can take into account that I cannot. However I can research the two basic approaches recommended by Dr 1 and Dr 2 in terms that may aide in your decision-making.
You and your husband will have to think through both recommendations in terms of 1) overall survival and 2) quality of life. Dr 2’s recommendation of chemo to shrink the tumor and then surgery will be harder on your husband. No surprise here. The chemo regimens in the studies below are highly toxic and you must consider your husband’s age, health, etc. At the end of this post I will link studies that examine integrative therapies to both enhance the efficacy of the chemo will reducing its toxicity.
The overall survival issue is how long, on average, will your husband live when comparing both therapies? Sorry to be so direct but I think this is what you want to know.
Survival benefits from neoadjuvant chemoradiotherapy or chemotherapy in oesophageal carcinoma: a meta-analysis.
“NTERPRETATION:
A significant survival benefit was evident for preoperative chemoradiotherapy and, to a lesser extent, for chemotherapy in patients with adenocarcinoma of the oesophagus. The findings provide an evidence-based framework for the use of neoadjuvant treatment in management decisions.”
Also, regarding your comment “2nd Dr referred us back to our hometown for treatment but will take a week to get an appointment.” I think your husband should use the time to “prehabilitate.”
Cancer Prehabilitation Improves Outcomes
If you choose to undergo chemo before surgery (preadjuvant chemo) if you email me the names of the chemos your husband will be taking I can research integrative therapies- examples would be antioxidant supplementation such as curcumin or grape seed extract- supplements that you can buy online and take morning and night to help your husband with both the chemo and the surgery.
Your onc may not like this but evidence-based research may convince you. If you choose to I can relay these studies. Let me know.
There is a lot of info here. Let me know if you have any questions.
thanks
David Emerson
ReplyHi David,
I am a 48 year old man in Vancouver, Canada. I recently had a swollen lymph node removed from my neck and the post op biopsy showed that cancer was present. Yesterday, a physical exam with a camera confirmed that cancer is also present at the back of my tongue on the side where the Lymph node was removed.
The oncologist who discovered the cancer on my tongue is recommending aggressive radiation for a 7 week period and has said that adding chemotherapy on top of the radiation would give me the best chance of beating this. But adding chemo comes with some harsh side effects, including a feeding tube as he says that I will almost certainly be unable to swallow (with both radiation and chemo combined).
Since he seems to be saying the chemo is up to me, I’m wondering if there is any information available about the difference in success rates / survival rates of just opting for radiation vs the combination of radiation and chemo? How do I make such an important decision when I have no first hand knowledge of cancer treatment?
John
ReplyHi John-
The more specific you are with your diagnosis the more specific I can be. The risk you take with your therapies is often a result of how much risk your cancer diagnosis presents. The five year survival stats below give you a general idea of the spread of five year survival risk for the location, tongue vs. floor of the mouth, and then local vs. regional. Presence of cancer in one lymph node may mean “regional” or may still be local as the node is near the tumor site.
Any info you can give me will help my research. Let me know and hang in there.
David Emerson
Tongue
Stage
5-Year Relative Survival Rate
Local
78%
Regional
63%
Distant
36%
Floor of the mouth
Stage
5-Year Relative Survival Rate
Local
75%
Regional
38%
Distant
20%
ReplyDavid, thanks for the quick reply. I had a petscan today and should have the results within a day or two. I’ll get back to you then and will be as specific as possible.
John
ReplyHello David,
First I want to thank you for your advice to me previously when I asked whether to go with a younger oncologist which would allow me to see him 3 weeks earlier than an older, more experienced oncologist. I decided to take the earlier appointment and saw the younger oncologist. It worked out fine for now. I have more questions for you which I hope you can help me with.
I was diagosed with Stage 3 cancer. Just to re-cap, when doing a biopsy on my small bowel, the surgeon found a 10 mm mass which turned out to be adenacarcinoma (which I’ve been told is more commonly found in the colon and not the small bowel). They removed this mass. They also found 3 benign lymph nodes and 1 lymph node which had adenacarcinoma. They have ordered a catscan for me (to scan lungs, liver, the abdominal area). I’ve already waited 2 weeks and the catscan still hasn’t been scheduled yet.
I called up a private imaging centre and was told that doing a petscan is the best way to see if the cancer is in any other lymph nodes in my body. However, doing an MRI is better for seeing what’s in the organs. Therefore, it would seem that doing both would be prudent. I’m in Canada, and fortunately our health care system would cover the cost of both, BUT, I understand the wait list is very long (could be months). I already called my oncologist and asked if he could order me a PET/CT and MRI. He said after doing the catscan, he would decide whether to order a PET/CT for me. Doing the MRI and PET/CT at the private centre would be expensive, but they could do it next week. My question is, in my situation, is it urgent that I do the MRI and PET/CT as soon as possible or can I wait? If I can wait, how long can I wait? If it’s detrimental for me to wait months for the MRI and PET/CT then I will try to come up with the money to do these tests privately as soon as possible.
The oncologist said that unfortunately, there is not much data on small bowel cancer. Is this true? As such, the oncologist is going to treat me as if I had colon cancer. The oncologist has recommended I have oral chemotherapy: Capecitabine(or XELODA) and GIAJFFOX (Gastroinstestinal, Adjuvant, Fluorouracil, Folinic Acid, Oxaliplatin). Are these aggressive chemo treatments? My concern is that we don’t even know if the cancer has spread to other lymph nodes and organs, so I don’t like the idea of killing my good cells when we have no information as to where, if any, it’s spread.
A third question I have is about Graviola. I’ve been told by a friend that he went to the Amazon to get the bark for this tree, which when combined with water to make a tea helps greatly in the treatment of cancer. Can you please give me your opinion about this? I should tell you that I’m a kidney recipient (my friend donated his kidney to me 2 years ago) so I’m on immune suppressant drugs the rest of my life. Anything I eat or take as supplements MUST NOT boost my immune system or counteract with my immune suppressant drugs (tacrolimus and mycophenalate) or it could result in the loss of my kidney. As such, I have to be vigilant about what I eat and take as supplements.
Grateful for your help, David.
Best regards,
Michelle
P.S pathology report still hasnt been revealed to me I will get my hands on it Monday, but pathologist said to thoracic surgeon limited small cell he said no surgery he recommended chemo and radiation, then said maybe just chemo and referred me to oncology who as of yet hasnt called me for a consult, hence my faith is telling me, I dont need them! I can do this myself, with someone who can coach me and direct me to things that work for the lungs and lymph nodes, as he only did a biopsy on my R10 and 11 node, and a lavage of of my right lower lobe which was sent off for cytology, so the only thing I know from all of this is small cell, limited on the R10 and or 11 node…nothing on the nodule in my lung altho he said he wouldnt have to operate on my lung? So confusing lol, and reaffirms my conviction they can make a bigger deal out of me if they think I will take their advise and treatment!! When they see in my eyes, i’m not afraid, and not reacting to what their saying, what they say, changes!
ReplyHi David, thank you for your response, pathology isnt complete, but limited small cell in my right lymph node, and im in the process of getting myself into the cancer treatment centers of america, they do genomic testing, and a lot of eastern methods, holistics massage acupuncture, nutrition, and herbs. My suregon said beware of places who have to advertise on TV, hes from Dana Farber, and I have seen 3 commercials for Dana Farber in the past day and a half!! I dont understand what agressive means exactly in terms of time, as I am working on insurance, and getting myself set to go to a place I feel can do the best for me, also I did some rekki[spell check] and am proactive with my diet, all advise is welcome from you, have a good day 🙂
ReplyHi Laurie-
I have no personal experience with CTCA but they say all the right things in their ads- things like genomic testing, massage (I do this), acupunture (I do this), nutrition, yes, and herbs, again…yes. And while I agree with your surgeon, I know of dana-farber and think highly of them. Of course they are totally conventional so keep that in mind.
By talking about insurance, etc. it tells me that you are getting organized and prepared. As for the meaning of aggressive, I apologize for not being more clear. It is a matter of whether or not conventional therapy is “curative.” Meaning can your surgeon and onc give you a reasonable chance of actually curing your cancer. In my case, multiple myeloma, no, conventional oncology is not curative.
Knowing this, I chose to pursue the full spectrum of therapies. This is all I am saying.
Laurie, please keep me posted, let me know if you have any questions or if PBC can research anything for you. Thanks and take it easy.
David Emerson
ReplyHi David,
Getting the run around with ins and primary care not supporting me, I fired him and am on to a new PC and apricot seeds, cyruta plus, bit of baking soda in 1 glass of water a day, and a few other implements in my diet and my soul, as far as making an appointment for acupuncture. Im sure you see where i’m going with this diagnosis, and appreciate any advice here, or in email from you. Enjoy your weekend! Faith and knowledge are the tools we need. I am believing that more and more as each day passes 🙂
Hi David
Im a 58 yr old woman who just got diagnosed with stage 3a small call cancer in my lung and lymph node. I am looking for alternative therapy, I am not a fan of chemo, radiation, or the odds. Please direct me somewhere near MA not that I would mind the travel, This must leave my body!!! Thanks in advance for your help
Hi Laurie-
I am sorry to learn of your NSCLC diagnosis. Since you are stage 3a I will be direct with you. As you have noted, your odds or five year survival rates are not great. Please understand that this only means that conventional oncology does not offer much or anything in the way of curative therapy.
Because non-small cell lung cancer is considered aggressive I think that you should consider a spectrum of therapies– some conventional, some integrative, and some alternative. Meaning, to truly beat your cancer I would throw everything but the kitchen sink at it. But this is just my approach…
In your post you did not mention surgery. If you can reduce your tumor burden, even though, as you point out, your cancer was found in your lymph node, I would consider surgical therapy.
Are you willing to consider an immunotherapy drug (keytruda or xalkori) if your NSCLC indicates a genetic or molecular match? In order to know this you must have your cancer genetically tested.
In addition to pursuing immunotherapy, please consider integrative therapies. By this I mean that supplementation such as curcumin or green tea extract has show the ability to enhance the efficacy while reducing the toxicity of specific chemotherapies.
There are integrative therapies for both radiation and chemo- I need to know what your onc recommends, what you may consider, in order to research these integrative therapies for you.
As examples, both curcumin and green tea extract have shown evidence-based ability to both enhance certain chemotherpies while reducing toxicities.
Curcumin as integrative therapy
Green tea as integrative therapy-
milk thistle as integrative therapy-
Laurie- these are just examples of what I am talking about. NSCLC when diagnosed at 3a can be aggressive and I believe that you must be aggressive in your thinking, aggressive in our treatment.
I hope this info helps. Let me know if you have any questions.
thanks and hang in there.
