Leave a Comment:
160 comments
[…] To Learn More About Overtreatment in Cancer Care- click now […]
Reply[…] To Learn More About Overtreatment in Cancer Care- click now […]
Reply[…] To Learn More About Overtreatment in Cancer Care- click now […]
Reply[…] To Learn More About Overtreatment in Cancer Care- click now […]
ReplyI am 73. I have had a polyp for 5-6 years completely symptomless and staying the same size. I changed gynaecologist and this one wants to remove it. I really am unsure what to do
ReplyHi Patricia,
While I’m reluctant (and not qualified) to tell you what to do about treating/not treating your polyp, I can cite the study from the article and tell you what other women coming to this site have said.
When you say your polyp is “symptomless and staying the same size” you are in the 41.7% from the study. Clearly, you are in the majority.
Further, my guess is that you would not be asking me or your doctor about the polyp if you weren’t concerned somewhat about your polyp.
1) Please talk to your doctor about the pros and cons of removing your polyp. There are side effects and risks to surgery or other therapies.
2) Ask your doctor why she wants to remove your polyp. This questioning might sound silly but my point is that your doctor should be able to convince you of the need to undergo therapy and take on the risks, to remove your polyp.
If your doctor can’t convince you to remove your polyp, in other words, if, based on the past 5-6 years living with the polyp, not causing any problems, you can’t agree to undergo the pain, cost, etc. in exchange for whatever the positive reasons are for removing the polyp, then why would you want to remove it?
I have done lots of therapies in my past, related to my cancer, based on my doctor telling me to do something. No reason, just “this is what I think you should do.” I now ask my doctor for more specific reasoning for undergoing therapies.
And you may decide to have your polyp removed. But your doctor owes you a thorough explaination, thorough reasoning.
Let me know if you have any questions.
David Emerson
Results of these examinations showed that
in 41 (13.7%) of these women, the polyp had naturally resolved;
in 125 (41.7%), there was no change in polyp size;
in 61 (20.3%), there was a decrease of at least 1 mm;
in 49 (16.3%), there was an increase of greater than 50% of the originally measured polyp diameter;
in 24 (8.0%), there was a greater than 50% increase in polyp diameter.”
[…] Are Endometrial Polyps Overtreated? […]
ReplyI have been diagnosed with a polyp of 1 CM X .7cm X .7 cm, 2 fibroids outside my uterus that are large, and one medium inside my uterus lining. I have pain and very long periods close together. Last period lasted 43 days and it started again about 2 weeks after last one ended. I had a biopsy a year ago and now my doctor wants to do a D&C, uterine ablation and remove the polyp and fibroid from inside my uterus. Should I be getting a biopsy again before procedure and do you think I need the uterine ablation. I am 53 years old and have not missed a period yet. I am seeing my doctor again in 2 weeks to go over treatment plan and pre-surgical appointment.
ReplyHi Regina-
I am a cancer coach. I am not qualified to respond to your situation. I am sorry I can’t be more help.
David Emerson
ReplyI had a recent Misscarriage on 08/11/2017.Then I needed to do two D&Cs and one round of Medical Abortion.It still shows some products inside.To make sure we have decided to undergo hysteroscopy on 02/01/2018.Before that doctor has given me number of tests including Sugar tolerance.I am giving all the lab results along with USG findings.
TSH: THYROID STIMULATING HORMONE – SERUM- 2.75 µIU/mL
BETA-HCG:QUANTITATIVE – SERUM/PLASMA- 1.1 mIU/mL
PROTHROMBIN TIME – 12 secs
ACTIVATED PARTIAL THROMBOPLASTIN TIME – Test 30 secs, Control-27 secs
HBsAg – NEGATIVE
LUPUS ANTICOAGULANT STUDY – Lupus Anticoagulant not detected
GLUCOSE -SERUM / PLASMA (FASTING)-91 mg/dL
CBC-Packed cell volume(Calculated)-39 %
ESR(Automated – Westergren method) -60 mm/hr
Eosinophils- 4 %
WBC Count(Optical/Impedance) -6.78 10³/mm³
Platelet Count(Optical/Impedance)- 110 10³/mm³
Hemoglobin(Optical/Impedance)-12.1 gm%
Neutrophils- 44 %
Lymphocytes-47 %
Monocytes-5 %
GLUCOSE – SERUM / PLASMA (2 HR POST GLUCOSE)-78 mg/dL
GLUCOSE – SERUM / PLASMA (1HR)-107 mg/dL
URINE GLUCOSE(FASTING) -Nil
URINE GLUCOSE(1HR)-Nil
URINE ROUTINE (CUE):
Colour-Straw
pH-6
Urobilinogen -Normal E.U./dL
Pus Cells-6-8 /h.p.f
Specific Gravity-1.020
Epithelial Cells-4-6 /h.p.f
Protein-Nil
Ketone-Nil
Transparency-Slightly Turbid
Bile Salts-Nil
Bile Pigments-Nil
URINE GLUCOSE(2 HR)-Nil
ANTI CARDIOLIPIN ANTIBODY IgG – SERUM (ELISA)-4.1 GPL U/mL
ANTI CARDIOLIPIN ANTIBODY IgM – SERUM-4.2 MPL U/mL
USG finding-
Apollo Chennai-Uterus Anteverted
Normal Appearing Uterus with homogenous myometrial Echoes
APD Echoes 3.7cms
Endometrium measures 6mm (Triple Line)
Echogenic material measuring 2.1*1.2 seen in the lower end of cavity.
Impression-Retained product of Gestation lower end of cavity
USG findings of CMC Vellore(Not got a physical report)
They given Polyp 19mm and SOL 10mm seen in uterus.(Totally confused how found it)
Bleeding is having on and off.Now having no Bleed since 3days.
No pain since 2 weeks.
I went under a Hysteroscopy today.They told that they got something like Polyp but note sure.To make sure they have sent it for a biopsy.Will get the result on 08/01/2027.When I asked them it could be a rpoc they said it can be.Beacause I never ever had any Vaginal discharge issue .Moreover I did a routine USG in the 9th month of 2017 there it showed nothing, absolute empty uterus.How can a Polyp devolps right after misscarriage.I got no connection.
ReplyHi Tanaya-
I am a cancer survivor and cancer coach. I posted the study about overtreatment to educate about the low risk of polyps being cancerous according to the research. I am not qualified to address any of the issues outlined in your post to me.
I apologize for not being more help to you. Good luck.
David Emerson
Cancer Survivor
Cancer Coach
Director PeopleBeatingCancer
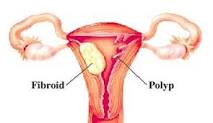
I think this is a highly uneducated post and while you state you are no expert it’s unwise to give out links in commemts about fibroids when you are talking about polyps. They are not the same thing and are made of completely different tissue. Fibroids are not a risk factor for cancer and have different treatment both natural and surgical. Polyps do have a cancer risk and different advice applies.
ReplyHi Meg-
While I appreciate your input I’m not sure I understand what you are saying. The study that is discussed focuses on polyps. Both of the links are for polyps. I can’t even find the work “fibroid” on the page. I wrote a different post about uterine fibroids. Those are two different posts. I don’t “give out” comments. Readers write the comments.
David Emerson
ReplyFibroids are not the same thing as polyps. They are two different things.
ReplyHi Pashta- thank you very much for your observation.
David Emerson
ReplyFibroid Treatment Without Surgical procedure (NATURAL & SAFE)
There’s nothing worse than bleeding closely between or during your durations which
embrace blood clots , having pains in your pelvis and or decrease again.
This fibroid healing plan accommodates listing of foods, herbs and workout routines that I adopted
for exactly four months. If you’re unlucky enough to have
extreme fibroid ache or if the fibroids are inflicting
serious problems then surgery or embolization is the one possibility.
This methodology of therapy has confirmed
effective at shrinking fibroids or destroying them fully, nevertheless,
it isn’t with out side effects. For all procedures besides hysterectomy, seedlings — tiny tumors that your doctor does not detect during surgery — might ultimately
grow and trigger symptoms that warrant therapy.
Fibroids could grow slowly as a single tiny lump or as a cluster, fluctuate in size from 1 mm
to greater than 20 cm (8 inches) in diameter or
more. Myomectom: the place just the fibroids are taken off
with out removing wholesome tissue of the uterus.
Conventional Ayurveda concept says that herbs are most effective after a person completes an inner cleaning program.
Nonetheless, this method of uterine fibroid elimination is
one of the best of the two surgical procedure choices for those girls that are
still desirous to conceive a baby.
Treatment with medicines called gonadotropin-releasing hormone analogues (GnRH analogues) can lower your oestrogen ranges, which
usually shrinks fibroids. Research reveals there’s a relationship between diet and developing uterine fibroids.
This procedure could also be an option if the fibroids are contained contained in the uterus (submucosal).
ReplyHi,
I am 30 years old and have recently been diagnosed with an endometrial polyp (1 x 0.8 x 0.5 cm), after inter-menstrual bleeding. My doctor has advised me to not remove it surgical at this stage, but check every six-months to monitor its size. She also mentioned that it would not interfere with my pregnancy. I am planning for pregnancy soon, and would like to know if there are any reported natural/dietary measures to stagnate or retard the growth of the polyp?
Thanks
ReplyHi Akig-
I agree with your doctor. I have excerpted the study that you read to support my thinking. If you monitor your polyp you should be able to keep an eye on if the polyps resolves, stays the same, shrinks, or grows.
To summarize: If you are diagnosed with endometrial polyps:
1) 13.7% of the time the polyps resolve on their own-
2) 41.7% of the time the polyp size stays the same-
3) 20.3% of the time the polyps shrinks at least 1mm-
4) 16.3% + 8.0% of the time the polyps grow at least 50% larger
David Emerson
ReplyHi there,
I had a question regarding endometrial polyps.
I have recently been diagnosed with 2 polyps (11mm and 8mm) which really surprised me as I don’t have symptoms and probably wouldn’t have noticed if I hadn’t done a routine ultrasound.
I am now incredibly worried about this – my Dr has said that it’s up to me whether or not I remove them since I don’t have any symptoms. I am really worried about them affecting my fertility as I do want to try to conceive fairly soon. Please help!! What are the chances that they will interfere or affect my chances of getting pregnant? Are there any other risks associated?
Hi Lina-
I am sorry to read of your unexpected endo polyp diagnosis. I get this kind of question frequently. I am a long-term cancer survivor and cancer coach. I blogged about the study that you read to highlight polyp “over treatment.” In short, according to the study discussed in the blog post, only 2.5% of polyps are malignant (lead to cancer).
Having said that I fully understand that “watching and waiting” is difficult for people. I am not fully experienced but I believe that “D & C” to remove the polyps is painful and can cause side effects. Further, I understand that simply surgically removing a polyp does not prevent the polyp from growing back.
I am not qualified to speak about fertility issues. I can offer the types of evidence-based, non-conventional, non-toxic therapies that increase the chances of endometrial polyps shrinking and disappearing. But this is as far as my experience goes.
One more thing. You mentioned that you are not experiencing any symptoms. Pain and bleeding appear to be the most common symptoms of endo polyps. You are doing well NOT to be experiencing any symptoms plus this fact reduces your risks of malignancy. See the excerpt below.
Re your questions:
1) “What are the chances that they (polyps) will interfere or affect my chances of getting pregnant?”
Pregnancy rates after hysteroscopic polypectomy depending on the size or number of the polyps.
“Hysteroscopic polypectomy of endometrial polyps appeared to improve fertility and increase pregnancy rates in previous infertile women with no other reason to explain their infertility, irrespective of the size or number of the polyps. Type of infertility of patients seems not to affect fertility rates after hysteroscopic polypectomy. Menstrual pattern was normalized in the majority of patients after hysteroscopic polypectomy. In addition, hysteroscopic polypectomy is a safe procedure with low complication rate.”
2) “Are there any other risks associated? (with polyps)”
Not sure what you are asking. The risks are associated with removing or not removing. D & C is bad, hysteroscopy is okay according to the study. Depending on when you are trying to get pregnant, consider non-toxic therapies to try to shrink and remove the polyps and then have a hysteroscopy polypectomy if they don’t resolve with non-toxic therapies.
Hang in there,
David Emerson
What Happens When You Watch and Wait?
From January to July of 2010, Dr. Hartman examined 300 women who had been diagnosed with endometrial polyps in the previous 2 to 43 months.
Results of these examinations showed that in 41 (13.7%) of these women, the polyp had naturally resolved; in 125 (41.7%), there was no change in polyp size; in 61 (20.3%), there was a decrease of at least 1 mm; in 49 (16.3%), there was an increase of greater than 50% of the originally measured polyp diameter; and in 24 (8.0%), there was a greater than 50% increase in polyp diameter.”
