Diagnosed with Cancer? Your two greatest challenges are understanding cancer and understanding possible side effects from chemo and radiation. Knowledge is Power!
Learn about conventional, complementary, and integrative therapies.
Dealing with treatment side effects? Learn about evidence-based therapies to alleviate your symptoms.
Click the orange button to the right to learn more.
Rethinking “Cancer”

What do I mean when I propose the idea of “Rethinking Cancer?” I’ve spent years researching and writing about the term that I understand and have lived every aspect of it. In the case discussed in the essay linked below, Laura J. Esserman, MD, MBA and Scott Eggener, MD discuss a specific issue that is caused by several types and stages of cancer. Or really, several types of pre-cancer.
The term cancer is as much about what is going on IN your body as anything. And for those diagnoses of cancer that are
- stage 0 or
- in-situ
the word cancer is essentially meaningless. Melanoma stage 0 simply means that the patient has melanoma that will not do anything. And certainly will not cause any damage.
What types of cancer are over-diagnosed?
Several types of cancer are known to be associated with overdiagnosis, often due to widespread screening programs. Some of these include:
- Prostate Cancer: Screening with prostate-specific antigen (PSA) tests can lead to the detection of slow-growing tumors that may never cause symptoms or harm during a person’s lifetime.
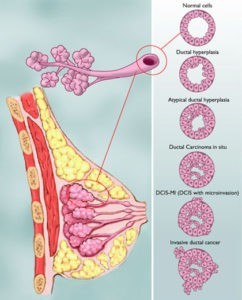
- Breast Cancer: Mammography screening can detect early-stage breast cancers, including ductal carcinoma in situ (DCIS), which may never progress to invasive cancer or cause harm.
- Thyroid Cancer: Increased use of imaging tests like ultrasound has led to the detection of small thyroid nodules, many of which are slow-growing and may never cause symptoms or harm if left untreated.
- Lung Cancer: Screening with low-dose computed tomography (CT) scans can detect early-stage lung cancers, but some of these may be slow-growing and would not have caused symptoms or harm if left undetected.
- Kidney Cancer: Incidental detection of small renal masses has increased with the use of imaging tests like CT scans, leading to the diagnosis of cancers that may not have caused harm if left untreated.
To look at the idea of stage 0 or in-situ cancer from a treatment standpoint, all I can say is that no treatment is needed. Yes, ductal carcinoma in-situ is usually surgically removed, but it doesn’t have to be.
If the patient does treat his/her cancer stage 0 then they risk side effects from the unnecessary treatment.
Have you been diagnosed with stage 0 or a types of in-situ cancer? Let me know if you’d like to learn more about evidence-based non-conventional therapies- David.PeopleBeatingCancer@gmail.com
Thank you,
David Emerson
- Cancer Survivor
- Cancer Coach
- Director PeopleBeatingCancer
Epidemic of overdiagnosis and overtreatment’ prompts calls to redefine cancer
“Momentous strides have been made in the understanding of disease biology for many cancer types.
However, these advances are not always reflected in the way cancer is defined and treated, according to some leaders in the field.
For example, certain diseases — such as ductal carcinoma in situ (DCIS) and low-grade prostate cancer — pose minimal risks for mortality or diminished quality of life, and they do not necessitate intense treatment that can potentially result in physical pain or disfigurement, psychosocial distress or financial burdens.
In a New York Times guest essay published last summer, Laura J. Esserman, MD, MBA, a surgeon and breast cancer specialist at UCSF Helen Diller Family Comprehensive Cancer Center, and Scott Eggener, MD, a professor of surgery and prostate cancer specialist at The University of Chicago Medicine, outlined the case for reconsidering the way cancer should be defined in its earliest stages.
In the essay, they described how a DCIS diagnosis or a biopsy revealing Gleason score 6 (Grade Group 1) prostate cancer have extremely low risks for causing symptoms or metastases, as both signify the earliest noninvasive stage of disease. Both “are more accurately explained as risk factors for prostate or breast cancers with malignant potential,” Esserman and Eggener wrote.
“As physicians, our job is to do no harm,” Esserman, director of the UCSF Breast Care Center, told Healio. “There are certain ‘cancers’ that we do not have to be so aggressive about treating.”
When people hear the word “cancer” they often become frightened, Esserman added, sometimes leading to a mindset that major surgery or extensive treatment is necessary.
This is not always the best choice, she argued, noting alternatives may exist.
“We can treat patients with stage III to stage IV ER-positive disease with endocrine therapy for 6 months, and we certainly can do the same for patients with DCIS. I’ve done it for years,” Esserman said. “Every woman has a chance to figure out more about her disease biology, discover whether there are any clinical trials for her, look for treatment alternatives and find out what is best for her.”
Healio spoke with oncology experts about the reasoning behind rethinking what the medical field calls cancer and the implications — both positive and negative — if this viewpoint becomes widely embraced in the clinical community.
Rethinking ‘cancer’
Experts first began diagnosing DCIS during the 1990s when the disease molecularly appeared the same as breast cancer and clinicians treated it as such.
In the early 2000s, Esserman and colleagues began searching through old databases that included data on patients on active surveillance for cancer.
“We found that among those with fast-growing cancers, those individuals were no longer at risk at 5 years from diagnosis, and for those with slow-growing cancers, they required 15 to 20 years of follow-up,” she said.
Those observations led Esserman and colleagues to publish a paper in JAMA in 2009 about rethinking what is called “cancer.”
Esserman and her co-authors made several observations defending their viewpoint. Among them: Incidence of breast and prostate cancers increased after introduction of screening and had not returned to prescreening levels; the increase in the relative fraction of early-stage cancers had increased; and incidence of regional cancers had not decreased at a commensurate rate.