David Emerson
Reply[…] Getting a different kind of Second Opinion- […]
ReplyI am a 66 yr old male who had a complete left lobectomy for lung cancer.After surgery my heart shifted over into the empty space, and now my DR wants to put a protheses in to push my heart back over. my question is if you are aware of this type surgery and where i can information on it. I am scheduled for surgery June 1st. This will be the third time i had surgery on this site through same entrance thru my back under left shoulder blade
ReplyHi Paul-
You pose and interesting question. Since I have no previous experience with this issue I can do two things. First I will post a link to an forum discussion about lobectomy and resulting organ shifting.
Organ shifting discussion click here-
I had to sign in to Inspire to read the posts so I imagine you will too. It is free. The people who post are all who had the same surgery and talk about pain from the surgery. It sounds as though every lobectomy patient experiences some shifting or organs but no one talks about a prostheses to keep one’s heart in place.
Secondly, I suggest you have a discussion with your doctor about the prosthesis. He must be able to present reasoning to you that convinces you of
1) the benefits outweigh the side effects-
2) less is more- you mention two previous surgeries to the site- a third will carry potential risks-
I hope this helps. Let me know if you have any questions.
thanks
David Emerson
ReplyHi there- if you can help I would be so appreciate! My stepdad has been recently dignosed with stage 4 lung cancer with met to liver—:( recomeded therapies are chemo and radiation.
I am reading this often does not work but I of course cannt argue with oncoligisty etc. I am wondering what therapies(natural or otherwise) you may know of that could be a help. He is 69 yrs old and needs all help we can get. I have suggested he suPplemtn with cucumin,fish oil and pomegranate extract- what are your thoughts on this? I also thought perhaps vit C therapy could help? He is wonderful man and I want to help load him with all options not just what oncoligist has mentioned- please help- appreciate your time and Congrats on your recovery!
Hi Manda-
I am sorry to read of your stepdad’s lung cancer diagnosis. I will be direct with you. Lung cancer diagnosed at stage 4 does not have very positive 5 year survival averages. Since I am not a certified physician, I cannot prescribe medicine.
However I can tell you what I would do if it were my stepdad. I would utilize, pursue and otherwise try every evidence-based therapy that I could research. Yes, curcumin, omega 3 fatty acids (fish oil- Carlson lemon flavored is what I take) and vitamin C. Intravenous vitamin C if you can find a center that you trust.
The supplements that I will list have been shown to fight lung cancer on their own. Further, many of these supplements have been shown to enhance the efficacy of certain chemos while they moderate their toxicity.
Yes, I would encourage my own stepdad to try conventional therapies. The study linked below is an example of curcumin ENHANCING the efficacy of carboplatin.
Curcumin sensitizes human lung cancer cells to apoptosis and metastasis synergistically combined with carboplatin.
http://www.ncbi.nlm.nih.gov/pubmed/25716014
Green tea extract as well-
http://www.ncbi.nlm.nih.gov/pubmed/?term=lung+cancer%2C+green+tea
Grape Seed Extract-
http://www.ncbi.nlm.nih.gov/pubmed/?term=lung+cancer%2C+grape+seed+extract
Silibinin- aka Milk thistle-
http://www.ncbi.nlm.nih.gov/pubmed/?term=lung+cancer%2C+milk+thistle
I would have my stepdad walk briskly for about 30 min a day. I would have my step dad eat little if any red meat, refined sugar, maybe a glass or two of red wine weekly.
If my stepdad’s oncologist recommended local radiation I would have my stepdad supplement with a combination of systemic enzymes call Wobenzyme N- http://www.ncbi.nlm.nih.gov/pubmed/?term=lung+cancer%2C+wobenzyme
I would figure out some long term goals for my stepdad- I would talk about my son Alex’s graduating from college, getting married, etc. Studies show the importance of mind-body therapies like goals, need to live, etc.
Manda, I have thrown a lot of info at you in one email. I hope you will reply with questions if you have any. Lastly, all of the supplements linked above can be found on Amazon. Or you can go to your local health food store.
Let me know if you have any questions.
Hang in there.
David Emerson
ReplyI’d like to know the odds for a lumpectomy with radiation vs lumpectomy without radiation in a 67 year old DCIS Stage O with a negative BRCA. Also considering prophylactic mastectomy with reconstruction because the breast tissue is so dense the mammos are very difficult to read, so follow up will be challenging. Thx.
ReplyHi Ceci-
I am sorry to read of your BC diagnosis. Although as you have mentioned, you are stage 0 and your risk of relapse, with or without therapy, is quite low.
To address your question “I’d like to know the odds for a lumpectomy with radiation vs lumpectomy without radiation in a 67 year old DCIS Stage O with a negative BRCA.” I will link a blog post with 4 studies in it that will speak to your situation. I will try to anticipate your thinking before you ask. You are not 70 and therefore not quite in the study demographic. If I read two of the studies correctly, radiation reduces the risk of additional cancer by less than 3%. Keep in mind that there is a risk of side effects that accompany local radiation.
Does Radiation in Elderly Early-Stage Breast Cancer Patients help?
“If you are diagnosed with early stage breast cancer, are 0ver 70, have a lumpectomy to remove the cancer, take tamoxifen for 5 years after your surgery, studies show that radiation will reduce the risk of relapse modestly (3%).
If a very small percentage of breast cancer survivors get breast cancer in there other breast, will they die of breast cancer? Will the local radiation cause side effects such as heart damage that may cause more harm than the 3% relapse?…”
Also, regardless of your decision to pursue conventional therapies, please read the linked post below to learn about those non-toxic, inexpensive therapies to dramatically reduce relapse risk to early stage BC.
Slash breast cancer risk, slash breast cancer risk of relapse?
As for your comment about a mastectomy because of dense breast tissue, you are correct that dense breast tissue makes it more difficult for oncs to read mammograms. You are not really asking a question about this so I will assume that by mentioning this issue you are sort of talking out loud.
So diagnostic info that may help you with your decision-making, please consider testing your current DCIS for it’s aggressiveness with the Oncotype DX breast cancer assay. My understanding is that if your onc prescribes this test your insurance will pay for it. The test will give both you and you onc more info to help with your decisions.
Oncotype DX for Breast Cancer- better than a second opinion?
I hope this helps. Please let me know if you have other questions. Take it easy.
David Emerson
ReplyI wanted to say the tumor is stable (not stale) I am sorry for my grammar English is my 3 language
ReplyHello David Emerson,
Would you please give me any advice. I have a Desmoid Tumor since January 2014and my doctors are telling me that I have to have a surgery done and that is my only option. The surgery is terrifies my it is will be really big like there saying. this is my Resent MRI findings:
FINDINGS:
Again identified is a mass that appears to be centered on the rectus muscle beginning at the superior pelvis and extending inferiorly. It produces a mass effect on the urinary bladder. The mass has increased slightly in size. It measures 11 cm in
craniocaudad diameter compared to 9 cm as measured on the sagittal image 12, series 12. The mass enhances homogeneously. The mass measures 7.3 cm in AP diameter as measured on the sagittal image 12, series 12 were on the prior study it measured 6 cm. On
series 3 image 18 the mass measures up to 13 cm in transverse diameter and 7.7 cm in AP diameter. This is also demonstrated slight interval increase in size.
No new masses are identified. The uterus and adnexal regions appear unremarkable. No pelvic fluid is evident. Other than the mass effect on the urinary bladder this appears unremarkable. No gross adenopathy is seen.
Visualized osseous structures appear unremarkable. Right now I fill that my tumor stopped growing and it is stale
I am taking
Vitamin D3 ,Vitamin C, Curamed,. would you please suggest any ting. Thank you for your time. I am Female 29 years old.
Hi Khanifa-
To be clear, I am not a physician. I am a long term cancer survivor.
There is a lot of info for you below. Let me know if you have any questions. The good news is that your desmoid tumor, according to the info linked below, is not cancerous/will not metastasize. While surgery is the most common therapy, there is a documented risk of relapse. Meaning there is a good chance the tumor will grow back. Desmoid tumors are rare and it is recommended that you find a center with experience with desmoid tumors aka aggressive fibromatosis.
The first link will take you to a number of articles and studies about non-surgical procedures including cryotherapy and radio frequency ablation. From my reading, these therapies may be successful yet they are largely untested.
“Treatment
“Treatment may consist of watching and waiting, complete surgical removal, radiation therapy, antiestrogens, NSAIDs, chemotherapy or microwave ablation.
A biopsy is always indicated as the definitive method to determine nature of the tumour. Management of these lesions is complex, the main problem being the high rates of recurrence in FAP associated disease. Conversely, for intra-abdominal fibromatosis without evidence of FAP, although extensive surgery may still be required for local symptoms, the risk of recurrence appears to be lower.[8] Wide surgical resection with clear margins is the most widely practiced technique with radiation, chemotherapy, or hormonal therapy being used to reduce the risk of recurrence.[7]”
http://en.wikipedia.org/wiki/Aggressive_fibromatosis
“If you are diagnosed with a desmoid tumor it is recommended that you be evaluated in a major, academic hospital with experts in sarcoma. These hospitals are usually designated as NCCN (National Comprehensive Cancer Network) centers. Patients with desmoid tumors should be evaluated by a multi-disciplinary team of surgeons, medical oncologists, radiation oncologists, geneticists and nurses”
http://www.dtrf.org/index.php/about-br-desmoid-tumors/about-desmoid-tumors.html
Please let me know if you have any questions. Take it easy.
David Emerson
ReplyI have had a mastectomy on my left breast, the diagnoses was 2 invasive carcinoma sites. Only 1 lymph node was removed and it showed clear. My onco. was 2. My question is the oncologist at first said I didn’t need to take anything or have chemo or radiation.
Then he changes his mind and wanted me to take tamoxifen or arimidex both caused me lost of side effects,( I have Rheumatoid arthritis so the joint pain was bad)so should I get a second opinion or should I just forget about taking any meds?
Hi BC survivor-
I am sorry to read of your bc diagnosis though as you have identified your BC is at an early stage. Each therapy you mention from mastectomy to chemo (tam or ari) to radiation lower your risk of a BC relapse. To give you info and research that is specific to your situation I need a stage.
If your diagnosis was BC stage 1 and your BC has not spread, as you say your lymph node was clear, (what to you mean by “My onco. was 2?) then each additional therapy recommended by your onc is meant to reduce the already low risk of relapse even lower. Further each of the recommended therapies, chemo and or radiation brings the risk of side effects.
For instance, joint pain is a known side effect of arimidex. Therefore taking more meds or additional therapies has risks (side effects) or benefits ( reduce the risk of relapse). Yes, a second opinion may help you make this decision.
Please consider two things which may help you think through your situation.