“Malignant polyps represented 2.5% of the total sample. Postmenopausal bleeding and age greater than 60 years were the only factors that remained associated with a higher risk of malignancy with a prevalence ratio of 3.67 (95% CI, 1.69–7.97) and 1.5 (95% CI, 1.01–1.09), respectively…”
To summarize: If you are diagnosed with endometrial polyps:
1) 13.7% of the time the polyps resolve on their own-
2) 41.7% of the time the polyp size stays the same-
3) 20.3% of the time the polyps shrinks at least 1mm-
4) 16.3% + 8.0% of the time the polyps grow at least 50% larger
ReplyHi Doctor,
I was recently diagnosed with 3 polyps in my uterus and I was wondering what is your suggestion on whether to wait and see, or treat?
For your reference, I am 27 and looking to start a family in the next year or so — so I would like to know the full risks/benefits to surgically removing the polyps (on chances of fertility and/or pregnancy process) OR not treating it & trying to conceive.
Please let me know if you can respond to me via email?
Thank you!
May
Hi May-
I am a cancer survivor and cancer coach. I posted the study to discuss the potential of cancer and endo. polyps. I am not qualified to answer your question.
Good luck.
David Emerson
ReplyHi m infertility and I did hysterescopy a findings are (n)cx and (n) vagina so what does this mean
ReplyHi Lucia-
I am a cancer survivor and cancer coach. I am not qualified to answer your question “what does this mean?”
David Emerson
ReplyI have been diagnosed with an endometrial polyp. I am interested in the antioxidant supplementation that you recommended in your comments above and am curious if you feel that overtreated polyps can actually promote future problems and even cancer in the endometrium?
ReplyHi Becky-
I am sorry to read of your endometrial polyp. Regarding your comments, I am not qualified to comment on over treatment. My role is that of a cancer coach curating information to provide someone like you. The studies provided provide therapies beyond conventional treatment.
David Emerson
ReplyI am 52 years old and never had any trouble with my cycle until August. That is when is bled so bad for 44 days. Dr in er said possible cancer, but just got biopsy of my uterus back. No cancer but do have pollyps. Am taking med roxy progesterone to stop bleeding and bentyl for cramping. Cramping occurs all the time bleeding or not. Also having blood pressure issues, it is running 147/98 127/92. My blood pressure has always been very low, like 85/55. I also have floating tissue in the uterus. Are the pollyps a concern?
ReplyHi Ginger-
I apologize for the slow reply. I am a cancer coach and have limited knowledge about your issue. I posted the study to address the possibility of cancer caused by polyps. The study states that “Malignant polyps represented 2.5% of the total sample” meaning 2.5% of polyps where cancerous. I do think you have other health issue to discuss with your doctor but your polyps shouldn’t be a concern according to the study excerpt below.
“Malignant polyps represented 2.5% of the total sample. Postmenopausal bleeding and age greater than 60 years were the only factors that remained associated with a higher risk of malignancy with a prevalence ratio of 3.67 (95% CI, 1.69–7.97) and 1.5 (95% CI, 1.01–1.09), respectively…”
To summarize: If you are diagnosed with endometrial polyps:
1) 13.7% of the time the polyps resolve on their own-
2) 41.7% of the time the polyp size stays the same-
3) 20.3% of the time the polyps shrinks at least 1mm-
4) 16.3% + 8.0% of the time the polyps grow at least 50% larger
David Emerson
Replyi david
I was diagnosed with endometrial polyp measuring 1cm through transvaginal us I’m schudled for hysteroscopy and removal of the polyp this Friday because I’m scared it might be cancer.but deep inside I’m feeling like I’m rushing,because 3 months ago I did an ultrasound for different issue that didn’t show anything can a polyp grow in 3 months or the us missed it ( by the way I saw the doctor because I was having spotting between period 2 times in 5 months).do you think surgery is the right thing to do in my case.I’m 41 .
HI Nathalie-
I am sorry to read of your endo polyps. I am a cancer coach specializing in blood cancers. I am sorry I can’t be more help
to you.
David Emerson
ReplyHi david just a reply I had my polyp biopsy and d and c report and everything was b9.but the doctor did mention that the polyps may return.I heard from reading some French speaking forum that it exist in Germany a clinic where two german doctors and a Chinese professor treat polyps using herbs and plants and most of the women who went there had their large polyps reduced in size and the small one just disappeared. Do you have any ideas what these plants-herbs might be. Thank you David for what you are doing it was very interesting reading your article and all the women experiences while waiting for the results.
ReplyI would love to know about the herbs and plants you refer to. I have read that progesterone can help and foods that help promote progesterone or process estrogen may help. flaxseed is supposed to be good and staying low on estrogen may help ( ie avoid dairy, and anyother animal products like eggs or meats the might have high estrogen)
ReplyHi David,
I’m 32 and going through infertility challenges. Both my husband and I are completely healthy, no issues. I was about to start IUI and the dr did a SHG and saw a polyp or fibroid on my uterus about 8mm. He’s recommending I get it removed before moving forward. I want to get a 2nd opinion but don’t even know where to start .. And advice on this would be helpful… Thank you!
ReplyHi Maria-
I am a cancer coach. I have no training or education with fertility issues. The post you read is there for those concerned about the risk of malignant polyps. I am sorry I cannot be more help.
David Emerson
ReplyI’m 56 years old and until about 36 months ago I had regular menstrual cycles, but had endometrial lining started thickening. My GYN ordered and ultrasound, everything was normal. A year later he did another ultrasound, everything was normal. Last year he did an ultrasound and my endometrium had thickened to about 10 mm. He ordered a biopsy, everything normal. 3 month later a second biopsy, everything normal again. Meanwhile, about 24 months ago my cycles were every 8-12 weeks, then in Jan. of 2015 (at the time my GYN was starting the biopsies) I had what I thought was my last period and I was now postmenopausal. Until 51 weeks later, I had another period. My GYN did another ultrasound (all were transvaginal, as well as abdominal) and found my endometrium had thickened to 17mm with a 1.1 x 0.7 x 1.4 cm polyp. Although the radiologist said everything looks benign, my GYN wants to do a complete hysterectomy. I’m in no pain and the bleeding is confined to what appears to be normal menstrual cycles. Is this over kill? Is removing the polyp only a good first step while waiting for biopsy results?
ReplyHi Michelle-
First and foremost, I am a cancer survivor and cancer coach. I posted that article and study in order to address the issue of polyps. As you say, your radiologist said that “everything looks fine” and that you are getting a pathology report to confirm that your polyp is benign.
I will say that your instinct, that a complete hysterectomy at this stage, is overkill. While I am no expert I have researched the issue of hysterectomy enough to know that there are side effects related to this procedure.
There is a small chance that your polyp is malignant-2.5%. There is a good chance that the polyp will not return. I agree with you that “Is removing the polyp only a good first step while waiting for biopsy results?” I do not see any harm in waiting while there is potential harm in having a complete hysterectomy.
Take it easy and good luck.
David Emerson
Cancer Coach
HI I got my Ultra sound done today.
The finding says uterus with 9 mm thick endometrium.
A soft echoic poypoidal lesion of 15*15*8mms size in the endometrial canal at the fundus.
Small anechoic cyst one in each ovary , Adnexae within normal limits.
I got the check up by gynic , she suggested me medicined and a course for 21 for getting regular menstural cycle.
IS it a matter of real concern?
Hi Shreya-
I am a cancer coach. I am not qualified to answer your situation. I am sorry I can’t be more help.
David Emerson
ReplyHi
I have had a cancerous endometrial polyp removed.
The uterus was thickened significantly
now the uterine thickening has resolved some 8 weeks later after being on a major naturopathic / integrative health protocol
i avoided hysterectomy because i was so afraid of the outcome and while i am open to removal of the uterus, i was not wanting my ovaries removed
I just had another ultrasound result come through that says that the endometrium appears normal, there is still a adenomyoma looking mass of the same size as the polyp was in width, length and height but only 1ml in volume. No endometrial margin invasion or myometrial invasion is seen like in the first scan.
What do you think
I would like to think it has resolved after the polyp was excised.
Thank you so much for looking at this for me
Ali
ReplyHi Ali-
I am a cancer coach. As such I am not qualified to try to answer your questions. You appear to have learned a lot about your situation. I would continue to consult both with your gyn. and naturopath.
thanks and hang in there,
David Emerson
ReplyDavid,
Are biopsies are part of the over treatment? I am 43, regular periods, some spotting in-between, lost weight without trying, etc. Doctor found a polyp via ultrasound and wants to do biopsy. My thought is to do nothing but monitor it, afraid that the biopsy might make it worse. Can biopsy spread a malignancy? Apologize if this is a silly question, mind racing a bit about this.
ReplyHi Pat-
If your question “are biopsies part of over treatment” no, the study you read is not referring to biopsies as over treatment. The article linked below discusses the risk of biopsing an endometrial polyp.
Your health situation, 43, regular periods, some spotting, etc. supports your thinking to monitor your polyp. According to the study the risk of a cancerous polyp is 2.5%.
While there is little evidence that a biopsy might make a polyp “worse,” there are risks. See below.
As the study explains, polyps usually stay the same or shrink. I would add those evidence based lifestyle and nutritional therapies to help shrink your polyp.
Let me know if you have any questions. Thanks.
David Emerson
“Endometrial Biopsy”
“Risks
There is a small chance that the cervix or uterus could be punctured during the biopsy. Bleeding or a pelvic infection is also possible.
Hello David. My name is Natalya (35years old).I was diognosed PCOS since 1999 in Russia. After years of my treatment I was prescribed Clomifene to induce ovulation but I didn’t take it because my family moved to USA.
Last year I started to take care of myself to get pregnant. My practitioner put me on Spironolacton,vitamins. For this time I am taking Metformin (1500mg), Progesterone (200mg),vitamins.
My last ultrasound(1/28/16) was on 18th day of my cycle:
There is well defined, echogenic,ovoid mass within the endometrial cavity strongly suspicious for endometrial polyp 8x5x9mm.
Both ovaries are still enlarged with small follicles 1-3mm. There no dominant follicle.
My questions:
Before taking the Progesterone I had no any terrible cramps during my period but cycle before my last one I had. That cycle I took Progesterone(200mg at night)for 20 days before starting bleeding.Does the Progesterone prolonged my cycle and started abnormal growing of endometrium? Usually my period is 24-28. With first taking of Progesterone my cycle was 40days. On my second Pr. taking,my cycle was 25 days.Now is 16 th day of my cycle. Should I continue to take Progesterone if I was diognosed with polyp?
I will be referred to Seattle Reproductive Clinic for further evaluation of polyp and fertility treatment. Before to go to the clinic I will be consulted with certified herbalist in Russia concerning PCOS and fertility.Do you know is it possible to clear off the polyp naturally?
Thank you for any suggestions I will recieve.
ReplyHi Natalya-
I am a cancer coach. I am not qualified to give you any advice about endometrial polyps. I wish I could be more help.
Thanks and good luck.
David Emerson
ReplyA 8 *11 mm echogenic nodule is seen in fundal endometrial cavity. Can it reduces the chances of conception
ReplyHi Ria-
I am not a gyn. or obstatrition. I am a cancer coach so please take the info below with a grain of salt. According to the Mayo Clinic study linked and excerpted below, yes, uterine polyps are associated with infertility.
Complications
By Mayo Clinic Staff
Uterine polyps might be associated with infertility. If you have uterine polyps and you’re unable to have children, removal of the polyps might allow you to become pregnant, but the data are inconclusive.
Let me know if you have any more questions.
David Emerson
ReplyI am post menopause and on Oct 2 had some bleeding. Doctor did US and said I have endometrial that was probably cancer and referred me to OB/GYN. she did exam and said I had a polyp which she couldn’t get out in the office. She did a pap and samples of the polyp and uterine wall and sent for biopsy. Everything came back benign. She scheduled out patient surgery for hysteroscopy and D&C and removed polyp. She said she never saw one that big and filled the uterine cavity. It was sent for further biopsy and came back benign. I bleed lightly for a week after the procedure then stopped. It has been one month since biopsy and I had a little light bleeding one time yesterday. Is it normal to have some bleeding again? Could stress cause it? My husband has been very sick and I have been very worried about it. Would that cause it?
Thank you
Shirley
Hi Shirley-
While I am sorry to learn of your endo polyp I am glad to read that you have taken the proper steps to 1) diagnose 2) treat (D&C) and then get a pathology report that should put your mind at ease. Meaning your polyp is benign.
I am not an OB/GYN so I can’t say officially that you shouldn’t have any bleeding at all one month after removing your polyp but I have to think that the “C” in D&C was substantial so it might take you awhile to heal completely. Certainly you should follow up with the physician who did your D&C to allay any anxiety you might have.
If you are interested there are antioxidant supplements that studies say reduce the risk of polyps returning. Let me know if you want more info.
In the meantime, take it easy.
thanks
David Emerson
ReplyHi David,
I have been busy dealing with some health issues that my husband has and just now had a chance to read your post. I would be very interested in knowing which antioxidant supplements reduce the risk of polyps returning. I have read that vitamin D and Curcummin help. If that is so would the turmeric with curcummin work as well? Thank you for your help.