“One possible explanation is that screening may be increasing the burden of low-risk cancers without significantly reducing the burden of more aggressively growing cancers and, therefore, not resulting in the anticipated reduction in cancer mortality,” they wrote. “To reduce morbidity and mortality from prostate cancer and breast cancer, new approaches for screening, early detection and prevention for both diseases should be considered.”
DCIS can be considered a “window of opportunity” for prevention and not necessarily a disease that requires surgery, Esserman said.
“Over the years, many of my patients have come to me after reading the latest literature on DCIS and said that they don’t want to undergo surgery but want to wait instead,” she said. “That is what led me to put an imaging protocol together with my colleague, Nola Hylton, PhD, and, lo and behold, what we have found over time is that certain patients are good candidates for less harsh treatment. For hormone receptor-positive DCIS, we can give some patients the option of 6 months of endocrine therapy and determine who is a candidate for active surveillance and who has a residual focal lesion better treated with surgical excision. With this framework, we can see whether we can improve upon the tolerability and efficacy of the standard endocrine treatments that we have.”
This observation led to the development of the phase 2 RECAST DCIS study to assess alternative treatments for DCIS. The study is accruing patients, with the plan to enroll more than 300 participants across 40 U.S. sites.
“In the past, cervical carcinoma in situ was changed to cervical intraepithelial neoplasia because of the concern that women were undergoing unnecessary hysterectomies while still of childbearing age,” Esserman said.
“Nothing can be more harmful to a woman who still wants to have children than to feel like they had to undergo this procedure unnecessarily. It is a signal to both physicians and patients to ‘put the brakes’ on treatment for other diseases, as well,” she added. “Patients don’t have to be committed to immediately deciding on what to do for treatment, even for the more significantly immune-driven DCIS cases. We have also developed immune-targeted intratumoral injections and have a phase 1 study that is very promising.”
A ‘controversial’ topic
Eggener recalled thinking about the concept of redefining what the medical community defines as cancer more than a decade ago.
“It was a topic only shared with close physician friends over drinks because it was so controversial,” he told Healio. “Fast forward years later, and many people have now published on the topic.”
In a commentary published in 2022 in Journal of Clinical Oncology, Eggener and colleagues proposed a simple terminology change for low-grade prostate cancer lesions and removal of the “cancer label” — a move they argued could significantly reduce overdiagnosis and overtreatment, as well as alter the cost-benefit ratio of screening for many patients.
“From a macro viewpoint, there’s an epidemic of overdiagnosis and overtreatment,” Eggener said. “Since the creation of the PSA blood test, every study and model has shown that for every patient we diagnose, treat and save their life, there are way more men that we’re torturing with unnecessary treatments.
“Just because we’ve always called it cancer doesn’t mean we need to continue to do so,” he added. “For example, Gleason 6 prostate cancer is an entity that does not cause problems and is literally incapable of spreading to other parts of the body or causing issues. That is why we are pushing the concept of rethinking what we call cancer. In some of the things we’ve written about, we literally take definitions out of the dictionary of what benign and malignant mean. By those definitions, Gleason 6 fits the definition of something that is benign.”
There are multiple potential benefits of re-evaluating how certain conditions are characterized, Eggener said.
“If we were to rethink what we call cancer, the effects could be profound and overwhelmingly positive,” Eggener said. “We could have a ton more men who do not undergo unnecessary treatment and, consequently, fewer men living with the side effects of that treatment. There could be less stress and anxiety over a cancer diagnosis that has such an extraordinarily low likelihood of causing problems down the line. There would also be easier access to life insurance and probably other beneficial aspects that we haven’t even thought about yet.”
Unnecessarily labeling certain conditions as cancer can lead to financial strain for patients, Eggener said.
“Many patients are unable to renew their life insurance or their prices for life insurance increase considerably, even though the prognosis for early-stage prostate cancer literally does not increase the likelihood of them dying,” Eggener said.
Financial considerations inadvertently play a role in redefining what is labeled cancer, he added.
“Most would agree that billable procedures play a part in all of this, but no one really wants to talk about it or address it. [This] is true for most of the American health care system, which is highly flawed,” he said.
“There is an element of fee for service and doing more procedures or prescribing more treatment because of it,” Eggener added. “Some people do it overtly and criminally, and many people do it subconsciously. For others, it’s a nonfactor, but it’s absolutely ‘baked’ into the system.”
Concept flaws
Although many experts agree with the idea of renaming certain conditions considered “cancer,” others express concern about the consequences of such a change.
“The concept that we do not need to treat these patients aggressively is totally valid, but changing the designation will alter the way we manage these patients,” Adam S. Kibel, MD, chair of the department of urology at Brigham and Women’s Hospital, told Healio. “If we tell patients that they don’t have cancer, they may not adhere to follow-up recommendations….”
Kibel and Epstein went on to say that there has been greater acceptance of active surveillance for Gleason score 6 prostate cancer. The underlying clinical conundrum of renaming is how to identify indolent tumors with reasonable certainty and, therefore, how the renaming will alter disease management.
Any change in nomenclature should have no effect on how the disease is managed, he added. Some patients with Gleason 6 prostate cancer still will require treatment and serial biopsies will be required to maintain active surveillance of the disease, he noted.
“Many patients with prostate cancer are overtreated and there is a need to demystify the disease,” Kibel said. “We give people a very scary diagnosis and so anything that we can do to demystify that is very valid and a good idea. However, there is a concern that patients are going to suffer as a result because they are not going to be treated correctly.”