1) To give you more info about the aggressiveness of your BC- please consider Oncotype DX to analyze your risk of relapse. Click and read the post linked below0
Oncotype DX for Breast Cancer- better than a second opinion?Oncotype DX for Breast Cancer- better than a second opinion?
2) please consider non-toxic therapies to reduce your risk of relapse- click and read the post below-
Slash breast cancer risk, slash breast cancer risk of relapse?
Let me know if you have any questions. Thanks and hang in there.
David Emerson
ReplyI was just diagnosed as follows: vocal cord, right false, laryngeal surface of epiglottis, biopsy: squamous cell carcinoma, moderately differentiated, invasive.
Doctor told me it is a very small spot that the cancer is originating from (which she says is good news).
My question: she suggests I have radiation (I have already met with a Radiation Oncologist).
My problem I am very claustrophobic. I have already had a simulation done of the radiation, with mask, etc. It was freaky.
I am wondering if chemo would be a better treatment … or even some holistic natural treatment.
Thank you for whatever info you can give me.
Linda-Marie
ReplyHi Linda-Marie-
I am sorry to read of your cancer diagnosis. It seems that your main concern is individual in nature (claustrophobic). I relay info based on studies about cancers- I am not well versed in the type of issue that you mention. Translation- I’m not sure what to tell you…ask your onc about local surgery? See the info below.
Keep in mind that the key piece of info that your dr. must report to you (and you to me) is if your cancer is “systemic” or has spread. I will assume that if your onc is recommending local radiation only, that your cancer is NOT systemic- it has not metastasized.
The wikipedia explanation covers the basics- http://en.wikipedia.org/wiki/Laryngeal_cancer#Staging
While this study relates that local radiation is the standard therapy for early stage laryngeal cancer (you I think) the study linked below questions a small percentage of patients who do not control their cancer with this therapy.
Please ask your onc about the small percentage of similar patients in this study who were NOT successfully treated with local radiotherapy-
“Seventy-five percent of T1 (3 of 4) and 70.6% (25 of 35) of T2 supraglottic cancers were successfully controlled by radiotherapy.
“Salvage surgery was attempted in five patients; however, all patients except one died of disease.
CONCLUSION: Although radiotherapy is a standard treatment for early laryngeal cancers, the results of this review may suggest considering other modalities in the treatment of early laryngeal cancer.”
http://www.ncbi.nlm.nih.gov/pubmed/19755083
Let me know if you have any more questions.
David Emerson
ReplyHello,
During routine checkup there were 2 tumor found in my dads intestine, the doctor suggested surgery to remove them. Now the surgery has been performed successfully and one tumor was like mushroom and other a bit bad. The doctor said its between stage 2 and stage 3, he also mentioned that if we scan him there will be no sign of cancer. But the oncologist is still suggesting he goes for chemo to ensure any cancer cell is destroyed.
After reading so many posts about 2% effectiveness of chemo, i am confused, should my dad go for chemo or any other alternatives?
He is 72 years old.
Thanks,
Ali
Hi Ali-
I wrote a blog post to answer your question. Please click here-
ReplyI have been diagnosed with bladder cancer oct. 2013 superficial, aggressive,now stage 3, but positioned at both sides of exit to bladder as well as other areas.Have had 2 resctions and am now being treated with bcg third round but did without treatment last year owing to global shortage of bcg. Question . How does the position of the cancer affect the removal of the bladder hopefully for a neo bladder and what are the chances of metastasis at this point?
ReplyHi Allison-
I am sorry to learn of your bladder cancer. If I read your question correctly you are asking about multiple sites within your bladder? And by “bcg” you mean http://www.webmd.com/cancer/bladder-cancer/bacillus-calmette-guerin-bcg-for-bladder-cancer”
I believe that bcg is only given for non-invasive cancers. Ask your onc but I don’t think you would be a candidate for bcg if your cancer had metastasized. As for a neo bladder, I assume that you are considering this procedure as your next step?
If so, my understanding of a neo bladder procedure is that your entire bladder will be removed. Again, this procedure involves only non-invasive bladder cancers. Yes, you may have multiple cancer sites within your bladder but according to the info linked below, the bladder cancer sites are all in the bladder and have not metastasized.
http://www.mayoclinic.org/tests-procedures/neobladder-reconstruction/basics/definition/prc-20013721
“If you require complete bladder removal, you may be a candidate to have a neobladder reconstruction. Determining if this procedure is right for you depends on several factors, such as:
Your age and overall health, particularly your kidney function
Extent of your bladder cancer
Previous radiation or surgery to the bladder or prostate, which may affect the ability of the bowel to heal correctly after creation of a neobladder
Your willingness to deal with catheters and tubes after surgery
Your doctor will review the risks and benefits of neobladder reconstruction with you and will discuss whether you’re a candidate for this procedure. Neobladder surgery is not an option if you have cancer of the urethra.”
Let me know if you have any other questions.
Hang in there,
David Emerson
ReplyI was diagnosed with Mucinous Carconoma. I had my lumpectomy and all of my pathology reports are great. Lymphnodes clear. Tumor was 1 cm…margins and rims clear. OncotypeDx = 8.
My oncologist is recommending radiation. My cancer was on the left side and I have concerns about my heart and radiation.
Is radiation always necessary?
thanks
ReplyPS…Oncologist is recommending radiation AND Arimidex (sp?) for at least 5 years.
ReplyHi Debbie-
You are asking about a large and important area of cancer care. I am going to treat your question as a blog post on pbc. I will email you a link tomorrow. thanks. David Emerson
ReplyThanks for your response. I forgot to add that my cancer, Mucinous Carcinoma was Stage 1A.
I look forward to your blog post.
debbie
ReplyI have the same diagnosis & staging as Debbie M. above, Mucinous Carcinoma Stage 1A. Grade 1, no positive lymph nodes. Lumpectomy on 2/2/15 and currently undergoing 3 weeks of radiation. Very interested in your comments. Discussed possibility of radiation boost at end of therapy with radiology onc today- he says treatment is adequate without it, but I can have the boost if I want it.
ReplyAlso forgot to mention they found a low grade DCIS as well within the same area and it was removed. I will be starting Tamoxifen after rads, we decided against Aromatase inhibitors because of other health issues.
ReplyHi Lisa-
I am sorry to learn of your BC diagnosis though you seem to be on top of your therapies.
If I understand both comments, you were diagnosed with both a Mucinous Carcinoma Stage 1A Grade 1 and a low grade DCIS? You had a lumpectomy, and you are currently undergoing local radiation. Also, you anticipate Tamoxifen after the radiation. While you don’t ask a specific question you do say you are interested in my comments and you raise the possibility of a radiation boost.
All of your therapies are shown to reduce the already low risk of BC relapse. In other words, both of your BC growths were contained and a lumpectomy reduced your risk of further BC. Local radiation and Tamoxifen further reduces your risk of relapse.
While I have never read specifics, most studies that examine radiation and Tamoxifen for contained BC raise the issue of side effects- heart damage, secondary cancers, pain, etc. So the issue of a radiation boost is a matter of a small increase of risk balanced by a small increased risk of side effects. I agree with your radiation onc- your local radiation therapy is adequate without a boost.
The only other evidence-based therapies for you to consider are listed in the post linked below. Many, many studies cite a reduced risk of BC relapse with regular moderate exercise, little or no alcohol, others listed below. All are non-toxic, inexpensive therapies.
Slash Your Breast Cancer Risk Now!
In sum Lisa, if you pursue the conventional therapies that you list and consider the non-conventional therapies as well, perhaps adopt a few, you are covering all of your bases.
I hope this helps. Let me know if you have any other questions.
David Emerson
ReplyMy dad diagnosed with vocal box cancer. The tumor is about 2 – 2.5 cm. Its at stage 3. We are waiting for his CT Scan report to find out if it has spread elsewhere. My dad is healthy but has diabetes. The oncologist gave us three options: radiation therapy, surgery or do nothing. Which one would you recommend? I would appreciate your help.
Replyhi Jiva-
I am sorry to read of your dad’s larynx cancer. Before I try to address your question I must say that your dad’s health leading up to either surgery. radiation or nothing will depend heavily on his lifestyle- meaning if he eats more fruits and veggies, less red meat, moderately exercises daily, and most importantly, supplements with those anti-oxidants that have been show to act against head and neck cancers.
In response to your question “Which one would you recommend?” since you have been given a stage III diagnosis then your onc has determined that the cancer has only spread to the supraglottis, glottis or subglottis and perhaps one lymph node.
“Stage III laryngeal cancer depends on whether cancer has spread from the supraglottis, glottis, or subglottis.”
http://www.cancer.gov/cancertopics/pdq/treatment/laryngeal/Patient/page2#_46
The choice between radiation or surgery largely depends on how experienced your onc or those surgical oncs he/she works with. The article/studly linked below cites surgical outcomes of laryngeal cancer as superior to chemoradiation but that the outcomes can be similar depending on the cancer center.
“Surgery associated with better survival for patients with advanced laryngeal cancer”
http://medicalxpress.com/news/2014-08-surgery-survival-patients-advanced-laryngeal.html#inlRlv
“Since then, chemoradiation has become increasingly popular treatment because it can preserve the larynx….Patients who had surgery had better 2-year and 5-year disease-specific survival… than patients who did not undergo surgery.”
Please let me know if you have any questions or comments. Thanks and hang in there.
David Emerson
ReplyI was diagnosed with breast cancer on right side in November, 1999. After biopsy it was determined that lumpectomy was best option (stage 1 – grade 3) I had a sentinel and one other lymph node removed followed by chemo and radiation and 5 years of tamoxifen. I have had regular mammograms annually and on 12/30/15 was diagnosed with breast cancer again on left side and this time after ultra sound biopsy and MRI it was discovered that there were two tumors; both stage 1 and grade 3. I had a mastectomy on 2/4/15 and will get the drain removed in a couple of days. Pathology report shows no spread to lymph nodes.
My Oncologist recommends letrozole (AKA Femara)2.5 mg (1 tablet daily) Everything I read says this drug or its cousins can only be taken 5 years.
I am planning to get a second opinion as the side effects are terrible such as bone loss, not being exposed to sun, bone/joint problems, drowsiness causing inability to drive, increase in cholesterol and a bunch of others.
Isn’t 2.5 mg a rather high dosage? I know other women who only take 1. mg.
I would very much appreciate your feedback and where the best facility for a second opinion.
My treatment is at Swedish in Seattle.
Thank you
Yvonne Steed
Hi Yvonne-
I am sorry to read about your breast cancer relapse. You are facing a sort of double edged-sword. It is difficult to have a BC relapse after you underwent a lumpectomy, chemo, radiation and tamoxifen. The statistical chances of a relapse in your case are quite small. (as an aside, I can relate as I was 1 percent of 1 percent upon my diagnosis but this reply is about you not me…)
Regarding your question about your onc’s recommendation of Letrozole/femara 2.5 tablet daily. “Isn’t 2.5 mg a rather high dosage? I know other women who only take 1. mg.”
