Recently Diagnosed or Relapsed? Stop Looking For a Miracle Cure, and Use Evidence-Based Therapies To Enhance Your Treatment and Prolong Your Remission
Multiple Myeloma an incurable disease, but I have spent the last 25 years in remission using a blend of conventional oncology and evidence-based nutrition, supplementation, and lifestyle therapies from peer-reviewed studies that your oncologist probably hasn't told you about.
Click the orange button to the right to learn more about what you can start doing today.
- You are here:
- Home »
- Blog »
- Multiple Myeloma »
- Diagnosed w’ Non-hodgkin lymphoma followed by Multiple Myeloma
Diagnosed w’ Non-hodgkin lymphoma followed by Multiple Myeloma
“It is possible that cytotoxic treatment per se may promote transformation10)”. Suffice to say that you have been through the blood cancer wringer. And lived to talk about it. I am impressed.
Hi David- In 2010 I was diagnosed with non-hodgkin lymphoma followed by multiple myeloma years later.
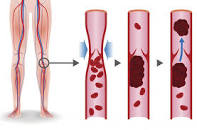
I presented with a football sized tumor in pelvis and a deep-vein thrombosis (blood clot) in my leg. The DVT traveled to to my lung.
I underwent a chemotherapy cocktail called “r-chop,” and had 25 rounds of radiation (turned out the 1/2 r chop was raised to full r-chop (Adriamycin aka red devil).
This was NHL, stage 2. My side effects following this therapy included psoriasis, shingles, others.
My oncologist thinks that I may have monoclonal gammopathy of undermined significance (mgus) or smoldering MM. He wants me to see a MM specialist again with 24 hr urine test and fat pad test for amyloidosis.
- MM Survivor
- MM Coach
- Director PeopleBeatingCancer
Recommended Reading:
- Multiple Myeloma Diet- Before, During, After Therapy
- MGUS Diagnosis- I Want to Reduce Risk Without Chemo
A Case of Coincident Multiple Myeloma and Non-Hodgkin’s Lymphoma
“Multiple myeloma (MM) is the major malignancy of plasma cells. Patients with MM can present with a variable spectrum of clinical features and different stages of the disease7).
MM is a disease in which approximately 99% of patients have a monoclonal protein in the serum and/or urine. This has led to the prevailing concept that myeloma is monoclonal at the cellular level6).
Although lymphomas are usually neoplasms of lymphatic tissues, substantial numbers of non-Hodgkin’s lymphoma arise in other tissue. Bone marrow biopsy may be diagnostic in patients without peripheral lymphadenopathy. Bartl et. al. found the incidence of bone marrow involvement in approximately 65% of non-Hodgkin’s lymphomas (NHL) at the time of diagnosis8).
In this case, the patient fulfilled criteria for MM with IgA lambda monoclonal gammopathy and bone marrow plasmacytosis7). In the bone marrow biopsy, there were localized collection of malignant lymphocytes in addition to the malignant plasma cells. Mesenteric lymph node biopsy revealed NHL.
The occurrence of both MM and NHL in our patient implies several possible pathogenetic mechanisms.
First, one malignant disease may evolve from anthor. The malignant B cell lymphoma clone may mature giving rise to MM. A comparison of the immunologic phenotype of both MM and NHL in a patient is needed to reach meaningful conclusions.
In our patient, where monoclonal Ig synthesized by both cell types had the same type of light chains, we performed a study with anti-idiotype reagents; idiotypic determinants expressed by serum and intracellular plasmacytic Ig were detectable on the surface Ig of lymphoma cells.
These findings suggest the possibility that the lymphoma cells transformed into plasma cells. On the other hand, the development of high grade malignant lymphoma in patient with chronic lymphocytic leukemia was first reported by Richter in 1928 and transformation to high grade lymphoma is now a well-known event in other low grade malignancies of the B cell lineage9).
The malignant transformation of MM has rarely been reported. During the last decade, patients with advanced MM survive longer due to intensified chemotherapy and improved supportive care. This increased survival has permitted the development and improved the chance of observing transformation of MM to high grade malignant lymphoma.
It is possible that cytotoxic treatment per se may promote transformation10). Another possible mechanism is that both malignancies are different manifestation of original neoplastic clone.
In 1982, Bryant et. al., reported plasma cell myeloma in a patient with a cutaneous T-cell lymphoma3).
In 1986, Gran et. al., described a patient with coincident MM and NHL with 2 serum monoclonal immunoglobulin2). They suggest that the rare association of two diseases represents different manifestations of a unique clonal disorder which affects the B cell precursor. Although it would be rare, a possibility of independent of two infrequent malignancies at one time exists.
In terms of patient management, treatment must be directed to the more life-threatening condition. In our case, lymphoma was a more serious condition because of intestinal bleeding.
This case offers additional support to the theory of malignant transformation of MM and NHL. Opportunities to study and understand the unique natural history and evolutional dynamics for this transformation are rare. We would recommend further multicenter comparisons of slimilar cases in a broad effort to better define this complicated disease process.