Shirley
ReplyAbout a year and a half ago a fertility Dr. found a 14mm (the nurse did the math and decided that was the average size) polyp. He said he would remove it as it may hinder my fertility. We decided to adopt. When we spoke he said, “if you were not attempting to get pregnant” I would probably do nothing with the polyp. So I left it. I have a friend who a year later said that her Dr. removed her because there is a risk of it developing into cancer or that it could be cancerous. I am concerned. I freaked out! I told by OBGYN about the polyp and she acted like it was no big deal. While I am overweight, I am pre-meno and asympotomatic. Help!
ReplyHi Jennifer-
I understand that most people “freak out” when they think of cancer. However, in your case I will present the odds (from the article that you came in on) and you can draw your own conclusions.
The study found that only 2.5% of polyps are cancerous. Further, I will quote the findings of the study as to what may happen to polyps- resolve, shrink, etc.
Keep in mind that the overall issue discussed in the blog post was if endo polyps were overtreated. Your Dr. and your OBGYN recommended not to treat.
If you are interested, there are antioxidant supplements such as green tea extract that studies have shown to shrink endo polyps. Or if you want to you can have another check-up to see if your polyp is still there, resolved, shrunk, grown, etc.
To sum, I agree with the thinking of both your original Dr. and your obgyn. However, I can provide you with more information if you are interested.
Let me know. Hang in there,
David Emerson
“To summarize: If you are diagnosed with endometrial polyps:
1) 13.7% of the time the polyps resolve on their own-
2) 41.7% of the time the polyp size stays the same-
3) 20.3% of the time the polyps shrinks at least 1mm-
4) 16.3% + 8.0% of the time the polyps grow at least 50% larger”
ReplyPlease help I’ve had a bladder sling and pelvic mesh d&c and a ablation about 3years ago. I’ve had no pain cramping periods nothing until about 4months ago. I had and ultrasound done both cervical and regular. Doctor found cyst on my ovaries and polyps on my uterus. I also had my tubes burnt 5 years ago I’m now bleeding with clots and in some pain that just don’t seem to go away with my pain meds. I’m at a loss on what to do gynecologist can’t see me until the 16th witch is 8 days from now I left a message on my family doctors voicemail I’m waiting on a call but the more I read online the more I’m concerned should I got to ER should I call doctors tell whoever answers the phone I have an emergency? I hate hospitals they just put a bandaid on and tell you to follow up with doctor. Any advice would be greatly appreciated.
ReplyHi Lacie-
I am sorry to learn of your health difficulties. For the record, I don’t like hospitals either. In answer to your questions please understand that I am not qualified to recommend an ER visit versus an appointment to your OBGYN or family doctor. Certainly you need to see one of these medical professionals though from here, without knowing your history I can’t make the call.
Please let me know if you have any questions. I am sorry that I can provide more help and support.
David Emerson
ReplyI read through a bunch of the conversation here and haven’t found my specific situation addressed: 52 years old, blood tests show hormone levels “consistent with menopause” (high fsh, low estrogen), periods have not stopped–they’ve become irregular, some longer, some heavier, some shorter, some lighter, sometimes as little as 3 weeks apart, sometimes I’ll skip 3 cycles, then have an extra-long period. These periods, no matter when or how they show up, are accompanied by “hormonal” symptoms including sore breasts, migraines, mood shifts. 10-pound weight gain in past year (from 115 to 125), all around waist. Ultrasound showed probably endometrial polyp. Doc recommends hysteroscopy/D&C removal, but can’t be sure whether this polyp is 1) actually what this little thing is, 2) actually causing symptoms, or 3) new or something that’s been there since my previous ultrasound, which was 17 years ago late in a pregnancy. Doc cannot answer my primary question, which is: Is irregular bleeding caused by perimenopause or by (what might be) a polyp? I believe her intentions are good–she wants to rule out anything more sinister and the way to do that is to send me down this expensive diagnostic path (I have a high deductible insurance plan, so I will pay every penny of this out of pocket). I’m not over 60. I’m not pre-menopausal. I am not post-menopausal. It seems that nothing during perimenopause can be ruled out or ruled in without expensive diagnostics, and that none of the statistics quite apply to the perimenopausal woman. Last year, I had a breast biopsy under similar circumstances–thankful afterward to be pronounced cancer-free, but dismayed by the expense and the stress and the resulting scars and loss of sensation, and the general sense of “you should just be grateful.” Not eager to go that road again but don’t want to foolishly ignore something that might be problematic. Anyone, any insight to share?
ReplyHi Anne-
While I am sorry to read of your situation I have to say that you have thought through your indicators, options, etc. very well. I can’t offer any thinking that your doctor cannot offer. My only contribution is to add the experience of those women who have contributed to the blog post that you read.
D&C can be painful and can lead to side effects. If you or your doctor don’t know the result of this procedure it is difficult to promote the cost and problems that may occur as a result.(I too have a high-deductible health insurance plan) The risk of malignancy from a polyp is quite low and yes, it is frustrating if you are peri-menopausal and don’t fit the studies statistics.
The only therapy that I can offer is those antioxidant supplements that studies have shown shrink endometrial polyps- curcumin, green tea extract and vitamin D3. Regular consumption of these supplements have the benefit of reducing the risk of a host of cancers. I have taken each for years. If you are interested I can send the studies citing the anti polyp action and links to what I take.
I understand and agree with your comments about breast cancer biopsies. Yes, a case can be made for testing but a stronger case, in my humble opinion, can also be made for over-diagnosis and over-treatment. But that’s another blog post.
I am sorry I couldn’t offer more information.
Let me know if you have any questions. Thanks and hang in there.
David Emerson
1) “Doc recommends hysteroscopy/D&C removal, but can’t be sure whether this polyp is 1) actually what this little thing is, 2) actually causing symptoms, or 3) new or something that’s been there since my previous ultrasound…”
2) …send me down this expensive diagnostic path (I have a high deductible insurance plan, so I will pay every penny of this out of pocket).”
3) “I’m not pre-menopausal. I am not post-menopausal. It seems that nothing during perimenopause can be ruled out or ruled in without expensive diagnostics, and that none of the statistics quite apply to the perimenopausal woman.”
4) “thankful afterward to be pronounced cancer-free, but dismayed by the expense and the stress and the resulting scars and loss of sensation, and the general sense of “you should just be grateful.””
Your question “Not eager to go that road again but don’t want to foolishly ignore something that might be problematic. Anyone, any insight to share?”
ReplyI can relate as a 54 year old who had similar perimenopausal bleeding situation but have had no bleeding since October. my probable polyp, diagnosed feb 2021 is large (2cm). I canceled a couple of surgeries opting instead for “watch and wait” for now. I will do a 3rd ultrasound in 3 months. dr. says if all good can do another in 9 months. but I may opt for surgery in 3 months if anything is questionable. surgery is hard on the body and I’d like to avoid but the waiting is stressful.
ReplyPMB. 59years . Had a tv us and a uterine biopsy. Came back negative for cancer but thinks bleeding caused from polyp. Having a D and C. Chances of a malignancy if biopsy of uterine tissue negative or does that not have any relevance ? Scared out of my mind!
ReplyHi Sarah-
I’m not quite sure of everything you are saying in your cancer coaching email so I will have to make a few assumptions based on what I think you are saying…
1) your biopsy was negative for cancer
2) but your Dr. thinks that your bleeding may be caused by a uterine polyp?
3) You will undergo D and C procedure to remove the polyp?
4) I’m not sure about this one- you say that you have already had a biopsy that came back negative yet you are wondering if your uterine tissue can be be malignant? A negative biopsy means that you do not have cancer. My understanding of your email is that your biopsy is negative which means you to NOT have cancer.
But I will excerpt the study you were reading to try to put your mind at ease. A chance of any uterine polyp being malignant is 2.5%. Since you experienced some postmenopausal bleeding your risk increases to %3.67 but this is still a very low risk.
“”Malignant polyps represented 2.5% of the total sample. Postmenopausal bleeding and age greater than 60 years were the only factors that remained associated with a higher risk of malignancy with a prevalence ratio of 3.67 (95% CI, 1.69–7.97) and 1.5 (95% CI, 1.01–1.09), respectively…”
To summarize: If you are diagnosed with endometrial polyps:
1) 13.7% of the time the polyps resolve on their own-
2) 41.7% of the time the polyp size stays the same-”
3) 20.3% of the time the polyps shrinks at least 1mm-
4) 16.3% + 8.0% of the time the polyps grow at least 50% larger
Thanks, Sarah and let me know if you have any questions.
David Emerson
Director PBC
I am 45. I had what I believe to be a sizeable polyp (1.5″ long x. 75″ wide, oval, with a. 25″ stalk) fall off of my uterus. I passed it through my cervix, along with a lot of blood, mid cycle. The polyp is at the lab, I waiting on diagnosis. Once the polyp passed, the bleeding stopped for 2 days, but then I passed a very large clot and started bleeding heavily and nonstop since.
Here is my question: could the polyp stalk have been attached to a radial artery in the uterus? And could that be where all of my subsequent blood is coming from? When the polyp fell off it ruptured a good size blood vessel?
ReplyHi Juliana-
I am sorry to read of your health challenges and I wish I could shed some light onto you situation. However the situation you describe needs to be observed and diagnosed by a medical doctor. Let me know if you would like information about nutritional supplementation to eliminate endometrial polyps.
Thanks
David Emerson
ReplyHi
I am TTC since 6 months. Was diagnosed with PCOD and was put on clomid (500mg in the first cycl and then 100mg in the second)and metformin(500mg twice a day).Went for follicular scans and it was found in the first cycle that there was an endometrial polyp of 6mm. In the second month it reduced to 3mm. The gynaec is saying to get it removed. Please suggest if it would be a good option to go for the polyp removal keeping in mind that the polyp shrinked on its own.
ReplyHi Maryam-
Great to read that you are trying to conceive. I am sorry to read of your Polycystic ovary syndrome. Your question “Please suggest if it would be a good option to go for the polyp removal keeping in mind that the polyp shrinked on its own” depends on your wishes. Meaning that it would appear that your polyp is disappearing on its own. Nutritional supplementation such as green tea extract could enhance the shrinking.
On the other hand, your thinking about trying to conceive may make it difficult for you to wait patiently while your endo polyp shrinks and disappears. When I’ve read comments from women trying to conceive only to discover an endo polyp, they often sound as if they can’t wait to cut out the polyps so they can hopefully conceive.
Does this make sense to you? I am 55 and after years of side effects from my cancer I believe that people should go under the knife only if they have to. Waiting to cure an endo polyp naturally makes sense to me. But then again, my son Alex is sixteen and my wife and I don’t want more kids.
That comment was meant to be a bit humorous but my comments never come across as being funny. Sorry. I’ve tried to present you with both sides of your decision and your answer depends on you priority.
If you are interested in more info about nutritional supplementation with studies to suggest therapies and dose to further reduce your endo polyp, let me know.
Let me know if you have any questions. Thanks and good luck.
David Emerson
ReplyThank you so much David for such an unbiased advice. Even I am afraid of getting it cut just because the metal that would be going inside might affect something which it should not.
ReplyThank you Maryam-
Here are studies that cite green tea extract, curcumin and vitamin D3 as nutritional supplements to shrink endo polyps. Good luck and let me know if you have any questions.
David
ReplyHi David, I was diagnosed by my gynae with a few small endometrial polyps. Has been trying to conceive. Should I proceed with hysteroscopy to increase my pregnancy chances or should wait and see?
I have a family history of cancers and I am a little worried.
Appreciate your opinion. Thanks!
ReplyHi Reg-
I understand your concern and thanks for reaching out. Your questions are some of the most often asked on PBC. I will try to link the info below for you to think through your options to hopefully help your decision-making.
First things first. As stated in the study that you came in on, your risk of one of your polyps being malignant is less that 2.5% Less depending on your age, lifestyle, diet, etc.
To think through to have your polyps removed or wait and see, first, the studies’ statistics about your polyps are below. To help you shrink your polyps, I will link studies and info about supplements below.
1) 13.7% of the time the polyps resolve on their own-
2) 41.7% of the time the polyp size stays the same-
3) 20.3% of the time the polyps shrinks at least 1mm-
4) 16.3% + 8.0% of the time the polyps grow at least 50% larger
Here is a blog post about uterine fibroids/ endo polyps that links to a study about green tea extract and UF/endo polyps-
Green Tea Extract shrink Fibroids
The brand, dose, etc. of green tea extract that I use and recommend.
Vitamin d and the risk of uterine fibroids.
This study is dry and full of medical jargon but it says that lower blood levels of vitamin D increase the risk of Uterine Fibroids. By supplementing with vitamin D you may either get rid of your fibroids or reduce the risk of a recurrence of getting fibroids.