First and foremost, you are the patient and therefore you decide as to the type of therapy as well as the dose. Since me and PBC pride ourselves on “evidence-based” research, I will provide research on the question below-
The comments of women in a similar situation to you might be helpful. Several of the women mention a diagnostic test called the onc
https://community.breastcancer.org/forum/96/topic/801767
The Oncotype DX test will result in a number that measures your risk of BC relapse. The test may help you decide how much chemo to have. In other words you may decide to withstand more or less severity/toxicity based on this test.
http://breast-cancer.oncotypedx.com/en-US
My research did not uncover any side effect comparisons between 1 mg vs. 2.5 mg or femara. Ask your onc but even he/she would agree that the more chemo you undergo the more toxicity and the greater the side effects.
Please consider non-toxic therapies to help you reduce the risk of relapse.
http://www.peoplebeatingcancer.org/blogslash-breast-cancer-risk-slash-breast-cancer-risk-relapse/
The only cancer facility that I have experience with the the Fred Hutchinson Inst.in Seattle. I went there to learn about stem cell bone marrow transplants. Excellent organization but very conventional.
The issue boils down to what you think, your decision. More chemo may reduce the risk of relapse but increase the risk of side effects. Less chemo is slightly greater risk of relapse but greater risk of side effects.
Please consider the Oncotype DX test to help you decide and non-toxic therapies regardless of what you decide.
Let me know if you have any questions. Hang in there.
David Emerson
ReplyHi David,
I received a kidney from my wife in 2009, and presently have no issue with regard to my kidney. I just discovered that I have prostate cancer. PSA 9.3 Gleason 9 and stage T2. From my biospy, out of 12 samples, one has 2 X 1mm and another has 1 X 1mm plus another at 5mm. The other 12 samples are cleared. My radio oncologist recommends that I under go hormone therapy immediately. Perhaps followed by brachytherapy. Since hormone therapy is not a cure, and brachytherapy may cause some seeds to migrate to my transplanted kidney which may be damaged by them, not to mentioned all the side effects from the hormone therapy. What is your opinion if I do nothing now and just keep a close watch on my PSA until it rises significantly. Eventually I have to receive some form of treatments and accept all the side effects associated with any form of treatment. I am 73 years old, if I delay my treatment completely I should be able to add a couple more years to my life without any treatment and suffer any side effects from any treatment. Once I start treatment, and in view of my kidney transplant, and therefore may not be suitable for external nor internal radio therapy. Do you think it is wise for me to gain some a few more years free from any treatment and side effects. You opinion will be much appreciated.
Hi Lucas-
I am sorry to read of your prostate cancer diagnosis. As an aside, I like the fact that your wife gave you one of her kidneys. And you have no issue with it.
The main issue regarding your prostate cancer diagnosis, as I see it, comes down to how advanced your cancer is. The impression I get from reading your post is that you would like to avoid negative side effects. In my mind, this means that you put quality of life high on your list.
If this is the case, please be careful when considering adrogen deprovation therapy (ADT). Though ADT has been shown to slow the progress of prostate cancer, it does have a number of negative side effects associated with it.
For the sake of this reply I will assume that you understand the pros and cons of both ADT and brachytherapy.
Please read the post I recently researched and wrote about cryosurgery in prostate cancer.
http://www.peoplebeatingcancer.org/blogcryotherapy-prostate-cancer-ready-prime-time/
Based on my understanding of your stage, T2, your tumor is confined to the prostate and may be confined to one lobe?
The challenge you face when discussing the issue of cryosurgery with your onc is that if your onc does NOT provide this therapy then he may not endorse it for you. Based on my understanding of your post, cryosurgery of your PCa may be a good fit for you.
Let me know if you have any questions. Hang in there and good luck.
David Emerson
Ed. Note- another therapy for you to consider-
David
ReplyMy wife has been diagnosed with glioblastoma multiform Stage 4.
She had the tumor removed 3 week ago and is due for radiation and chemo therapy. We are aware of the risks involved in radiating the brain, but are willing to take the chances as it is the only conventional option to this kind of cancer. Although we reluctantly accepted radiation, chemo is a big problem for both of us, as it is not clear how it could be helpful. It depletes the immune system, which at the end of it all has to win the war with the cancer and if it does not, death is inevitable. Chemo is like a declaration of war with the enemy, blowing up foe and friend alike and hoping that kills the enemy only. Has a survivor of globlastoma opted for radiation without chemo? Any ideas on the issue will be appreciated!
Hi Alex,
I am sorry to read of your wife’s GBM stage 4 diagnosis. I agree with your comments about chemo though I include radiation therapy when talking about the brain. I will be direct.
Conventional oncology offers no curative therapies for GBM stage 4. Surgically removing the tumor is an excellent first step. My bias in cases such as yours is to place quality of life above all else. I will offer evidence-based research, with sources below for you to consider either as complementary to radiation or not.
Novocure device
http://www.peoplebeatingcancer.org/breakthrough-brain-cancer-therapy-novocares-treatment-for-glioblastoma-multiforme-gbm/
Cannabidiol-CBD-
http://jpet.aspetjournals.org/content/308/3/838.full
Curcumin- by itself or to enhance the efficacy of temozolomide chemo- I understand that you are against chemotherapy but consider low-dose chemo- less that the standard of care-
Curcumin sensitizes glioblastoma to temozolomide by simultaneously generating ROS and disrupting AKT/mTOR signaling.
http://www.ncbi.nlm.nih.gov/pubmed/25050915
Omega 3 (fish oil) either by itself or to enhance radiation?
http://www.ncbi.nlm.nih.gov/pubmed/21267532
Grape seed extract-
http://www.ncbi.nlm.nih.gov/pubmed/20673175
Alex, the five therapies linked above may manage your wife’s GBM as well as or better than radiation. Without the toxicity. Some ideas to consider.
Let me know if you have any questions.
hang in there
David Emerson
Alex-
I almost forgot. Please consider the capsule form of antineoplaston therapy-
http://burzynskipatientgroup.org/
David Emerson
ReplyMy dad was diagnosed with stage 4 lung cancer on Jan 20th. He is suppose to start chemo on Feb 13. I have also been looking into proton therapy and I changed his diet. He is eating only cancer fighting foods.
We did not get a second opinion. What can we expect from chemo. My dad is not sick, other than the 2 tumors in the soft tissue and the 1 on his lung.
ReplyHi Angie-
I am sorry to read of your dad’s stage 4 lung cancer diagnosis. I will try to answer your question about what to expect from chemo but if you would like info on diet and nutrition let me know.
If you would like more specific info on what to expect from chemo I will need the specific regimen that your onc is recommending. Please consider immunotherapy- this will require specific molecular testing by your onc on your dad’s specific lung cancer.
http://www.cancer.gov/clinicaltrials/results/summary/2012/PD-1-immunotherapy0612
If you dad undergoes “cytotoxic chemotherapy” meaning standard of care, statistically this therapy is not curative. Meaning the chances are that your dad will not make it for five years. Further, this chemo regimen is highly toxic and may cause dramatic side effects. I understand that you say that your dad is not sick and it may be difficult to wrap your brain around your dad’s prognosis. But please understand that conventional chemo, in this case, is not curative and is highly toxic.
http://www.ncbi.nlm.nih.gov/pubmed/17873174
If you would like information on integrative therapies, that is to say evidence-based supplementation that will enhance standard chemo while reducing chemo toxicity I can email you specifics. This would require working with your onc to reduce the dose given to your dad- either less chemo at one time or stretch the regimen out over a longer time. It is difficult to convince oncs to deviate from the standard of care. You will need to have a solid relationship with your onc.
It’s up to you. Let me know. Thanks
David Emerson
ReplyHello David:
I was diagnosed 5/13 with Stage I rectal cancer. Standard-of-Care is a permanent colostomy, which I declined.
I have tried many alternative therapies which I credit for the slow progression but I am now Stage II and need to find a solution.
My initial treatment included the ketogenic diet and Dr. Kelley enzyme protocol. Supplements include Hydroxycitrate, R-Lipoic Acid, B-17, Vit D complete (w/A&K), AHCC, Vit. B, Metformin, and Butyrate complex.
I am considering Iscador but the studies I have read indicate only success in QOL and maybe stabilization but not tumor shrinkage.
My last-chance therapy would be Chemoradiation/Chemo but I don’t want to wreck my immune system if there is another alternative therapy with promise for shrinking of adenocarcinoma rectal tumors.
Is there something else out there I should be trying?
Thanks.
Hi Pat-
I am sorry to read of your rectal cancer diagnosis though I am glad that you declined a permanent colostomy if your original diagnosis was stage 1. I will list possible therapies below for your consideration. I encourage you to continue your diet, enzyme protocol and supplementation regimen. I will link a post about anti-CRC supplementation-
Your primary challenge will be to consider adjuvant chemoradiation post surgery. I can’t tell from your post if you underwent surgery to remove the original tumor. If you are otherwise healthy the studies I’ve read reference surgery to remove the tumor. Surgery alone shouldn’t ruin your immune system as you say.
“In stage II CRC, there is tumor penetration through the bowel wall involving the serosa; however, there is no involvement of regional lymph nodes or distant metastases. While the overall survival in this subgroup of patients is approximately 70%–80% 5 years after surgery, in high-risk stage II disease, the clinical outcome is similar to that of patients with stage III disease. Currently, these high-risk patients are identified by tumors that not only penetrate the bowel wall but also show evidence of adhesion to or invasion of surrounding structures, free perforation, obstruction, or aneuploidy.”
http://theoncologist.alphamedpress.org/content/10/5/332.full
Whether you undergo surgery only or surgery plus chemoradiation please consider the supplements listed in the blog post linked below. Consider REDUCING the total dose of chemo while supplementing with the list below to both enhance your chemo will reducing the toxicity your immune system will benefit. Your onc will be extremely reluctant to give you less than the standard of care…
http://www.peoplebeatingcancer.org/blogcolorectal-cancer-supplementation/
Let me know if you have any questions. Hang in there.
David Emerson
ReplyHi.
I am 50 years old,been healthy and
have negative mammogram every
year,until july 2014 by my early
mammogram followed by ultrasound,and core biopsy .I diagnosed to invasive lobular carcinoma ,99% positive ER
negative PR
negative Her
Low ki-67
BRACA negative
I had chemo every 21 days for
5 times . I just had my double
Mastectomy on February 2015
one of the sentinel node size 2.2mm is positive but additional
6 lump nodes are negative .
Original cancer size was 2 cm
Mastectomy specimen size was 1.9 cm. now I have to have radiation.
My question is my cancer didn’t
Respond good to Chem that I got.
What that means I didn’t get no
benefits of that chemo ,what should
I do?
Thanks
Hi Nancy-
I would like to do more research on the many diagnostic issues you mention above but before I do I wanted to email my initial finding to you. I think you will like it, have a better weekend, etc. I will excerpt the info that I think is important and provide a link to the entire article at the bottom of the quotes.
“Poor Response To Chemotherapy Does Not Mean Poor Outcome For Patients With Rare Breast Cancer”
Women with a rare type of advanced breast cancer who do not benefit from primary (pre-surgical) chemotherapy still have been found to do better in the long run than patients with a more common advanced breast cancer who do respond to chemotherapy.
This is a striking finding, the first to find that in a type of breast cancer, response to chemotherapy seems to have little to do with long-term treatment success…
…”In fact, this study suggests women with invasive lobular carcinoma have a different kind of disease, and that they may benefit from a treatment that is more adequately tailored to the biology of their cancer.
In the end, our study indicates that primary chemotherapy, with its toxic effects, may not be the best standard of care for women with invasive lobular carcinoma,” Cristofanilli says. “Additional investigation, including genomic and proteomic studies, are warranted to help clarify the unique biological features of this disease.”
What they found was contrary to what they had anticipated. Women with invasive lobular carcinoma had a poorer response to primary chemotherapy yet better overall survival.
… five years after treatment, breast cancer had not come back in 80 percent of women with lobular carcinoma, compared with 66 percent of ductal carcinoma patients. And five-year survival in women with invasive lobular carcinoma was significantly higher – 91 percent – compared with 72 percent in women with invasive ductal carcinoma.
http://www.sciencedaily.com/releases/2005/01/050111163605.htm
To answer your question “What that means I didn’t get no benefits of that chemo ,what should I do?” The article above says that you MAY in fact, benefit from the chemo. May I ask what “stage” you were told when you were first diagnosed? Invasive Lobular Carcinoma, yes, but what stage, II or III?
Where are you being treated? What is the name of your hospital? I would like to do more research on your case.
thanks very much,
David Emerson
ReplyThanks David
Stage II (intermediate Nuclear Grade)
Chemo regime
Adrianycin
Cytoxan
Taxotere
Hi Nancy-
The Breast Cancer diagnostic testing you list compared to most PBC posting is extensive- thank you. Therefore please talk to your onc to confirm my findings below.
Also, Adriamycin (anthracycline) chemotherapy damages your heart and kidneys. I know because I had adriamycin and developed chronic a-fib. Please consider coq10 supplementation.
Coenzyme q10 for prevention of anthracycline-induced cardiotoxicity.
http://www.ncbi.nlm.nih.gov/pubmed/15911925
Effect of Coenzyme-Q10 on Doxorubicin-Induced Nephrotoxicity in Rats
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3533995/
To further recommend non-conventional breast cancer therapies, please read the post below and adopt these evidence-based therapies to greatly reduce your risk of breast cancer relapse.
http://www.peoplebeatingcancer.org/blogslash-breast-cancer-risk-slash-breast-cancer-risk-relapse/
First, as my previous reply stated, the lack of response to the pre-adjuvant chemo doesn’t mean poor outcome for your diagnosis.
Secondly, based on the specifics of your tumor size and single lymph node involvement, according to the link below you are stage IIB.
Stage IIB describes invasive breast cancer in which:
“the tumor is larger than 2 centimeters but no larger than 5 centimeters; small groups of breast cancer cells — larger than 0.2 millimeter but not larger than 2 millimeters — are found in the lymph nodes OR
the tumor is larger than 2 centimeters but no larger than 5 centimeters; cancer has spread to 1 to 3 axillary lymph nodes or to lymph nodes near the breastbone (found during a sentinel node biopsy) OR
the tumor is larger than 5 centimeters but has not spread to the axillary lymph nodes”
http://www.breastcancer.org/symptoms/diagnosis/staging
Third, when you write “positive ER” if you mean positive estrogen receptor, I think that your onc may encourage endocrine therapy.
“Endocrine therapy for breast cancer involves selective estrogen receptor modulators (SERMS), such as tamoxifen, which behave as ER antagonists in breast tissue, or aromatase inhibitors, such as anastrozole. ER status is used to determine sensitivity of breast cancer lesions to tamoxifen and aromatase inhibitors.[27”
“Cancer
Estrogen receptors are over-expressed in around 70% of breast cancer cases, referred to as “ER-positive”, and can be demonstrated in such tissues using immunohistochemistry…”
http://en.wikipedia.org/wiki/Estrogen_recepto
Well, this is another long, involved email. Let me know if you have any questions.
David Emerson
ReplyI recently had prostate cancer surgery and now, 3 months later, my first PSA test shows 1.58, so I assume cancer is still present. I’m schedule to see the doctor in 3 weeks. Do you have any recommendations. I am 65.
ReplyHi Larry,
This is going to be a long email so please read this when you can concentrate. Further, if you have any questions please ask.
Please keep in mind that I am not a professional- just a long term cancer survivor who has learned a lot over the years. While I think your assumption may be correct,(your prostate cancer has metastasized) I do have therapies for you to consider- therapies that I believe will both slow any residual prostate cancer as well as enhance your quality of life if your onc recommends androgen deprivation therapy (ADP).
First, situation linked below-
Artificial Prostate-Specific Antigen Persistence After Radical Prostatectomy
“The serum half-life of PSA, after removal of all prostatic tissue, is 2 to 3 days. Therefore, PSA levels can be expected to decrease below the detectable limit within 4 to 6 weeks after RP.3 PSA persistence at a significant level beyond this point is usually a strong indicator for disseminated prostate cancer. This is not an uncommon clinical scenario, especially in high-risk disease, and it often leads to immediate additional treatment for the respective patient.4”
http://www.jco.ascopubs.org/content/30/5/e62.full
Please give serious consideration to this article. Bone strengthening therapy is not standard of care this early in the process. However if you take ADT your bones will weaken.
This link doesn’t paint a pretty picture of ADT but I hope to show you integrative therapies to moderate the negative side effects.
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3747499/
Larry, if it is okay with you I would like to take a day or two to research therapies to manage your libido, your heart, muscles, etc.- all of the negative side effects of ADT- I hope to find supplementation to enhance the effectiveness of ADT in hopes of you being able to REDUCE the standard dose and reduce the negative side effects.
Please reply to the above to tell me what you are thinking- Thanks
David Emerson
ReplyHi David
my husband has leiomyosarcoma (pelvic is primary site and is only there ) in pelvic ,size 14.9×10.8×17.3 before radiation and ,post radiation treatment size increased by about 5 cm now is 16.4×13.3×22.9.
the mass is so big that is pressure on bladder ,rectum ,sacrum ,sciatic nerve there is loss of fat plane .also mass does abut the common and external iliac vessels bilaterally with loss of intervening fat plane between structures .they do,however ,continue to demonstrate normal flow .When we spoke to surgeon oncologist she said that his tumor is low grade 2,she was going to do surgery post radiation but now is impossible because tumor is bigger .She mention that there is risk of bleeding because big iliac vessels.
There will be only chemo and more radiation tx left for him. His doctor is oncology surgeon and his case was discussed with sarcoma doctors group.My husband since diagnosed in August 2014 had and have sciatic nerve pain,foot drop ,had some numbness but got better post radiation ,circulation in leg is OK ,has difficulties to walk and i see is making him weaker with walking ,he lost some weight ,before radiation in November 2014 he had colonostomy surgery done ,now he slightly loose weight and gets back .He really looking for miracle we have 2 children he wants to be for them.I ask for second opinion last Friday .Do you think if any vascular surgeon will do surgery does he has chance …….thank you Ania
Hi Ania-
Thank you for answering all my questions. I’m sure that you have been getting experienced support from your surgical onc with the input of the sarcoma doctor. I am not qualified to say anything about a vascular surgeon. In addition to working with these doctors I will say that you should consider Budwig, Gerson and PolyMVA (see the link below). Your options are limited so I would be casting a wide net. Hang in there and good luck.
http://polymvasurvivors.org/soft-tissue-sarcoma.html
David Emerson
ReplyMy husband was diagnosed with pelvic leiomyosarcoma in August 2014,went for 25 days of radiation therapy ,Doctor was planning to do surgery after tumor will shrink post radiation treatment ,but tumor didn’t shrink ,just got slightly bigger.We are left with no more treatment for now maybe more radiation and chemo later .Please any advice to shrink tumor .What you know about HYDROGEN PEROXIDE AND BAKING SODA ,I have hear that people have good result with those .Any other advice please and thanks
Ania
Hi Ania-
I am sorry to learn of your husband’s cancer diagnosis. While I can include info about possible therapies I can offer much more specific information for you if you can tell me your husband’s
1) Stage at diagnosis-
2) type and size of the tumor-
3) is your oncologist a “sarcoma oncologist?” Does he/she see at least 100 sarcoma patients annually? If a specialist is not in your area you can consult with on on the phone. He/she may be able to offer therapy ideas-
4) is the leiomyosarcoma the primary or secondary site? In other words, did the LMS come from a cancer elsewhere?
5) finally, how old is your husband and generally what health is he in?
As for you question about hydrogen peroxide and baking soda, I couldn’t find anything about HP and LMS. I did find general info about LMS and the Budwig Protocol however-
Also, there is some info from leiomyosarcoma survivors and the Gerson diet-
If you can relay answers to the questions I ask above I will do more research and email the results. Thanks and hang in there.
David Emerson
All the questions and answers may have an impact on your husband’s therapy and prognosis.
ReplyHi David,
I’ve been diagnosed with prostate cancer. PSA is 7 now, slowly gained from PSA 2 over a
few years since I’ve moved into my 60 years old status, currently 68.
My biopsy was 3+3 and the oncologist said I was at the low stage. A recent MRI shows no
cancer tumors anywhere, same for the digital exam. Urination is average flow.
I take 4 grams of apricot seed, ground fine daily. Also the same amount of sulfur crystals.
What is your opinion?
Thanks,
Kimo
Hi Kimo-
I am sorry to read of your prostate cancer diagnosis though when this cancer is diagnosed in an early stage such as yours, the prognosis is excellent. I am asked about early stage prostate cancer frequently so I have completed a fair amount of current research on your situation. In general my research has found many articles and studies reporting that early stage prostate cancer is over-treated. The treatment almost always results in short, long term side effects. Therefore my opinion would be to pursue the non-toxic therapies below in addition to keeping a close watch on your situation.
I will numerate the therapies for you to consider below.
1) Apricot seeds- apricot or B17 is controversial. There is enough anecdotal evidence to support what you are doing.