If you are wondering how to check your blood levels of vitamin d you can get this tested or simply start supplementing with vitamin D. I take 2000 mg daily with the brand linked below. Increased blood levels of vitamin D will reduce your risk of several chronic diseases. Read the post about vitamin d’s health benefits to learn more.
Vitamin D3 health benefits
Inhibitory effect of curcumin on uterine leiomyoma cell proliferation.
Again, research study full of jargon but the bottom line is that curcumin “inhibits” uterine fibroid growth.
This is the brand and dose that I use and is most bioavailable (gets in your blood).
To summarize Reg, taking one capsule of green tea extract, vitamin d and curcumin with food daily will, according to the studies, should help your endometrial polyps shrink.
Please ask me questions if anything is unclear or if you are wondering about anything.
thanks
David Emerson
ReplyI had an Ultrasound of the pelvis. The uterus measures 8.5x4x4.5cm with a 2.5 cm fibroid with a 5 mm calcification noted. I am 72 years young…I had a polyp removed with a D&C over 8 years ago and several months later a new one developed and I had that removed. I DO NOT want to go through this again!…It’s not a pleasant experience as no surgery no matter how minor is! That being said, I am not sure what to do? I have not had a vaginal ultrasound as I am more scared then ever to hear if that is a “uterine polyp” or not?…What do you think?
ReplyHi Gayle-
Thanks for reaching out. Your questions, concerns are some of the most frequently asked questions I get on PBC. Yes, I have read that surgical removal of endo polyps is painful. And yes, they can return.
Ahhh, the first issue I have to acknowledge is that I understood a uterine polyp, an endometrial polyp and a fibroid to be basically the same thing. All caused by estrogen, all low risk of malignancy, problematic for sure but not life-threatening.
All the studies I will link below talk about natural therapies to either remove polyps/fibroids and or reduce the risk of relapse (polyps returning…). I take green tea extract, vitamin D3 and curcumin myself for a host of medical reasons, mostly to reduce the risk of my cancer relapsing.
To confirm the basic statistics from the previous study:
1) 13.7% of the time the polyps resolve on their own-
2) 41.7% of the time the polyp size stays the same-
3) 20.3% of the time the polyps shrinks at least 1mm-
4) 16.3% + 8.0% of the time the polyps grow at least 50% larger
Here is a blog post about uterine fibroids/ endo polyps that links to a study about green tea extract and UF/endo polyps-
Green Tea Extract shrink Fibroids
The brand, dose, etc. of green tea extract that I use and recommend.
Vitamin d and the risk of uterine fibroids.
This study is dry and full of medical jargon but it says that lower blood levels of vitamin D increase the risk of Uterine Fibroids. By supplementing with vitamin D you may either get rid of your fibroids or reduce the risk of a recurrence of getting fibroids.
If you are wondering how to check your blood levels of vitamin d you can get this tested or simply start supplementing with vitamin D. I take 2000 mg daily with the brand linked below. Increased blood levels of vitamin D will reduce your risk of several chronic diseases. Read the post about vitamin d’s health benefits to learn more.
Vitamin D3 health benefits
Inhibitory effect of curcumin on uterine leiomyoma cell proliferation.
Again, research study full of jargon but the bottom line is that curcumin “inhibits” uterine fibroid growth.
This is the brand and dose that I use and is most bioavailable (gets in your blood).
To summarize, taking one capsule of green tea extract, vitamin d and curcumin with food daily will, according to the studies, should help your endometrial polyps shrink.
Please ask me questions if anything is unclear or if you are wondering about anything.
thanks
David Emerson
ReplyYOU NEVER TOLD ME THE “BRAND” OF CIRCUMIN OR GREEN TEA EXTRACT TO USE? PLEASE ADVISE.
ReplyHi Gayle-
The brand of curcumin I take is LEF SuperBio Curcumin- I also have “prime” on amazon.com so I don’t pay for shipping. I supplement a lot.
A Tool for Cancer Patients, Survivors & Caregivers – Amazon Prime
http://www.amazon.com/Life-Extension-Bio-curcumin-Vegetarian-Capsules/dp/B000X9P5GM/ref=sr_1_1?ie=UTF8&qid=1451491344&sr=8-1&keywords=superbiocurcumin
As for green tea extract (EGCG) I supplement with LEF Mega Green Tea- I take the dose that is recommended on the label. The recommended dose of green tea extract from this study is 800mg, about the same daily dose as the label recommends.
Here is the green tea/endo polyps study-
Green Tea Extract shrinks Uterine Fibroids
Let me know if you have any questions-
David Emerson
Reply[…] will seek a surgical therapy for their uterine fibroids. But it’s important to point out that a study on this site documented that the over 71% of uterine fibroids either remain the same, shrink or disappear on their […]
ReplyHello,
I am 42 years old. I was diagnosed with a uterine polyp in 2008 and had it removed. Then, in 2014 I started having the same symptoms: cramping and spotting between periods and was diagnosed with a uterine polyp again. I had it removed in December 2014. Both pathology reports came back negative. 6 months after my last polypectomy I was diagnosed with a uterine polyp again. What should I do: have it removed again? Why do they keep coming back? I am 5’6”, 124 lbs, pretty healthy, active, and I exercise regularly. I am desperate. I am afraid my doctor is going to suggest hysterectomy and I do not want to have it. What are my choices?
ReplyHi Victoria-
I understand why you feel desperate however please understand recurring polyps are common. I don’t want to sound like I am minimizing your situation. I will give you choices based on studies below. I am not a doctor and cannot give advice. I am simply offering studies that can guide your thinking. Sorry for the long reply but I try to include studies to explain why I do what I do or to support recommendations.
Also, your current lifestyle, 5’6”, 124, (trim), active, exercise, are all good. Keep these up. Please do not have a hysterectomy.
As the endometrial polyps over-treatment article stated, if you are diagnosed with a polyp and do nothing,
1) 13.7% of the time the polyps resolve on their own-
2) 41.7% of the time the polyp size stays the same-
3) 20.3% of the time the polyps shrinks at least 1mm-
4) 16.3% + 8.0% of the time the polyps grow at least 50% larger
I will assume that you understand conventional therapies to remove polyps aka polypectomy, etc.
Here is a blog post about uterine fibroids/ endo polyps that links to a study about green tea extract and UF-
Green Tea Extract shrink Fibroids
Vitamin d and the risk of uterine fibroids.
This study is dry and full of medical jargon but it says that lower blood levels of vitamin D increase the risk of Uterine Fibroids. By supplementing with vitamin D you may either get rid of your fibroids or reduce the risk of a recurrence of getting fibroids.
If you are wondering how to check your blood levels of vitamin d you can get this tested or simply start supplementing with vitamin D. I take 2000 mg daily with the brand linked below. Increased blood levels of vitamin D will reduce your risk of several chronic diseases. Read the post about vitamin d’s health benefits to learn more.
Vitamin D3 health benefits
nhibitory effect of curcumin on uterine leiomyoma cell proliferation.
Again, research study full of jargon but the bottom line is that curcumin “inhibits” uterine fibroid growth.
This is the brand and dose that I use and is most bioavailable (gets in your blood).
Curcumin health benefits
To summarize Victoria, taking one capsule of green tea extract, vitamin d and curcumin with food daily will, according to the studies, reduce the risk of a recurrence of uterine fibroids aka endometrial polyps. Again, according to those studies there are not side effects with this form of integrative or complementary therapy.
I hope I have answered your question “what are my choices.” Please ask me questions if anything is unclear or if you are wondering about anything.
thanks
David Emerson
Reply[…] The single most asked about cause of cancer on PeopleBeatingCancer is uterine fibroids (UF) aka endometrial polyps (EP). Fortunately I posted a study that determined the average risk that UF/EP is cancerous is 2.5%. […]
ReplyHi Jeanette-
I hope you are feeling okay.
My guess is that you are asking this question because you are anxious about your pathology report. The answer is up to your pathologist though it should not take too long. However I will say that according to the study you came in on, depending on your age, pre/post men. status, bleeding or not, there is approx. a 3.8% risk of your polyps being malignant.
Further if you are looking for information about evidence-based research into therapies to reduce the risk of relapse, please let me know.
I am sorry I couldn’t be more specific.
good luck
David Emerson
ReplyHi
I am 26 years old and trying to conceive from last 4 years reacently under gone hystoscopy 3 months back and my dr put me on meditaion ie on dhupaston for 3 months and after that she asked me to come for follicle scan on d9 so today i went for it the scan showing one more polyp was there and no follicle were there and endometrium is 0.38.so i want to know was there any serice thing to worry ?is there a chane that poly will grow again and the chance of poly becoming cancerous.please suggest
ReplyHi Swethaven,
Your english is difficult for me to understand so I will try to confirm what you are asking. Okay?
You have been trying to get pregnant (excellent) for the past 4 years and you are wondering if everything is okay down there-
1) hystoscopy 3 months ago.
2) dhupaston
3) follicle scan showing one polyp-
4) endometrium is .38
And your question is
” was there any serice thing to worry ?is there a chane that poly will grow again and the chance of poly becoming cancerous?”
The study that you read about endo polyps being overtreated states that 1) the risk that a polyp is malignant (cancerous) is 2.5%. And 24.3% of the time polyps will grow.
Therefore, as the study indicates, the majority of the time, a polyp with stay the same, shrink or disappear. Lastly, while I cannot link the study for you, I’m pretty sure that I read a study saying that removing endometrial polyps INCREASES the chances of getting pregnant.
To summarize: If you are diagnosed with endometrial polyps:
1) 13.7% of the time the polyps resolve on their own-
2) 41.7% of the time the polyp size stays the same-
3) 20.3% of the time the polyps shrinks at least 1mm-
4) 16.3% + 8.0% of the time the polyps grow at least 50% larger
I hope I have answered your questions. Let me know if you need clarification about anything.
thanks and good luck!
David Emerson
ReplyI’m 51, I’ve been in menopause for almost 3 years. A little over a month ago I started bleeding, moderately heavy for about 7 days, then 3-4 days of brown spotting. I went to my gyn who did a biopsy of my endometrium, he said it was normal and there was no thickening, we could skip the ultrasound for now, unless I had any more issues. 4 weeks later I started bleeding again, this time about 4 days. I called to order the transvaginal ultrasound, which they did, and they found a “super tiny” polyp. The dr said, not to worry, it’s so small, they’ll check it again in a year. Everything I read say if you’re post menopausal and bleeding the polyp should be removed. Could it be because there was no thickening? Do polyps and thickening go hand in hand? Does the fact that it’s “super tiny” mean that it’s not likely the cause of the bleeding? I just had a lumpectomy that came back benign, it was a radial scar, “proliferative fibrocystic changes”, I understand a polyp is also an overgrowth of cells, am I creating too much estrogen or something causing these things?
Thanks
Hi Elaine-
Your questions are on-point. However, as I understand it, they can’t be answered definitively. By this I mean that being post menopausal causes changes in your hormones but as you have identified your polyp is tiny and your lumpectomy was benign. Both endo polyps and fibrocystic changes are common.
The stats below are excerpted from the original study and indicate that your tiny polyp will either stay the same size or resolve. Thickening of the endo walls increase these risks but since you have no thickening you are doing well.
To answer your question “am I creating too much estrogen or something causing these things?” Though estrogen is the theory I have never found a study that proves that estrogen produces polyps.
The decision to remove the polyp is up to you however I think your dr. is offering good advice to watch and wait. If you are like me watching and waiting my be difficult. Therefore I can offer evidence-based, modest lifestyle therapies that increase the chances that your tiny polyp will resolve. Moderate regular exercise also may help.
Nutritional supplementation for endo polyps-
To summarize: If you are diagnosed with endometrial polyps:
1) 13.7% of the time the polyps resolve on their own-
2) 41.7% of the time the polyp size stays the same-
3) 20.3% of the time the polyps shrinks at least 1mm-
4) 16.3% + 8.0% of the time the polyps grow at least 50% larger
I hope this helps. Let me know if you have any questions.
David Emerson
ReplyHi there,
I am 32, and was just diagnosed with a uterine polyp. I am having it surgically removed, because I want to start trying to have a baby soon (I already have two). I am scared to death that pathology will come back cancerous. My dr found the polyp because I was having spotting between periods and she sent me for an ultrasound… Any insight to ease my mind?? Thank you in advanced
ReplyHi Naomi-
I understand that any surgery, anything like a uterine polyp can cause a person to be “scared to death.” As for “any insight to ease your mind” I can offer what is quoted in the article- the risk that your polyp is malignant is %2.5 which is reduced if you are postmenopausal. I will assume that you are pre menopausal. Lastly, though I can’t find the study now, I have read that removing polyps may help you conceive.
“Malignant polyps represented 2.5% of the total sample. Postmenopausal bleeding and age greater than 60 years were the only factors that remained associated with a higher risk of malignancy with a prevalence ratio of 3.67 (95% CI, 1.69–7.97) and 1.5 (95% CI, 1.01–1.09), respectively…”
Good luck.