2) Likewise organic sulfur-
3) Please read this Reuters article citing a study by Dr. Dean Ornish about early stage prostate cancer patients-
http://www.reuters.com/article/2008/06/17/us-genes-lifestyle-refile-idUSTON70483420080617
4) Add to the healthy lifestyle discussed above the following anti-oxidant supplements with evidence-based research to support anti-prostate cancer action.
curcumin-
http://www.ncbi.nlm.nih.gov/pubmed?term=curcumin%20and%20prostate%20cancer
green tea extract-
http://www.ncbi.nlm.nih.gov/pubmed/?term=green+tea%2C++prostate+cancer
vitamin D3=
http://www.ncbi.nlm.nih.gov/pubmed/?term=vitamin+d%2C+prostate+cancer
grape seed extract-
https://search.yahoo.com/yhs/search?p=prostate+cancer%2C+grape+seed+extract&ei=UTF-8&hspart=mozilla&hsimp=yhs-001
resveritrol
https://search.yahoo.com/yhs/search;_ylt=A0LEVinKb8lUUS8AnaAnnIlQ?p=prostate+cancer+resveratrol&fr2=sb-top&hspart=mozilla&hsimp=yhs-001
Kimo- if you combine the lifestyle therapies studied by Dr. Ornish and consider curcumin, green tea extract, vitamin D3, grape seed extract and resveritrol (all can be purchased through Amazon.com) I think you will be able to manage your prostate cancer without the need for toxic therapies.
Let me know if you have any questions. Thanks and hang in there.
David Emerson
Hi: I’ve been diagnosed with stage 4 lung cancer that has also spread to my living. Both the radiologists and oncologists have told me there is nothing they can do. Can’t go on chemo because of bad kidneys. Anyway was reading about hemp oil and mistletoe extract as possibly being able to help stop the growth of the cancan. Have you heard of this?
ReplyHi Wendy-
I am sorry to read of your lung cancer diagnosis. I agree that conventional oncology has no curative therapy for you (you don’t want to go on chemotherapy). However conventional oncology had no curative therapy for me either… in 1997, and here we are.
I don’t mean to sound negative about conventional medicine. I am only saying that there is much more to cancer health than conventional oncology.
Yes, I have heard of cannabidiol (C-B-D) and mistletoe as cancer therapies. Both are non-conventional and more difficult to find info about- info such as efficacy, dosing, etc.
http://www.ncbi.nlm.nih.gov/pubmed/22198381
http://www.ncbi.nlm.nih.gov/pubmed/?term=mistletoe+and+lung+cancer
This is a little off topic but I am in the process of taking a homeopathic remedy for a blood clot in my leg and the remedy is working very well so I thought I would pass the below info on to you…if you want the name of an excellent homeopathic dr. let me know.
http://www.ncbi.nlm.nih.gov/pubmed/2559483
As for where to get cannabidiol, I have no experience here. If it were me I would go to the internet and search for C-B-D oil. Same thing for sourcing mistletoe. As I mentioned above, I can refer you to a homeopathic doctor.
As for your lung cancer spreading to your liver, my approach would be to pursue those non-conventional cancer therapies that you are looking into and believe that the metastasized cancer (liver spots) is managed at the same time.
Wendy, you situation is complicated- please let me know if you have any other questions or concerns.
Thanks
David Emerson
Hello dear,
My mother in law is diagnosed with liver cancer. Now the city scan shows that she has the cancer in multiple places and at this point in time the doctor told us that there is nothing they can do except telling us to take her home and have some quality time with her. The size of the cancer range from 7 to 12cm.since these doctors are not giving us any hope, what’s your advice on this? and what do you think about giving her delta 9 THC cannabis? I appreciate your help.
Elias
ReplyHi Elias-
I am sorry to read of your M-I-L’s metastatic liver cancer. While your oncologist’s advice may seem harsh, it is important for you, your wife and your MIL to understand that there is nothing that conventional oncology can offer you. Toxic chemotherapy and radiation will only make your MIL feel awful.
At this point I would suggest a range of immune boosting therapies combined with a spectrum of evidence-based anti-liver cancer therapies that are non-toxic. Nutrition, supplementation, lifestyle and mind-body therapies are what I do for my own incurable cancer (not liver cancer).
Elias, I am both a cancer survivor and cancer coach. I do not tout miracle cancer cures. I work with cancer patients to learn about and undergo evidence-based therapies.
If you are interested I am happy to provide specific examples for you and your MIL to learn about and consider.
Let me know, thanks.
David Emerson
Cancer Coach
Hi David,
Thanks for the response. Yes I am interested if there is something you can offer. The whole family is so desperate to try anything that can help her. BTW what do you think about the cannabis?
Thanks
Elias
good evening, just returned from an appt. was told Liver biopsy came back positive. Have a 2.4cm x 1.9cm tumor on my liver. My initial diagnosis was for stage 2 pancreatic cancer last may. Ca19-9 tests showed no real cause for alarm. Readings were from 112 to 157. In dec. the test came back at 1665. At that time the doc said to have a ct scan, which showed the tumor on the liver. Was told today there are no available treatments to take care of the problem. My kidneys are in stage 3 failure and have shown to be steady for the past 1 1/2 years, I also have diabetes and other issues. I am not happy the way the doctor told me the prognosis but I am not going to accept the end result of his. I am wondering if there is any other treatments I can have to try to make the tumor become smaller or if you know of someone or something I can research for this problem. Thank you for your help
ReplyHi Sandy-
I am sorry to read of your cancer diagnoses. But you seem to have an excellent attitude so you are ahead of the game as far as I am concerned. By themselves, pancreatic cancer, liver cancer, kidney failure, and diabetes, I would be able to offer possible therapies. Taken all together, I believe I would suggest one therapy that might aggravate another health issue.
In other words, the cryotherapy/cryosurgery that I would offer to freeze off the tumor on your liver might cause problems elsewhere. The Whipple surgery I would suggest to reduce the tumor burden of your pancreatic cancer might present other problems.
I hate to admit it but your situation is over my head. If it were me all I could think of to do would be to see a naturopath to pursue a liver and kidney flush and combine this with other nutritional therapies. It is possible that there are homeopathic remedies for you to consider as well.
I am sorry that I can’t offer more concrete ideas. Please let me know if you have any questions.
thanks and hang in there.
David Emerson
Replygreetings,
i have been diagnosed with glioblastoma multiforme stage 4. approximately 70 percent of tumour was removed on jan 3 and i am waiting now for assessment and subsequent treatment.
i look forward to hearing from anyone that has a similar condition
thanks
andre
Andre-
I am sorry to read of your GBM stage 4 diagnosis. While I communicate with other GBM patients such as yourself I have no current ongoing relationships with GBM patients as of today.
Two ideas. One, if you are interested, I can email info about non-conventional evidence-based therapies (or info about therapies that are “integrative” meaning they enhance conventional therapies) and two, I can run an ad on Facebook that will attract other GBM stage 4 patients.
I am offering to run the FB ad/blog post, only because PeopleBeatingCancer happens to be spending this week testing how to use social media to facilitate our cancer coaching patients requests.
If you are interested I am offering to run a small Facebook campaign paid for by PBC. No charge to you. Let me know.
Thanks and hang in there,
David Emerson
ReplyI have been diagnosed with prostate cancer. Gleason score of 3/3, psa of 5.3, and 2 of 26 biopsy sites showing cancer cells (in area where my urologist detected some abnormality during rectal exam). I am considering pencil-beam proton therapy. What is your opinion of this procedure?
ReplyHi Terry-
I am sorry to read of your prostate cancer diagnosis. Did your urologist stage your cancer? An accurate stage is needed to think through your therapy options. Based on your post I’m guessing that your prostate cancer is stage 2.
To be clear, I am not a medical doctor, I am a long term cancer survivor- I have learned a great deal over the years but I cannot give you a medical opinion.
Having said this I will give you my opinion based on evidence-based research.
Your Gleason score, psa and biopsy results all sound to me as though your cancer is low-risk. While pencil-beam radiation is lower risk than many other prostate cancer therapies, there are side-effects. Knowing this I would take time to practice non-toxic therapies all the while keeping a close watch on your prostate, and see how you progress.
Those non-toxic prostate cancer therapies I allude to are linked below. Please read and consider each.
Terry- while this study is small, it sounds as though is applies directly to you.
http://www.reuters.com/article/2008/06/17/us-genes-lifestyle-refile-idUSTON70483420080617
In addition to the lifestyle changes listed in the above article, also consider supplementation such as curcumin, green tea extract, resveritrol, and grape seed extract-
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3521661/
http://www.cancer.gov/newscenter/newsfromnci/2007/prostategrapemuscadine
Let me know if you have any questions. Thanks
David Emerson
ReplyHi David, I’m a 37 year-old female (mother of 3) living in Canada, and was diagnosed with a thyroid tumor in September (4 months ago). Since then, I had a biopsy with no results (inconclusive results), so I was asked by my endocrinologist if I want a second biopsy or the surgery. He never explained to me the risks or consequences of any of my options, but I did some online research, and I opted for the surgery. At this point however, I wonder if I have any chances to see an oncologist or have a blood test to see if there are any cancer cells in my body without an actual cancer diagnosis (but having the risk of it because of the 3cm tumor on my thyroid gland). I have my next appointment booked with my family physician for next week to seek second opinion, but I wonder if that (referral to another endocrinologist, or to an oncologist, or just to a blood test) is smtg I can expect. I am not familiar with the referral process, and I am so frustrated so far of not getting answers, while hearing from every angle that the best chance of treating/curing cancer is when it’s recognized early. Thank you for being here and helping us!
ReplyHi Thyroid patient-
Without a conclusive biopsy or stage I am limited in how much research and info I can provide you.
I will list some pertinent issues and then try to outline your options. Keep in mind that most or all of my research is based on studies in and of Americans not Canadians.
1) The chance that your tumor is cancerous is remote. “Most often the first symptom of thyroid cancer is a nodule in the thyroid region of the neck.[3] However, many adults have small nodules in their thyroids, but typically under 5% of these nodules are found to be cancerous”
2) The 5 year survival rate for thyroid cancer is very high “Five year survival rates are 97.8% in the United States.[2]”
http://en.wikipedia.org/wiki/Thyroid_cancer
The feeling I get from your post is that you want to put your mind at ease by finding out one way or the other, if your thyroid tumor has metastasized/is cancerous.
Detection of metastases
Detection of any metastases of thyroid cancer can be performed with a full body scintigraphy using iodine-131.[18][19]
Here is info about blood tests for thyroid cancer-
I can’t speak to the referral process in Canada. Sorry. We Americans understand that the Canadian medical system is free and wonderful at solving many health issues but not so good at complicated problems such as cancer.