David Emerson
ReplyHi. I am 68 and (obviously) post-menopausal. I’ve never had children and took HRT for only a year about 20 years ago. A recent ultrasound revealed an endometrial polyp with a vascular pedicle (.8 x .5 x .9cm), and a sessile area of tissue (1.2 x .3 x 1.1cm) in my uterus. My doc has recommended a D&C, although I have no symptoms. The radiolist recommends waiting/watching. What do you think?
ReplyHi Rea-
I am excerpting the original article below. You have probably read the percentages but I thought I should cite them again. You know that you are the only one who can make this decision as it is your body. But since you asked my opinion I will offer it.
Based on the risks below, endo polyps will will stay the same or shrink about 75% of the time. Based on this, I would go with your radiologist and watch and wait. The studies I have read say that weight is associated with estrogen and polyps so, at the risk of annoying you I would also recommend exercising.
On a personal note, my own health issues spurred me to live a much healthier lifestyle. So this diagnosis my spur you as well.
Please let me know if you have any questions or comments. Thanks.
David Emerson
“Malignant polyps represented 2.5% of the total sample. Postmenopausal bleeding and age greater than 60 years were the only factors that remained associated with a higher risk of malignancy…
To summarize: If you are diagnosed with endometrial polyps-
1) 13.7% of the time the polyps resolve on their own-
2) 41.7% of the time the polyp size stays the same-
3) 20.3% of the time the polyps shrinks at least 1mm-
4) 16.3% + 8.0% of the time the polyps grow at least 50% larger
ReplyI am almost 49 and am perimenopausal. I have a 18mm endo polyp which was found by having a transvaginal ultrasound in October 2014. I have experienced heavy menses for the last 6 – 8 months and only had the US as I was found to be anaemic. My gyno has suggested surgical removal of the polyp but not hysterectomy, however there is a 3 month wait on the surgery. What are the chances of it growing anymore?
Cheers,
JO – from Australia
Hi JO-
I am sorry to learn of your polyp though I have to say everything you mention sounds pretty normal. This might not make you feel any better but both your situation and what your gyno recommended sounds good. What I mean by this is that in many cases a full hysterectomy may be too much. This procedure may create problems aka side effects years from now.
Surgical removal of the polyp may have the effect of returning your heavy menses to normal. As for the 3 month wait do you mean a 3 month wait for the surgical removal of the 18mm polyp? I am not a professional but the studies I have read indicate that the odds are that 1) the polyp will remain the same, or 2) shrink a bit. Your quality of life (heavy menses) will not change but the time shouldn’t be a problem otherwise.
So to answer your question “What are the chances of it growing anymore?” to quote the study
“1) 13.7% of the time the polyps resolve on their own-
2) 41.7% of the time the polyp size stays the same-
3) 20.3% of the time the polyps shrinks at least 1mm-
4) 16.3% + 8.0% of the time the polyps grow at least 50% larger”
Number 4- the chances of the polyps growing are 24.3%-
Let me know if you have any questions.
Thanks
David Emerson
ReplyHi..I am 30 years old(no children yet), 5’3″height and 73 kgs weight. I have recently diagnosed with hysteroscopy and polypectomy, waiting for my biopsy results(hoping for the best). I am highly desperate to become mother. I am very afraid of multiple polyps found during polypectomy. I was having ovaluation bleeding in b/w my regular periods from many years, where I started noticing much it after my marriage. My only afraid is of endometrial cancer as I was in abnormal bleeding from many years. And please suggest me how to take care of myself not to get any more polyps in future. Thanks in advance and please reply asap
ReplyHi Radhika-
If I read your post correctly you have been diagnosed with “multiple polyps.” You also have been experiencing menstrual bleeding that increased with regular sex? (“after my marriage…”). Further, you are young- 30 years old.
According to the study outlined in the original article about overtreatment of endo polyps:
1) “Malignant polyps represented 2.5% of the total sample” further Women who were menopausal with polyps had an almost 4-fold higher likelihood of that polyp being malignant than when polyps were diagnosed in reproductive-aged women,”
The risk of malignant polyps is low at 2.5%
2) I will try to link the study but it is my understanding that removal of endometrial polyps may help to become pregnant. Below is a list of therapies to get rid of endometrial polyps. Please discuss these therapies with your doctor.
Radiofrequency ablation – This technique delivers intense heat to destroy thickened or abnormal tissue inside the uterus. An electrode inserted into fibroid tumors or thickened areas melts tissue away.
High-frequency ultrasound – This method uses high-frequency ultrasound to destroy small fibroid tumors.
Myomectomy – A surgical procedure used to treat uterine fibroids. The uterus remains intact and only the fibroids are removed.
Intrauterine device (IUD) – Inserting an IUD within the uterus (similar to the birth-control device) laced with the hormone progesterone can reduce endometrial wall thickening and control excessive menstrual bleeding.
Loop electrosurgical excision procedure (LEEP) – A conservative procedure that preserves the uterus while removing abnormal cells in women with cervical cancer.
Hormonal therapy – Hormone pills, similar to birth control pills, or hormone injections can reduce pain, and excessive or irregular bleeding.
Anti-estrogen therapy – Hormone blockers given until natural menopause occurs can keep ovaries from producing estrogen, which can shrink fibroids.
Uterine artery embolization (UAE) – Usually performed by an interventional radiologist, this procedure cuts off the blood supply feeding fibroids. A catheter is threaded through a blood vessel in the groin to the area of the uterus. Eventually tissue fed by the zapped blood vessel dies and is reabsorbed.
Dilatation and vaginal curettage (D&C) – A procedure that resurfaces the uterine lining and may help to control excessive bleeding temporarily.
Pain Medications – Some non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, not only reduce painful cramps but can calm heavy bleeding.
Herbal and dietary supplements – Certain dietary supplements and teas may help relieve menstrual cramps and regulate blood flow. Cramp bark, derived from the viburnum plant can quell cramping; valerian root has a sedating effect that can relax the uterus; pycnogenol can reduce swelling and pain; and red raspberry leaf tea (rubus) can help keep the uterus muscle toned.
Radhka, please let me know if you have any question. I hope this info helps.
Thank you,
David Emerson
ReplyHello David
I just came across your reply,thank you very much for your reply.
Good news is that I got my biopsy results absolutely normal. My gynic confirmed my womb and uterus are completely fine. After polyp removal, endometriasis and my extreme period pain is completely gone. My periods are back with normal cycle length 28 days. I am happy I have came across many wonderfull people like you through my journey. ASAP I will update for sure my pregnancy news.
(FOR ALL LADIES ON THIS WEBSITE) Dear friends, I know many of us are going through much stress and depression. My suggestion is donot get panic by polyp stuff,I suffered this from past 2 years and now I am back to normal. Polyps are curable and this whole process of treatment is to make us normal again. Trust me everything will be okay soon. All the best for everyone here.
Thanks David
ReplyRadhika-
Wow. Thank you very much for relaying your status to me. I produce an annual report and your story is sure to be front and center this year. Please keep in touch.
David Emerson
ReplyHi David
Thanks for your reply. I am happy to update you that I am 16 weeks pregnant now and everything is going well with my baby.
(I conceived in 2 months after my surjery)
All the very best for everone here.
Thank you
ReplyHi David,
I am 50, experiencing painful, irregular periods with excessive bleeding. I had a vaginal ultrasound and Dr thinks I have a polyp the size of a golf ball with a smaller one attached, in my uterus. Dr. wants to do a hysterectomy of the uterus and Fallopian tubes. Said it was too big to get out with hysteroscopy, would have to cut it up to get it out. He also said my endometrial lining was ‘sticky’ and I have several small fibroids in my uterus as well. My first question is: would it be risky for him to ‘cut it up’ to get it out if there happened to be cancer cells in it? Would they spread? Also: Should I request a biopsy? I’m thinking it might be difficult to get a biopsy of both polyps.
I’m concerned that if I don’t get the hysterectomy and the polyps return in a few years, I will most likely be post menopausal by then and I’ve read about the increased risk of those polyps being malignant after menopause. Any insight you have would be greatly appreciated:)
Thank you.
Hi Susan-
I’d like to research your specifics. I need to research polyp removal- by “risky” are you thinking of the spread caused by power morcellators? Again, I need to research this issue further. As for a biopsy, yes, I think this is a good idea. Biopsy-ing of all polyps makes sense but I will reply again to morrow. There is always a risk of polyps returning. And the risk of malignancy increases a bit with post menopausal women. I will reply again.
thanks and hang in there.
David Emerson
ReplyHi Susan-
I’ve been researching the issues you ask about in your post and I will try to address each question:
1) “would it be risky for him to ‘cut it up’ to get it out if there happened to be cancer cells in it? Would they spread? Also: Should I request a biopsy? I’m thinking it might be difficult to get a biopsy of both polyps.”
As you can read from the first link below, fibroid tumors can grow as large as “20 cm.” While there may be long-term health issues with hysterectomy, I found no articles or studies talking about any problems associated with removing large polyps or masses. While the risk of malignancy is low, I think it is prudent to make sure your doctor examines the polyp for malignancy.
2) “Should I request a biopsy? I’m thinking it might be difficult to get a biopsy of both polyps.” I have been assuming that you want to remove your polyps one way or another so I’m not sure why you would be thinking about asking for a biopsy. If the masses are removed they will be examined.
Further, I have excerpted and linked discussion of what I read as your type of tumor- “submucosal, bleeding, etc.”
3) “He also said my endometrial lining was ‘sticky’ and I have several small fibroids in my uterus as well.”
Types of Fibroid Tumors
“Fibroid tumors may grow as a single nodule or in clusters and may range in size from 1 mm to more than 20 cm in diameter. Fibroid tumors are the most frequently diagnosed tumor of the female pelvis and the most common reason for a woman to have a hysterectomy. Although they are often referred to as tumors, they are not cancerous.”
“Submucous or Submucosal fibroids are found within uterine lining and can protrude into the uterine cavity. Generally, these are ones that can cause the most problems. Since they are located in the uterine endometrium, they can cause heavy prolonged bleeding during menstruation.”
Long-term Effects of Hysterectomy
4) “I’m concerned that if I don’t get the hysterectomy and the polyps return in a few years, I will most likely be post menopausal by then and I’ve read about the increased risk of those polyps being malignant after menopause.”
As you will read in the above link about possible long term negative side effects of hysterectomy, yes, there are possible problems with a hysterectomy. Also, yes, there is a possibility of polyps returning if you don’t have a hysterectomy. While, according to the research in the original linked study, the risk of malignancy increases slightly with post-menopausal women, the increase is slight.
Is your main concern with long-term problems from a hysterectomy or possible cancer from polyps? I have no experience with this form of polyp removal but I thought would pass along the site to you-
http://www.uterine-fibroids.org/
http://www.uterine-fibroids.org/Debbie.html
thanks and let me know if you have any questions.
David Emerson
ReplyHi, I was diagnosed by intravaginal ultrasound with a polyp of about 1 cm nearly four months ago and I had it removed by hysteroscopy about three months ago. It was non cancerous and my periods have gone back to normal since the op. I am 46 and have been trying for a baby for about 4 years with no success; hormone tests all came back good, could this polyp have been the reason for my secondary infertility and if so how good are my chances of conceiving now? I also had two growths removed from my cervix about 12 years ago, lab results were inconclusive. I have 3 children with previous husband, youngest now being 16 and I had 3 early miscarriages spaced between my 3 children. I have always fallen pregnant very quickly and easily in the past and based on family history am not expecting menopause for another 10 yrs or so!
ReplyHi Joanna-
Your situation seems to be pretty complicated but I will try to link and excerpt studies that address your questions as well as possible. My understanding is as follows:
1) Good to read that the 1 cm polyp was removed, non cancerous and your periods returned to normal.
2) At 46, you are young from an endometrial polyp standpoint.
3) my understanding is that yes, endo polyps can complicate getting pregnant. I will link supporting studies below.
As many of these sites document, endo polyps can complicate getting pregnant-
However, as is discussed in this link, pregnancy outcomes improve with endo polyp removal- click and read this study–
“Women in the study group had a better possibility of becoming pregnant after polypectomy, with a relative risk of 2.1 (95% confidence interval 1.5–2.9). Pregnancies in the study group were obtained before the first IUI in 65% of cases. CONCLUSIONS: These data suggest that hysteroscopic polypectomy before IUI is an effective measure.”
Lastly Joanna, your childbearing history is event filled (congrats on the three kids-BTW and I am sorry to read of your miscarriages)- I don’t think any study can exactly cover all the intricacies of your situation. However, the single most important issue cited by studies is that endo polyp removal improves pregnancy rates.
I hope I have addressed all of your questions or concerns. Let me know if you have any questions.
Thanks and hang in there.
David Emerson
ReplyHey there :
I have a polyp in my urteris, and i booked surgery on the 5th of Jun this year. Here is a problem, i am also on contraceptive pill for cysts, i had ovarian cyst removed early this year.