Let me know if this info helps. Let me know if you have any other questions.
thanks
David Emerson
ReplyThank you very much for your quick and thorough answer. It helped me understanding my situation better, and I was able to express my concerns to my family doc today clearly. Yes, my biggest concern is if it metastasized, or if this is actually already a secondary (I’m not sure of the medical term) cancer. So my doctor explained that right now I only have one symptom (thyroid tumor), so we have to focus on that, remove it, and after the surgery, they’ll be able to tell if it was cancerous or not. If it’s cancerous, I’ll probably have the full body scintigraphy that you mentioned above after the surgery. She asked me about other symptoms, like headache, coughing blood, or loosing weight as signs of other cancer. I don’t have these right now, so I’m hoping for the best. But what I have is tinnitus (sometimes my hearing is like I’m under water on either or both ears) and some purple bruises that are healing very slowly and I mentioned these to her, but she was not concerned. What do you think? I realize, I’m not a diagnosed cancer patient, so I don’t want to waste your time, and I also really appreciate your care and attention so far. Just one more question: Do you think the anti-cancer therapies (baking soda, katogenic diet, vitamin B-17, etc.) should work against benign tumors as well? Or are those cells work that much differently that they react totally differently (or don’t react at all) to these therapies? Thank you and all the best.
ReplyHi Klara-
First and foremost, you are not wasting my time. Asking me questions or asking your family doc questions are never wasting time. To put it another way, it is your responsibility to yourself and your friends and family to keep an eye on your health.
Now, to address your questions. Your doctor is correct in saying that you have a growth in your thyroid as many of us do. Only five percent of these growths in one’s thyroid will spread or are “malignant.” Having a different cancer would be a “secondary” cancer.
If you are not comfortable with the researched “average” of 5% chance of your thyroid growth spreading, then yes, remove the growth and examine the growth. If your dr. tells you that your growth is not “malignant” then you probably do not need to have further testing done. But if you want to put your mind further at ease, then yes, have more testing.
As for tinnitus, it can be causes by many things. The link below will give you more info on how you may be able to deal with it.
http://tinnitus.net/tinnitus-causes.php
If you experience not other symptoms then you are doing well. If you asked your doc. about tinnitus and bruising and she was not concerned then again, you are doing well.
As for the other therapies you asked about, yes, in general therapies such as nutrition and supplements do reduce one’s risks of cancer, any cancer. I take a number of supplements daily, eat lots of fruits and veggies, exercise moderately, all in an effort to remain cancer free. It is less about you thinking or acting about a benign thyroid tumor and more about living a reduced-risk lifestyle.
I hope this helps. Thanks.
David Emerson
ReplyI am a 66 year old female who was recently diagnosed with DCIS I had a surgical biopsy and about 2.5 inches of micro calcification was removed. I”m going in for surgery again because the surgeon wants to remove cells around the margin. If the margin is positive she recommends a mastectomy, if not I believe it’s only radiation therapy. Since it is a non invasive cancer I was wondering does this seem like the right treatment for me and would it be worth it to get a second opinion a this point? Thanks.
ReplyDear Newly dx’ed DCIS-
First and foremost, yes, get a second opinion. You need an onc to closely look at your DCIS to determine your risks of relapse, which I will do my best to relay below. I will try to address your questions one at a time.
1) Two issues here- “If the margin is positive she recommends a mastectomy, if not I believe it’s only radiation therapy.” First, there is a test to determine early BC risk of relapse called oncotype dx (http://breast-cancer.oncotypedx.com/en-US). This test is expensive and you must make sure your insurance covers it. I bring the test up mainly because I get many questions from early stage BC patients asking about the need for lumpectomy, mastectomy, local radiation, chemo and the risk of relapse.
2) regarding radiation therapy- Let me first go on record as saying that you DO NOT fit the description of “elderly patient.” At 66 you are 4 years younger than the article describes as elderly. I’m simply giving you information on which to base your decisions.
Radiation Does Not Improve Survival in Elderly Early-Stage Breast Cancer Patients
http://www.medscape.com/viewarticle/722500
3) Only you can decide on the extent of your therapies now and the risk of relapse. I hope the articles linked below will help.
Slash breast cancer risk, slash breast cancer risk of relapse?
http://www.peoplebeatingcancer.org/blogslash-breast-cancer-risk-slash-breast-cancer-risk-relapse/
Compilation of DCIS questions and answers-
Let me know if you have any other questions- I hope this helps- hang in there and good luck-
David Emerson
ReplyHi David I was trying to use the links you provided, do you know it seems to be blocked, even if you try copying and pasting it into the web browser. I am in the midst of deciding on whether to take radiation and tamoxifen which has terrible side effects after a lumpectomy. Oncotype 15% and taking tamoxifen for 5 years reduced to 9%. Radiation Oncologist explains chance of recurrence without any treatment is 21.7%, with radiation is 6.4% to the breast area only, and with tamoxifen its 4.7% recurrence to the body. Kindly advise.
ReplyHi Sholoy-
I am sorry to read of your BC diagnosis. To clarify your situation, what stage were you at diagnosis? Have you had an Oncotype test of your BC? I understand that local radiation and/or tamoxifen or another aromatase inhibitor will reduce your risk of relapse but you are correct these therapies cause side effects and increase the risk of secondary cancer.
The advice you request will be based on two things. First, your stage at your original BC diagnosis (DCIS, 1, 2?). Secondly, evidence-based, non-conventional therapies that can reduce your risk of BC relapse such as anti-BC nutrition, supplementation, bone health, lifestyle and mind-body therapies. Let me know and I will offer input.
Thanks
David Emerson
P.S.- I will fix the broken links if you tell me where they are- what blog post the are in-
ReplyHI David, I am 68 years old and was diagnosed with colan cancer July 21/14. The tumour was removed with no problem. Then a cat scan showed spots on the liver plus an MRI. I have had 6 rounds of chemo and they have shrunk by more than 50%. I have also been taking aloe vera juice 3 shot glasses a day. At first with chemo I had mouth sores, baking soda didn’t work, 24 hours after the aloe sores were gone.
Now they want to do resection of the liver, remove the complete right side and remove the 2 spots on the left or burn them and then have 6 more chemo. This liver surgery is massive and I am very susceptible to infection. I have been reading about milk thistle
I am very terrified of surgery. David what do you recommend?
Thanks in advance for your opinion
Bryan & Sheila
Hi Bryan and Sheila-
When you were first diagnosed with colon cancer, what was your stage? Surgical removal of the tumor is often the first step. I am researching different methods of removing the colon cancer mets to your liver. When you say “burn them” are you referring to cryotherapy? Yes, milk thistle promotes liver health but your onc clearly believes that he/she must remove all colon cancer tumors- ASAP.
You say that you are terrified of surgery yet you underwent your initial colon surgery with a positive outcome. Doing nothing has risks but undergoing more surgery also has risks. How do you feel about this risk/reward? What was your stage at diagnosis?
Let me know, thanks- David
Cryotherapy for liver metastases- http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0056683/
ReplyWe are from Canada. My brother was diagnosed of colon cancer, had colon resection June 2014, 13 sessions of Chemo, stopped chemo in December 2014. When the tumors shrunk his surgeon decided that he’s now illegible for liver resection. On February 9, 2015 65% of his liver removed. He had liver failure right after the surgery, was unconscious for 3 days while he was transferred to the Acute Care centre trying to keep him a life. Miraculously he wake up and was hospitalized for 2 weeks. His bilirubin went up to 398 mmol/L . He did frequent visits to the hospital due to liver function sysmptoms and problems. September 22, 2015 shows the bilirubin went down to 40 mmol/L. His liver function keeps improving. He currently has an external bile duct drainage bag. He had unsuccessful several attempts to open the bile duct blockage. He has to live forever with the bag hanging from his bile duct. The doctor said his duct is too small and can’t be repaired unless he goes for another surgery. But this is impossible before he gains his health back which may take another couple of years.
On June, 2015 CT scan shows a suspicious spot in his liver and one in the lymph node. Last CT Scan September 15, 2015 shows the cancer is progressing, the report shows 4 tumors in the liver, and the tumors sizes are bigger in the lymph nodes. There is no treatment for him at this stage.
His surgeon finally admitted that he has done a mistake when he decided to remove part of his liver. In addition to the fact that he removed too much of the liver, his liver was already damaged from the Chemo, that’s why he had liver failure. The bottom line is, if cancer metastasised to the lymph node and other organ, any kind of surgery would not do well. Once you operate and cut your skin open, the tumors will spread like crazy.
What would I do if I go back to the day we knew I he had colon cancer?
If the cancer metastasized to the lymph nodes DO NOT go for any surgery! I have been searching around all day every day, talked to many cancer scientists (I work with cancer scientists) and consulted many doctors, I’ve been reading and searching for more than a year, collected piles of research documents. The result is not to do any surgeries. The best option in this stage is to go for Immunotherapy and oncolytic virus treatments.
Immunotherapy success stories for aggressive cancer. In Canada there was an experiment done on a patient in Princess Margaret Hospital. When we asked his oncologist if he’s illegible for this trial, he told us unfortunately he is not illegible because he does not have the “mismatch repair mutation”. Most of colon cancer patient stage 3 and 4 has this problem.
Oncolytic virus treatment is basically a combination of two virus injected to patients, one to kill the cancer cell, the other to increase the immune system and prevent the cancer from coming back. There are experimental trials right now.
September 22, 2015 his oncologist has given up on him. The tumors will spread to other organs, bones, lung, brain etc. He has no treatment for him. He asked us to prepare him for Palliative Care to manager his symptoms once they hit.
I gave him couple of trials to look at for Virus vaccine, he seemed to be not aware of them. He promised to refer him to the doctor who is conducting the trial in Mount Sinai Hospital. This trials are available in different countries https://clinicaltrials.gov/ct2/show/NCT02285816?term=oncolytic+viruses&cntry1=NA%3ACA&rank=6
You can also check the Immunotherapy: https://clinicaltrials.gov/ct2/show/study/NCT02060188?term=CheckMate+142&rank=1&show_locs=Y#locn
Hi LS-
I am sorry to read of your brothers health challenges but he is fortunate to have you doing research for him. Is there anything that you are asking me? You know more about your brother’s situation at this point.
Let me know.
David Emerson
ReplyMy husband has the same situation. He got tumor removed from his colon last week and ct scan showed two spot on his liver. Docs wants chemo till the the tumors get smoler so then cut the liver. We have not dedicated what to do next. He has not get chemotherapy yet. I am trying to boost his immunology system with natural product, he feels good. I hope this works. Thank you for sharing.
ReplyHi Elisana-
I am sorry to learn of your husband’s metastatic colon cancer. The chemotherapy regimen (s) that your husband will undergo (if he does) will be very toxic. And the toxicity is necessary to kill colon cancer cells and shrink the tumors on his liver. However I encourage you to consider non-toxic therapies to integrate with his chemotherapy regimens. They synergy will enhance the efficacy of his chemo while moderating the toxicity of the chemotherapy. Further, I encourage your husband to include evidence-based anti-colon cancer supplementation.
For example, curcumin has been shown to kill colon cancer while it enhances certain chemotherapy regimens.
Chemotherapeutic potential of curcumin for colorectal cancer.
I am both a cancer survivor and cancer coach. I can research and provide you with research and specific recommendations that I mention above. Let me know if you would like to learn more about cancer coaching.
David Emerson
ReplyI am a 63 year old male who was diagnosed with prostate cancer 2 years ago. the oncologists recomment surgery to remove prostate, or radiation or both as needed. not recommended is seed therapy.
i have seen my brother in law go along with his doctors and he died within two years of being diagnosed with a cancer of the blood.
My homeopathic doctor in mexico, has just received his license to practice medicine here in the usa and recommends following the oncologists advice.
I don’t plan on following their advice. i prefer to die without all of the pain and suffering i have seen friends and relatives go through with surgery, surgery problems, radiation, more readiation, and chemotherapy that never ends until you are dead.
I am taking ;
1. 1 nature made muliti vitamin for him
2. 4 IP6 & INOSITOL daily
3. 375 mg CuraMed with BCM-95 (ie. Curcumin)
4. 400 mg EGCg (green tea extract)
5. 200 mcg of Selenium
6. 5 mg of Biotin
7. 8 drops of cellfood in water
8. 200mg of organic fresh squeezed lemon juice and 1 teaspoon of baking soda in a glass distilled water
My oncologist wants to have a MRI done on my prostate.
My question: Is there anything else that might be recommended to fight this prostate cancer. I was originally diagnosed with a gleason score of (3+3) two years ago. My gleason score last year was (4+3). My PSA throuhout has been hovering around 3. Any comments are welcome.
Alan
ReplyHi Alan-
I am sorry to read of your prostate cancer diagnosis and I understand your basic disagreement with conventional oncology. I live with a great deal of collateral damage from aggressive conventional therapies that I underwent. Therapies that did nothing for my cancer.
However, it is not simply yes or no to conventional oncology. Take one issue at a time. Below I will discuss your original pc diagnosis, further diagnostic testing and your integrative therapies.
First, regarding your diagnosis two years ago. While your Gleason and PSA scores are getting up there and should not be taken lightly, I agree with you that you do not need to be too aggressive at this point. What sort of symptoms are you currently living with? If any?
PSA “hovering around 3” does not have to mean therapy at this point. How long have you been taking the list of supplements above? Meaning, do your numbers, PSA and Gleason, reflect any time taking the supplements? Will your insurance cover your MRI?
Alan, if you choose to focus on lifestyle and supplements to manage your PCa, it is a good idea to get diagnostic checks as often as possible. If your numbers remained stable then you can make a good case for avoiding conventional therapies- therapies which will bring negative side effects.
Regarding your supplement list. Please click the link below to read a blog post I wrote about a study conducted by Dr. Dean Ornish. It seems to me that you exhibit the symptoms of one of the “30 low risk prostate cancer patients.” By dedicating your life to what is mentioned in the article, diet, daily moderate exercise (6 times weekly) you stand to change your prostate cancer’s genetic expression and to manage your PCa. Again, please keep a close eye, diagnostically speaking, on your prostate.
Curcumin, green tea extract, less red meat, lots of fruits and veggies, regular testing, Alan, you are pursuing therapies. Lots of then. Just not conventional therapies.
Let me know if this makes sense. Let me know if you have any questions.
Hang in there.
David Emerson
ReplyBeing a Chiropractor I fully realize that it is not my field. Yet when my sister in laws’ father had the same problem he decided to try “Herbal Prostate Complex” from Herbal Care Direct. His PSA is now normal. His daughter is an MD. Problem. I’ve tried ordering the same product for other friends and it seems that the company is out of business.If you can research this company. Find them. Let me know. Ihave no personal or professional connections to this company. Thanks. Mark Baerwaldt
ReplyHi Mark-
I appreciate your comments. However I could not find any evidence-based info or research on HPC. Further, the company you refer to to purchase HPC is listed as a scam investment.
http://www.complaintsboard.com/complaints/herbal-care-direct-regina-saskatchewan-c578545.html
ReplyI was recently dx’d with stage 4 breast cancer. bummer right? I am in the medical field (non clinical but around enough medical care to know to do my own research as well as taking into account the expert’s advice). In addition to all of the main stream supplements, I came across this webpage today. It is a different spin than the main stream. I still have to cross check their info but it looks promising as an adjunct source of natural therapy. Good luck to all!
ReplyDear s davis-
I am sorry to read of your breast cancer diagnosis. Please let me know if there is anything PBC can do for you.
thanks
David Emerson
Replyhi i have serious problem prostate cancer spreading is it some other way cure or direction to beat this cancer
thank you J.B.
ReplyHi J.B.-
I am sorry to read of your prostate cancer diagnosis. I need more information in order to provide info.
1) What stage of prostate cancer is your diagnosis?
2) What other diagnostic tests have you undergone? PSA, Gleason score?
3) Have you had a core biopsy? If so, what are the results?
A diagnosis of prostate cancer can mean many different things. The more information the more info I can provide you.
Let me know.
David Emerson
ReplyAlan-
I’m just checking in to see how you are doing. Also, here is a therapy for you to consider-
David Emerson
Replyhave you tried chamomile tea and dandelion roots crush up with some soil left on 1 tablespoon of the dandelion root per day until you start getting heart burn then that’s when your body tells you enough for now,then keep drinking the chamomile tea,it might just work you never know until you try it..god bless
ReplyYes I had colon cancer an now a cell went to mylung. There is a drug ahcc.this has a lot of good results. I just started this.this will open your eyes
ReplyHi Margarit-
Maybe I can help. What drug are you referring to?
David Emerson
ReplyHi ALan,
You can never tell anyone what to do and I’m not trying to. I’ll just give my opinion. My Father was diagnosed with prostate cancer 12 years ago with a Gleason score of 10+10 (the worst you can have). His oncologists recommended medical castration (by taking drugs) followed by radiation. They did not recommend surgery in his case. He has been stable for all these years with VERY minimal side effects even though his cancer was aggressive and they caught it just in the nick of time. If he had waited he would almost certainly have faced a far more serious path and could eaily have died.
I advise you to get a second opinion and if they agree, to seriously condider following their advice and treatment. Blood cancer is COMPLETELY different from prostate cancer so it is hard to compare them. By taking matters into your own hands, you could easily end up suffering when you don’t have to because your cancer os probably manageable with the right treatments. Think about that.
Good luck,
Greg
ReplyI have Prostate cancer and I was on Hormone Therapy I got Hot flesh for many years but I have to go to Bath-room during night very often
ReplyHi Zygfryd-
I’m not sure what you are asking. Please clarify your question. Thank you. David
I have testicular cancer pure siminoma
Left Testical was removed I have a recurance lymph node next to my kidney has cancer I have no tumor markers though I had a stint out in my kidney to drain it I told to do 3 cycles of platinum chemo what should I do
Raymond-
Please read my reply to your first email. Thanks.
David
ReplyDear David I have Myelodysplastic syndrome _refractory anemia with ringed sideroblast.I have blood transfusion every second week but my hemoglobin is very low like 5,6
Thank you David
Hi Zygfryd-
I am sorry to read of your myelodysplastic syndrome. Do you have a question?
David Emerson
ReplyHI Bob-
I am sorry to read of your penile cancer. I can offer you information about therapies, both conventional and non-conventional as well as cancer centers (hospitals), or other info if you are interested. If you would like more info, please ask specific questions and give me your stage at diagnosis and basic info about yourself such as age, general health, etc.
Let me know. Thanks and hang in there.
David Emerson
ReplyI have a recurance from teticular cancer left test removed tumor I have is next to my left kidney no tumor markers I’ve been told to so cycles of plat chemo it’s pure siminoma what should i do
ReplyHi Raymond-
I am sorry to read of your testicular cancer. I need some background first.
1) When were you first diagnosed with testicular cancer? What was your stage at diagnosis?
2) What therapy did you first undergo when you were first diagnosed? Only surgery? Chemotherapy?
3) You currently have a stent in your left kidney to drain it periodically?
4) You have relapsed? How was your relapse diagnosed or discovered?
Let me know, thanks.
David Emerson
Cancer Survivor, Cancer Coach
Dear David,
My husband 76 years old had a Whipple procedure a year ago, followed by Gemzar chemotherapy with terrible side effects.Now the cancer is back in the bed of the surgery. He also had stomach cancer in 2010, and renal cancer (one kidney removed) in 2012.
We still want to win this beast.
Any suggestions will be much appreciated
ReplyHi Sofia-
I am sorry to learn of your husband’s relapsed pancreatic cancer. With his history of previous cancers as well as his age please consider
evidence-based integrative therapies (see example below) as well as evidence-based anti-pancreatic cancer nutrition, supplementation, lifestyle and mind-body therapies based on the pathways linked below.
When you say “back in the bed of the surgery” are you saying that your husband will undergo surgery again to remove his pancreatic tumor? Gemzar is the marketing name of gemcitabine. There are several supplements that research shows can integrate with conventional chemotherapy regimens.
Curcumin and gemcitabine in patients with advanced pancreatic cancer.
Let me know if you have any questions.
David Emerson
ReplyHi Scott-
I am sorry to learn of your stage 3 squamous cell carcinoma. In order for you to decide if I can help you I need to understand your situation more thoroughly. Are you saying that you have been diagnosed with non-small cell lung cancer, squamous cell, stage 3?
If so, is your NSCLC stage 3A or 3B? I need to understand your situation to be able to offer information about the non-toxic therapies that you are asking about.
Let me know, thanks and hang in there,
David Emerson
ReplyI think the cure for cancer might be sugar. It would give all cells the chance to fight back cancer with the energy given by massive amounts of sugar. Plus if the cancer had the sugar it probably wouldn’t fight the body’s cells because it has all the energy it needs to survive.
ReplyHi Rob-
You are correct. Sugar feeds cancer. Deprive cancer of sugar and it dies. The challenge with “sugar feeds cancer” is that sugar is in almost all foods- glucose, fructose, sucrose, fruits, veggies, etc.
I am a cancer survivor who tries to consume as little sugar, in all its forms, as possible. I am good enough to remain in CR but I can’t quit all sugars all the time. thanks
David Emerson
Reply