Here is a problem, i am on holiday at the moment, and on the active pills(the homone ones)at the moment, but i start having light bleeding 6 days ago…….could it caused by polyp ?
Should i be concerned ? how long this bleed can last or when should i be concern ? I am oversea at the moment…….
cheers
ReplyHi Clate-
Thank you for reaching out to PBC. I will try to address each of your question/concerns-
1) “Here is a problem, i am also on contraceptive pill for cysts, i had ovarian cyst removed early this year.” Yes, oral contraception pills are one form of therapy for ovarian cysts.
2) “Here is a problem, i am on holiday at the moment, and on the active pills(the homone ones)at the moment, but i start having light bleeding 6 days ago…….could it caused by polyp?”
To confirm, you were diagnosed with an endometrial polyp for which you will have surgery on June 5th. You are taking contraceptive pills for your ovarian cysts. While on holiday, you are experiencing light bleeding. You are wondering if the light bleeding could be caused by the endometrial polyp?
Yes, endometrial polyps can cause bleeding.
“Cause and symptoms
No definitive cause of endometrial polyps is known, but they appear to be affected by hormone levels and grow in response to circulating estrogen.[2] They often cause no symptoms.[3] Where they occur, symptoms include irregular menstrual bleeding, bleeding between menstrual periods, excessively heavy menstrual bleeding (menorrhagia), and vaginal bleeding after menopause.[2][5] Bleeding from the blood vessels of the polyp contributes to an increase of blood loss during menstruation and blood “spotting” between menstrual periods, or after menopause.[6″
3)”Should i be concerned ? how long this bleed can last or when should i be concern ? I am oversea at the moment…”
Depending on your age, weight and how long you will be on holiday, the articles and studies linked do NOT raise concern for light bleeding. As the original article/study states, the majority of endo polyps resolve on their own. Since you have been through something similar, when you return from holiday I would go see the same physician who worked with you on your uterine polyps.
Let me know if you have any questions.
thanks
David Emerson
ReplyI recently had a polyp that came back as with precancerous cells. I am 52 years old. Have had 4 pregnancies. The doctor did a D&C and mentioned that the lining of my uterus was normal and that she did not find any cancer or precancerous cells. Yet she insists that I should have a complete hystorectomy, due to the fact that polyps come back and since that one had precancerous cells it could indicate that in the future I could have cancer.I mentioned to her if we could actually monitor this and take a wait and see to monitor, she made a referral to an OB oncologist to get her opinion and also a plan of action to monitor, since she stated the norm is to do hystorectomy in this situation.
What are the chances of a precancerous polyp turning to cancer after it has been removed.
Hi Roxana-
Normally I begin these responses by saying that I am sorry that the person has been diagnosed with such and such but your post reads as if you did everything possible for someone with a diagnosis of a uterine polyp. You have made all the right decisions. I know of no studies of precancerous polyps sprouting more polyps that are cancerous. While a person can get another polyp after D&C removal, I have never read a study that cites an increased risk of malignancy AFTER polyp removal.
I believe the point of the D and C that you underwent is to remove any chance of cancer. Yes, there is always a chance of another polyp in the future, non, pre or cancerous but I believe that you are correct in wanting to take a wait and see approach.
I understand that it is difficult to not do what a doctor “insists” on but you are the patient and it is your body. I am not qualified to tell you what to do. I am simply saying that your reasoning sounds correct to me. Based on the original “overtreatment” article in addition to the article linked below, there are small chances of premalignant polyps (1.6%) and malignant polyps (2.5%) but as you say, you had the pre malignant polyp removed.
You are young (52) and this reduces your risks of malignant polyps further. The decision to have a hysterectomy is yours. I wish I could find a study that talks about cancerous polyps after D and C but I can’t find any.
“Women were diagnosed with benign lesions in 95.8% of cases. Premalignant polyps accounted for 1.6% of the total number of cases. Malignant polyps represented 2.5% of the total sample. Postmenopausal bleeding and age greater than 60 years were the only factors that remained associated with a higher risk of malignancy with a prevalence ratio of 3.67 (95% CI, 1.69–7.97) and 1.5 (95% CI, 1.01–1.09), respectively.”
I hope this reply has helped. Please ask any more questions that you may have.
thanks
David Emerson
ReplyHi David,
I am a 31 year old woman with no children yet, but hoping to conceive within the next couple of years.
I have had completely normal, regular periods all my life, until 5 months ago. Since that time I have had bleeding between each period (sometimes light staining, sometimes heavy with clots), pain and bleeding after sex and cramping randomly throughout the month.
Today I had a trans-vaginal ultrasound which showed up what the sonographer called a small endometrial polyp.
I have to wait a week for the doc to report on it, and I’m a little scared- hoping you could provide some advice/reassurance.
Am I right in thinking it is very unlikely to be cancerous? And is my best option to have it removed? I am slightly overweight so would decreasing my weight help with thee symptoms of this polyp or just help prevent more in the future?
Many thanks xx
Hi Caroline-
Your post is well-written and your thinking is logical- right off the bat you sound like you are handling your situation well. I don’t mean to sound silly but you really do sound on top of your situation. I will try to address your questions one at a time. Let me know if I miss something.
1) “Am I right in thinking it is very unlikely to be cancerous?” Yes, very unlikely. 2.5% chance. You have a small risk of malignancy. You are young, pre-menopausal with a diagnosis of a “small endo polyp.” All good. To quote the study-
“Malignant polyps represented 2.5% of the total sample. Postmenopausal bleeding and age greater than 60 years were the only factors that remained associated with a higher risk of malignancy…”
2) “And is my best option to have it removed?” Of course this is up to you. I wrote the blog post based on the study saying that endo polyps where over-treated. My advice is to take it one test at a time. In other words, talk to your doc and see how often you can get tested, see how your “small endo polyp” goes. The odds are that your polyp will remain the same, shrink or disappear.
“1) 13.7% of the time the polyps resolve on their own-
2) 41.7% of the time the polyp size stays the same-
3) 20.3% of the time the polyps shrinks at least 1mm-
4) 16.3% + 8.0% of the time the polyps grow at least 50% larger”
As for your weight, yes, according to the study, endo polyps may be triggered by estrogen. Losing weight reduces estrogen. At least while you are concerned about your polyp working a bit to help your body shrink it or resolve it will make you feel better I think.
I hope this helps. Let me know what your doc tells you.
Hang in there.
David Emerson
ReplyHi,
I have only today got my report which says i have an endometrial polyp! i am 41, over weight, un-exercised, have excessive bleeding during my periods which are regular and last for 5 days incidentally, and i also have multiple cervical cysts. my instinct is to not do anything surgical … not even a biopsy. to wait and watch and try medication and life style changes! there is no history of cervical or breast cancer in my family but i lost 3 relatives on my father’s side to cancer including my father in 2013. is it foolish of me to even consider taking a non-surgical stance?
Hi Priya-
I will try to address your question ” is it foolish of me to even consider taking a non-surgical stance?” by outlining the findings of the article about endo polyps.
First and foremost, at 41 you are not menopausal. This is good as menopausal has a 4 fold higher likelihood of a malignant polyps.
“Women who were menopausal with polyps had an almost 4-fold higher likelihood of that polyp being malignant than when polyps were diagnosed in reproductive-aged women,” said Dr. Kaunitz. Correspondingly, a polyp was 2-fold more likely to be malignant in women with bleeding than in those who were asymptomatic…”
Secondly, yes, you mention “excessive bleeding” but again, the article mentions “postmenopausal bleeding” as a potential risk factor.
““Malignant polyps represented 2.5% of the total sample. Postmenopausal bleeding and age greater than 60 years were the only factors that remained associated with a higher risk of malignancy…”
Finally, with regard to “taking a non surgical stance” as you say, by watching and waiting, the majority of the time, the polyps shrink or remain stable.
“To summarize: If you are diagnosed with endometrial polyps:
1) 13.7% of the time the polyps resolve on their own-
2) 41.7% of the time the polyp size stays the same-
3) 20.3% of the time the polyps shrinks at least 1mm-
4) 16.3% + 8.0% of the time the polyps grow at least 50% larger”
Having said all that, the decision comes down to what you feel most comfortable with. Yes, I would encourage you to exercise modestly and lose some weight but I would say that regardless. In other words, I am a cancer survivor myself and I read studies all the time about how lifestyle and nutrition can lower risk of cancer or cancer relapse.
If you would like to pursue taking steps to reduce your risks of cancer (your father’s side of the family) I will email studies and articles about specifics that may help you. But again, it is up to you. I don’t want to overwhelm you any more than you are.
Lastly, you can take a watch and wait approach slowly- meaning a few months at a time. Re assess your thinking after you see your doctor again in a few months.
Let me know what you think or if you have any questions.
David Emerson
Replyhi david,
thanks for your reply. the thing is, i have a mental block against biopsies. i have actually seen my father’s lymphnode tumour grow drastically after we nicked it to sample a piece for the biopsy, right in front of my eyes! and all the online testimonials that i have read, tell me, removing a polyp once is not a guarantee it will not re-occur. so if i am willing to put up with the monthly menace of a painful period, why should i tamper with my body? i am saying all this as my gynacologist and Gp are out of town! and this was too much info inside of me! after meeting with my treating doctor, i might be compelled to take a more cerebral. less emotional decision!
Priya-
You are correct, polyps may regrow after removal. And I understand having difficulty with biopsies. And yes, taking some time to both think through the issues as well will help you calm down and then talk to your doctors. The way I have learned to handle my many cancer related issues is to look at each logically and take my time to think through all the issues. Let me know if you have more questions.
David
Replyand yes i would really appreciate you emailing me studies on how to reduce instances of cancerous occurrences if there is a family history! thanks …
ReplyPriya-
I should have been more specific- please tell me the types of cancer- prostate, colon, breast, etc. Certain supplements have shown anti cancer action against specific cancers. Thanks
David
ReplyI am 47 years old, still have my regular periods, and have 3 grown children. I have just recently been diagnosed with my 3rd round of uterine polyps. I was first diagnosed in 2009 and had a d&c for removal of the benign growths. Exactly 1 year later, the polyps returned and I had a uterine ablasion…again the polyps were benign. After that I lost about 80 lbs and had no recurrence for 3 years. I have recently begun to gain some of my weight back, and Now I have just found out I have 2 new polyps. I am wondering about surgical treatment? Since I am aware that estrogen helps them grow and my added weight makes me produce a lot of estrogen…I was wondering if I could just watch the polyps for a few months and get back on my eating a exercise plan to see if that helps instead of a major surgical procedure (I don’t do well under anesthesia). Or since it is my 3rd recurrence, should I just opt for the d&c or hysterectomy (as my Dr. suggested). My only symptoms of these polyps have been sight bleeding I between my periods — no pain, no excessive bleeding or cramping. I am afraid that if I wait, since it is my 3rd occurrence, my risk for cancerous cells to show up will be high. I would love to hear someone else’s take on my particular case.
ReplyHi Jacqui-
I have one adolescent son and I can only imagine how rewarding it must be to have raised 3 children. Congrats.
Based on your post and your question, it seems as though you understand your body and endo polyps pretty well. While I am not qualified to give you a medical diagnosis to your questions:
1) yes, according to the study, estrogen may be a cause of polyps
2) your second question sounds as if you would prefer to wait for a few months rather than surgery. As the study’s results excerpted below indicate, the odds are that polyps either resolve on their own, remain the same or shrink. Exercise and diet may help this.
Further, you are pre-menopause and as you say, bleeding is slight. I have not read that a third recurrence of polyps increases the risk of cancer.
“To summarize: If you are diagnosed with endometrial polyps:
1) 13.7% of the time the polyps resolve on their own-
2) 41.7% of the time the polyp size stays the same-
3) 20.3% of the time the polyps shrinks at least 1mm-
4) 16.3% + 8.0% of the time the polyps grow at least 50% larger”
If you have any other questions don’t hesitate to reply. Thanks and good luck.
David Emerson
ReplyDear David ,
I’m glad to you have made this support group for endometrial polyp. Diagnosis end with this today which is 21x10mm .
Could you please tell different treatment available today .
What could I eat or do to combat endometrial polyp .
Thank you
Vasu
Hi Vasu-
Before we discuss possible therapies for endo polyps, we should confirm the basic issues discussed in the article you read about possible overtreatment of endo polyps.
If you have been diagnosed with endo polyps the first things to think about 1) if you are pre or post menopause as this affects your polyps risk of malignancy and 2) have you experienced bleeding? This also affects the risk of malignancy.
I have excerpted that part of the blog post which discusses specific percentage.
“Malignant polyps represented 2.5% of the total sample. Postmenopausal bleeding and age greater than 60 years were the only factors that remained associated with a higher risk of malignancy with a prevalence ratio of 3.67 (95% CI, 1.69–7.97) and 1.5 (95% CI, 1.01–1.09), respectively…”
“To summarize: If you are diagnosed with endometrial polyps:
1) 13.7% of the time the polyps resolve on their own-
2) 41.7% of the time the polyp size stays the same-
3) 20.3% of the time the polyps shrinks at least 1mm-
4) 16.3% + 8.0% of the time the polyps grow at least 50% larger”
To answer your question about anti endo polyp nutrition, the only site that I found that discusses endo nutrition simply talks about estrogen and a healthy balanced diet.
http://www.livestrong.com/article/471313-uterine-polyps-and-a-healthy-diet/
Rather than approaching endo polyps from a nutritional standpoint, the link below will take you to sites about anti endo herbs. I cannot vouch for the efficacy of this info as I have no experience with anti endo polyps herbs.
What I am saying is that I could not find much about nutritional solutions to endo polyps. Let me know if you have any other questions.
thanks
David Emerson
ReplyPS I am not overweight, am a (healthy) vegan (8 years) and exercise every other day (swim, lift weights, windsprints, strength train). I was on hormones for birth control when I was younger, but no hormone replacement therapy during menopause (despite the majority of Dr’s recommending versus natural options). It’s possible the polyp/thickening of the endometrial lining developed in response to a pregnancy/abortion I had, although that’s been over 20 years ago…
ReplyHi Kathleen-
My guess is that you are thinking though your endo issues- you ask questions in your other two posts but not this post. Let me know if you have other questions. I will address the other post now.
thanks
David
Hi there,
Thanks for this website.
I’m 62, and bled slightly leading to an ultrasound (thickening of the endometrial lining (7 mm)), two failed biopsy attempts (stenosis of the us), a sonohysterogram (pea-size endometrial polyp), and a failed polyectomy (positioning of the uterus/scar tissue prevented the Dr. from “seeing” the right place to enter the uterus). In retrospect, I’m not sure why the long path of testing was recommended. Seems like you’d go straight to a sonohysterogram for a post-menopausal woman with symptoms (biopsies are not representative and ultrasounds don’t have the resolution sonohysterograms do). I divert…. Among other options, my Dr. wants to discuss a short course of hormones to “soften” the scar tissue to attempt another polyectomy. I am extremely ambivalent about another surgery attempt, not only because I’m this side of terrified of sedation, but the expense alone (we’re up to $4000 out of pocket, and still waiting for the anesthesiologist’s bill) and because the potential of her not being able to complete the surgery still exists. In reading Dr. Hartman’s study where 76% of 300 patient’s polyps either resolved, had no change in size, or decreased at least 1 mm, it causes one to pause when considering surgery, although his study did not cite what % went on to develop malignant cancers. At this point I’m inclined to try a natural approach–herbs, detox, diet, and appreciate any studies and treatment plans you can point to where this approach resolved these polyps. Thanks again!!
ReplyHi Kathleen-
If I understand this post, you are asking for non-invasive or “natural” therapies for removing endo polyps? You seem to have a good understanding of Dr. Hartman’s study of polyps- yes, while the study documents the percentage of endo polyps that either shrink, resolve or remain the same, Dr. Hartman’s study does not cite what, if any, polyps become malignant.
There are drug therapies listed in the article though my guess is that you don’t want to pursue drugs to shrink your polyps.
Reading through some of these sites about herbal remedies for endo polyps makes me nervous in that there is little if any evidence-based research or documentation. I wish I could offer better info… let me know if you have any questions.
David Emerson
ReplyAre there any foods I can be eating to combat endometrial polyps?
ReplyJessica-
Thanks for posting. I will email you directly.
Thanks
David Emerson
ReplyI’m keen to know what food can prevent endo polyps too. It’s my 2nd time having polyps (3cm this time) in 2 yrs.
ReplyHi Blue-
I have pasted info below about 1) antioxidant supplementation that studies show eliminates endo polyps, herbs that are shown to reduce the risk of endo polyps and some general info about anti-endo polyp nutrition.
I supplement with curcumin, green tea extract and vitamin D myself for a variety of health reasons. Let me know if you have any questions.
thanks, David Emerson
Here is a blog post about uterine fibroids/ endo polyps that links to a study about green tea extract and UF-
Green Tea Extract shrink Fibroids
Vitamin d and the risk of uterine fibroids.
This study is dry and full of medical jargon but it says that lower blood levels of vitamin D increase the risk of Uterine Fibroids. By supplementing with vitamin D you may either get rid of your fibroids or reduce the risk of a recurrence of getting fibroids.
If you are wondering how to check your blood levels of vitamin d you can get this tested or simply start supplementing with vitamin D. I take 2000 mg daily with the brand linked below. Increased blood levels of vitamin D will reduce your risk of several chronic diseases. Read the post about vitamin d’s health benefits to learn more.
Inhibitory effect of curcumin on uterine leiomyoma cell proliferation.
Again, research study full of jargon but the bottom line is that curcumin “inhibits” uterine fibroid growth.
This is the brand and dose that I use and is most bioavailable (gets in your blood).
Uterine Polyps and a Healthy Diet
Rather than approaching endo polyps from a nutritional standpoint, the link below will take you to sites about anti endo herbs. I cannot vouch for the efficacy of this info as I have no experience with anti endo polyps herbs.
https://search.yahoo.com/yhs/search;_ylt=A0LEV7.XZAxVvDEAnbAnnIlQ?p=herbs+for+endometrial+polyps+removal&ei=UTF-8&hsimp=yhs-002&hspart=mozilla&b=1
I was recently told I had uterine polyp. My first check up in November 2014, was 16mm. Follow up in January 2015, grew to 17.5mm. I am 33 years old and have two children, both via C-Section. My doctor suggested d&c, but I’m worried. All I read is that size of the polyp matters and is most related to cancerous. My doctor tells me I shouldn’t worry because of my age. But I can’t help to worry and especially after reading the size of the polyp matters. Could you please give me more information regarding women my age and the size of the polyp. Thanks!
ReplyHi Yahaira-
I will spell out your questions as I understand them. Let me know if I misunderstand something.
1) What is “d&C?” What are possible side effects?
http://en.wikipedia.org/wiki/Dilation_and_curettage
2) Age at diagnosis?
Yes, the article linked below does say that younger women have less chance of polyp malignancy.
“Because of the low prevalence rate of malignancy in asymptomatic young women with no risk factors, routine removal of the lesions might be avoided because of its lack of cost-effectiveness. ”
http://www.medscape.com/viewarticle/754861_6
3) Size of polyps and how they relate to your health?
I can’t find any studies that say anything about the size of endo polyps beyond saying that polyps do vary in size, some shrink and some grow.
“Endometrial polyps are usually benign although some may be precancerous or cancerous.[2] About 0.5% of endometrial polyps contain adenocarcinoma cells.[10] ”
Let me know if you have any other questions.
David Emerson
ReplyThanks David! I went in for my D&C Jan 29. Waiting on my results this Thursday.
ReplyComments from Margaret-
I have had three d&c’s/ with hysteroscopes-1 every year at the same time for a or I believe recurring polyp.
I am a nurse myself and work in the operating room-have for 48 years.
As to my experience as to note attached of woman in her 30’s, I feel are different. My research on the polyp occurrence took in my age, size-pudgy so careful to watch such as it heightens estrogen and thus that the higher incidence of polyps.
Though two different Drs did my 3 procedures, which included a hysteroscopy, I feel certain neither fully excised the polyp completely the first two times. I hope that is so, as if this thing comes back a fourth time I will be having a hysterectomy.
Goodluck!
ReplyHi Yahaira,
How are doing now ? What was your treatment ? I also have been diagnosed with EP. Going in for surgery soon.
Thanks
Vasu
I’ve been ttc for 8month, recently found out I have uterine polyps 2 of them and 2mm each. Thinking bout getting the surgery to get it removed.will removing it increase my chances of getting pregnant?
ReplyHi Bee-
Wonderful to read that you and your husband are trying to conceive. While the article focuses on endometrial polyps not uternine, being peri menopausal lowers your already very low risk of the polyps being cancerous.
Now then, as for your question “will removing it increase my chances of getting pregnant?” An excerpt from the Mayo Clinic site on the subject may be of interest-
“Complications
By Mayo Clinic Staff
Uterine polyps may be associated with infertility. If you have uterine polyps and you experience infertility, removal of the polyps might allow you to become pregnant.
Uterine polyps also may present an increased risk of miscarriage in women who undergo in vitro fertilization (IVF). If you’re considering IVF treatment and you have uterine polyps, your doctor may recommend polyp removal before embryo transfer. ”
http://www.mayoclinic.org/diseases-conditions/uterine-polyps/basics/complications/con-20027472
According to the article-
“Prognosis and complications
Endometrial polyps are usually benign although some may be precancerous or cancerous.[2] About 0.5% of endometrial polyps contain adenocarcinoma cells.[9] Polyps can increase the risk of miscarriage in women undergoing IVF treatment.[2] If they develop near the fallopian tubes, they may lead to difficulty in becoming pregnant.[2] Although treatments such as hysteroscopy usually cure the polyp concerned, recurrence of endometrial polyps is frequent.[6] Untreated, small polyps may regress on their own.[10]”
Hope this helps. Good luck and let me know if you have any more questions. Thanks
David Emerson
ReplyI am a breast cancer survivor and was on tamoxifen for five years. A polyp has just been discovered in my uterus. I am to have an MRI and most likely a biopsy. My question is: due to the tamoxifen is there any chance of the polyp being benign?
ReplyHi BC survivor-
I am sorry to read of your breast cancer diagnosis however it sounds as though you are doing well. I have excerpted several paragraphs from studies that I think speak to your question “due to the tamoxifen is there any chance of the polyp being benign?”
If I understand the studies, the polyp is likely to be benign and a small risk that the polyp is cancerous. I would proceed with both your MRI and a biopsy.
Let me know if you have any questions or concerns. Good luck- David Emerson
“Uterine sarcomas consisting of leiomyosarcoma, carcinosarcoma, high-grade endometrial stromal sarcoma, adenosarcoma, and sarcoma not otherwise specified, are rare and estimated to comprise 8% of all invasive uterine cancer cases (8). In a review of all National Surgical Adjuvant Breast and Bowel Project breast cancer treatment trials, the rate of sarcoma in women treated with tamoxifen was 17 per 100,000 patient years versus none in the placebo group (7).”
“In standard dosages, tamoxifen may be associated with endometrial proliferation, hyperplasia, polyp formation, invasive carcinoma, and uterine sarcoma.
Most studies have found that the increased relative risk of developing endometrial cancer for women taking tamoxifen is two to three times higher than that of an age-matched population (1–3). The level of risk of endometrial cancer in women treated with tamoxifen is dose and time dependent. Studies suggest that the stage, grade, histology, and biology of tumors that develop in individuals treated with tamoxifen (20 mg/d) are no different from those that arise in the general population (3, 4). However, some reports have indicated that women treated with a higher dosage of tamoxifen (40 mg/d) are more prone to develop more biologically aggressive tumors (5).”
“Gibson et al [19] recently reported the results of a retrospective review of endometrial pathology found at dilatation and curettage (D&C) performed in 240 breast cancer patients. Seventy-five (31%) of these patients had received tamoxifen, 20 mg/day, for a mean duration of 26 months as therapy for their breast cancer. Patients in this study were stratified as symptomatic (abnormal bleeding) or asymptomatic (curettage performed as part of another procedure or due to the presence of a thickened endometrial stripe on ultrasound examination).
Among tamoxifen users who were symptomatic at the time of D&C, the incidence of endometrial polyps was 15%; hyperplasia, 2%; and adenocarcinoma, 11%; compared with an incidence of 13%, 4%, and 11%, respectively, for nonusers. Among asympto- matic patients receiving tamoxifen, the incidence of polyps, hyperplasia, and adenocarcinoma was 9%, 0%, and 0%, while nonusers had an incidence of 5%, 4%, and 0%, respectively. All of the cases of endometrial carcinoma were associated with abnormal vaginal bleeding. The 11% incidence of endometrial carcinoma in this study was comparable to what has been reported for all patients presenting with postmenopausal bleeding in the general population [20].
The mean duration of tamoxifen use in those patients found to have adenocarcinoma was 44 months, compared with 18 months in those patients with polyps, and 19 months in the patient with hyperplasia. This difference was not statistically significant, possibly due to small numbers. The authors concluded that short-term tamoxifen use at the 20 mg/day dosage level was not associated with a higher incidence of abnormal pathology, as detected at the time of D&C in breast cancer patients.”
– See more at: http://www.cancernetwork.com/oncology-journal/effect-tamoxifen-endometrium#sthash.C1oysaCn.dpuf
Replypost menopausal…likely polyp…supposed to undergo DNC but hypothyroid…had DNC one year ago…negative pathology…what if I ignore??
ReplyAccording to the article “What Happens When You Watch and Wait?”
From January to July of 2010, Dr. Hartman examined 300 women who had been diagnosed with endometrial polyps in the previous 2 to 43 months. The women ranged in age from 22 to 78 years. Factors considered in this analysis were location of polyp, time interval between studies, menopausal status, abnormal bleeding, blood flow, endometrial thickness, and patient age.
You are post menopausal but what is the location of you “likely polyp,” bleeding, if any, endometrial thickness and age? Based on these answers you can use the article above to decide to treat or to watch and wait.
David
Reply52 yrs old. endometrial thickness over 13. according to GP, from transvaginal us—tiny cyst seen—gyn said suspects likely polyp. scheduled for dnc this week.
ReplyThis is an eye opener for me. In 2011 I had a polyp removed and now i discovered it has recurred again. The doctor says he will carry out the same procedure as well as run more fertility tests to ensure everything is okay since I am also trying to conceive.
However a previous check by a different doctor had shown my fallopian tubes were okay and had not blocked.
I am however sceptical about all this tests and surgery (hysteroscopy) and I wanted to know if theres a need to also do the fertility tests or if removal of the polyp is all I need. I feel as if the doctor could be misguiding me since the surgery for polyp removal is really expensive for me right now and any additional tests for fertility may be even more expensive. Please give me your thoughts which I will highly appreciate.
Gee
ReplyHi Gee-
I don’t mean to sound wishy-washy but everything has risks and benefits. I don’t believe that doctors purposely mislead. I think that recommendations are all based on percentage risks. The article outlines the risks so you have access to some basic information. Consider asking the doctor who wants to do fertility tests what the possible outcomes will be with and without the testing. I have always found drs to be hardworking clinicians but asking the right question helps both dr. and patient to understand the risks and benefits of any procedure. Let me know if you have any other questions. Thanks. David
Hi Gee-
thanks for posting to my blog about endometrial polyp over-diagnosis.
thanks
David Emerson
ReplyHi Margaret-
First of all, thanks for reaching out. Our exchange on PBC will educate others. Your example of regular check-ups and polyp removal will reduce the risk of future cancer.
Research indicates that being 15 years past menses puts you in menopause and should reduce your body’s estrogen production not increase it.
Further, your research/reading up on your situation seems to be on target all around. Yes, menopause causes weight gain as well as hypertension. You are correct to moderately exercise. Losing 7 lbs in three weeks is awesome. You are on the right track.
WebMD’s discussion should be helpful-http://www.webmd.com/menopause/guide/menopause-weight-gain-and-exercise-tips
The key to not yo-yo is to get into a habit of moderate exercise. Please read “The Power of Habit” by Charles Duhigg.
Please confirm with your doctor but I think you can “help myself with polyp recurrence” by managing your weight and hypertension.
Let me know if you have any questions- good luck!!!
Thanks
David Emerson
“Causes of uterine polyps
Uterine polyps are similar to uterine fibroids, most likely developing due to an imbalance of the hormone estrogen. Excess endometrial tissue develops in response to estrogen, causing soft uterine polyps to grow from the uterine lining. Polyps are more frequently seen in perimenopausal or postmenopausal women, but can occur in younger women as well.
Uterine polyps are more common in women with high blood pressure (hypertension), who are overweight, or who are taking tamoxifen (a medication used for treating breast cancer).”
Read more at http://trmbaby.com/for-patients/library/conditions/polyps/#jsyISc1ogRX6jYtQ.99
ReplyI am 64 yrs. old and have breast cancer. I am treating the cancer naturally and have made progress. I recently had a transvaginal ultrasound and the report said I had a 2.6 cm cyst on my ovary and polyp or polyps in my uterus. Right now I chose to try castor oil packs, flaxseed with warm water on an empty stomach and epsom salts bath with a drop or two of pure lavender to shrink it do away with the cyst and polyps. I am going to repeat the ultrasound the end of November and see if there are any changes. I am on a clean diet, take supplements and exercise. I don’t want surgery or a hysteroscopy. I would like to treat naturally. Any suggestions? Thanks.
ReplyHi Sheri-
I am sorry to read of both your BC as well as your cyst and polyp. While the odds are overwhelming that the cyst and polyp is/are benign, and the odds are pretty good that the cyst and polyp will either shrink or resolve on it’s own, let me ask you a couple of questions to clarify things.
1) What was your stage when you were diagnosed with BC? Did you undergo any conventional therapies such as a lumpectomy?
2) What do you mean when you say that “you have made progress?”
Thanks and let me know.
David Emerson
ReplyQuestion: I had a polyp two years ago. It was diagnosed w US using uterine fluid infusion for visualization. An endometrial bx was done. Though negative for ca, I received a hysteroscope/D&C. Path results were negative for ca though a polyp was seen and removed. Then a year ago ( nearly to the the same annual date ) another situation of a polyp occurred. I refused in office bx due to prior severe pain with that process, though an US showed thickening of the endometrium. I was treated again as the year before, with a negative path report though again a polyp via the hysteroscope was seen and removed. Now another year later, I am bleeding. I am scheduled for an US. The GYN feels another polyp or re growth has probably occurred. In reading up on articles, it appears high estrogen levels might contribute to the development of uterine polyps. I am overweight and am treated successfully for HTN. Recently, I started actively doing exercise and watching my fat and caloric intake. I have lost 7 lbs in just over three weeks. Are estrogen levels high because I am heavy or is this part of being post menopausal? I am 68, stopped menses around age 50. I am curious if I can help myself with polyp reoccurrence or not. Are high estrogen levels needing/or can they even be reduced, if the cause for polyps or does weight etc enhance increased estrogen in of itself. I was always small-some thought I looked too thin and I ate robustly. Once I got passed menopause I have struggled gaining more each year. I have yoyo’ed with dieting, so am hoping this time I can prevail.
ReplyHi Margaret- thanks for posting to my blog about endometrial polyp over-diagnosis.
thanks
David Emerson
ReplyFollowing a post – link doesn’t work to: http://www.peoplebeatingcancer.org/forums/topic/endometria-polyps-questions-and-answers/
ReplyHi Denise-
I apologize for not removing the link sooner. The forum was discontinued due to lack of participation. I have removed the link. Thank you for pointing this out to me.
Do you have any questions about endometrial/uterine polyps?
thank you
David Emerson
ReplyI am diagnosed of endometrial polyps last 2014 and stop at 2015,at this time seems occurred because i have heavy menstrual bleeding and irregular periods,in this regards hope you advised me for good threatening,thank u
ReplyHi Evelyn-
I am not clear about what you are asking. I am a cancer coach. If you have gynalogical questions you should talk to a medical doctor.
David Emerson
ReplyI’m ronique in 23 years old nd have been told that my body produces polyps . I have had 3 or 4 hysteroscopy especially nd need one now but my doctor is concerned because of my young age a day the rapid re-occurence of the polps. help me the pain is paralyzing. he put me on depo in hope of it taking care of the problem instead of surgery
ReplyHi Ronique-
I am sorry to read of your recurring polyps. Please consider supplementation in the studies below shown to both shrink polyps and to reduce the risk of polyps coming back.
David Emerson
ReplyMy name is Vanessa. I am sure I have these polyps. I have passed two over the course of the last year. The bleeding in-between periods have increased to the point where I am losing so much blood every month I am now anemic. I am consistently tired and weak. My hormone’s are up and down so much I feel bipolar most of the time. I do not have access to health insurance and have been told by a gynecologist that it is probably a sign of premenopaus but as I started looking into this more, I have found that it could be a sign of cancer. I am 32 years old but early menopause runs in my family, usually triggered by a hysterectomy but typical women in my family will enter in their 30’s without the hysterectomy. Multiple types.of female cancer also runs in my family, All the women on my mothers side has has some form of cancer that invaded their reproductive systems. My question has two parts, the first being does the fact female cancers run in my famil, do I have a much higher risk of my polyps being cancerous than a regular woman and if so, since I am done having children, should I just get a hysterectomy?? Or should I just have a hysterectomy to help even out my hormones? I don’t know what to do or the cost associated with any procedures.
ReplyHi Venessa-
I am sorry to read of your health challenges. I gather from your email that though you are experiencing symptoms and believe that you have polyps, you have not seen a doctor. I will try to provide information below but I recommend that you see an OBGYN.
First of all, the study linked and excerpted in the blog post that you read indicates that PRE-menopausal women such as yourself have less of a risk of malignant end polyps. Further, the study found that the risk of cancerous polyps on average was 2.5%. I have excerpted the study’s findings regarding endo polyps below.
To address your questions- “My question has two parts, the first being does the fact female cancers run in my famil, do I have a much higher risk of my polyps being cancerous than a regular woman…” There is no mention in the study of any link between genes and malignant endo polyps.
Also, “…and if so, since I am done having children, should I just get a hysterectomy??” This is the kind of question that you and your OBGYN should discuss. There are risks and benefits to having a hysterectomy. You should talk to a professional to be able to weigh these pros and cons. Likewise is the answer to your question about hormones and the cost of this procedure. Please talk to a medical doctor.
“To summarize: If you are diagnosed with endometrial polyps:
1) 13.7% of the time the polyps resolve on their own-
2) 41.7% of the time the polyp size stays the same-
3) 20.3% of the time the polyps shrinks at least 1mm-
4) 16.3% + 8.0% of the time the polyps grow at least 50% larger”
Let me know if you have any other questions. Good luck and hang in there.
David Emerson
ReplyI was a little blown away by your post…My name is also Vanessa and a year ago, I had several uterine polyps removed. At the time, I thought I was just going through menopause and had spent the previous two years dealing with periods that were getting heavier and heavier. The last year before surgery, I was bleeding 30 out of every 40 days…When I was finally able to get onto Washington Health Care, they discovered/removed the polyps, gave me 50,000 units of vitamin D for 4 weeks, had shots of B-12 in my ass and took iron because of anemia. BLEEDING STOPPED IMMEDIATELY! No periods or spotting for 8 months…then a little period…then another…and now…I have had 3 heavy periods in 6 weeks…I am sure the polyps have returned…Oklahoma is not conducive to my health…I am not eligible for sooner care(no kids) not eligible for medicare(only 51) and was told I don’t make enough money to qualify for a tax credit with Obama Care(They told me to call later and lie about income to receive a tax credit.) I am currently trying to figure out how to get medical care in this God forsaken state and I’m not going to lie…I am worried about this being bad! If my last lead on a free clinic doesn’t work out, at least I have…Well, not my health…
ReplyBack in 1999 my Dr found cancer cells in my uterus, after having four daughters and two miscarriages, it is now 2007, I found another Dr. By this time I’m in stage 4. He said six more month I would have had full blown cancer. What legal action right do I have? They only gave me a hysterectomy because by the time I had my last child I had private insurance. Before then was Medicade so the state didn’t want to help me.
ReplyHi Crystal-
In response to your question “What legal action right do I have?” I am a cancer survivor and cancer coach. I am not qualified to offer an answer to your question.
Good luck.
David Emerson
ReplyHello! My name is Veronica and my doctor told me I had a polyp because I was complaining about spotting during/after intercourse. I want to know if I should get the D&C or try and let it dissolve on its own. Or by chance could it be something else because she really didn’t really get into it. Just told me I had a polyp and to get it removed, no information that would be helpful whatsoever
ReplyHi Veronica-
I’m not experienced enough to advise you about your therapies for a uterine polyp. I wrote about endometrial polyps being overtreated because of the study that I excerpted and quoted below. I am a cancer survivor who believes that less treatment is often better. To enhance the chance that your polyp will resolve on it’s own I can send you studies about antioxidant supplementation.
Let me know. Thanks and hang in there,
To summarize: If you are diagnosed with endometrial polyps:
1) 13.7% of the time the polyps resolve on their own-
2) 41.7% of the time the polyp size stays the same-
3) 20.3% of the time the polyps shrinks at least 1mm-
4) 16.3% + 8.0% of the time the polyps grow at least 50% larger
David Emerson
ReplyHi. I’m 43 years old. A year ago at inspection at me have found out a polyp endometrium 6.3mm one. At the same time nothing disturbed me.I have not experienced bleeding. The doctor offered to remove. But I refused. And every 3 months was examined. Yesterday, at the next examination the doctor found 3 polyps, the largest of which is the size of 2mm. My question is: how one polyp of 6.3 mm could turn into three small? And whether it is necessary remove these polyps? Are the chances of endometrial polyps becoming cancer?
ReplyHi Arzu-
I am a cancer coach. I am not qualified to answer your question. I am sorry I can’t be more help.
David Emerson
ReplyMargaret, I too had high estrogen levels. I have cut out most chemicals that we’re surrounded with (shampoo, soap, makeup, cleaning supplies). I make my own laundry soap, use vinegar for the rinse instead of fabric softener (w/3 wool balls in the dryer), use glycerin bar soap for the shower, and healthy hand soap. I also apply Progessence Essential Oil to my neck 3x/wk. I had applied it nightly for 4 months before my polyp was removed. I noticed a huge difference in my estrogen level as my breasts used to be dense and they weren’t after a month of doing this nightly. I will continue keeping the chemicals as much as I can out of my life, and so out of my system. Read up on it.
Reply