
Recently Diagnosed or Relapsed? Stop Looking For a Miracle Cure, and Use Evidence-Based Therapies To Enhance Your Treatment and Prolong Your Remission
Multiple Myeloma an incurable disease, but I have spent the last 25 years in remission using a blend of conventional oncology and evidence-based nutrition, supplementation, and lifestyle therapies from peer-reviewed studies that your oncologist probably hasn't told you about.
Click the orange button to the right to learn more about what you can start doing today.
- You are here:
- Home »
- Blog »
- Multiple Myeloma »
- Multiple Myeloma Therapy- Bisphosponate Risks- Zometa, Aredia, etc.
Multiple Myeloma Therapy- Bisphosponate Risks- Zometa, Aredia, etc.
“Here, we focus on the current guidelines for the use of BPs in MM and address side effects such as renal toxicity, osteonecrosis of the jaw, and low-energy fractures.”
If you’ve been diagnosed with multiple myeloma, chances are your oncologist will include bisphosphonates in your regimen as a multiple myeloma therapy. Bisphosphonates such as Zometa and Aredia are “standard-of-care” for newly diagnosed MM.
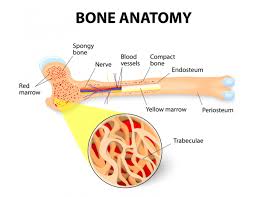
Bisphosphonate therapy has been shown to harden bones thereby reducing the risk of SRE (skeletal-related events-pathological fractures) in NDMM.By reducing your risk of fractures, you will live longer (longer overall survival).
Bisphosphonate therapy was included in my induction therapy when I was diagnosed with MM in early 1994. As a NDMM patient, you lifelong challenge is to maintain your bone health (bone mineral density) and reduce the risk of bone fractures.
The challenge to NDMM patients is that bisphosphonate therapy can cause several different adverse events aka side effects. Specifically:
- Renal Damage
- Osteo-necrosis of the Jaw (ONJ)
- Low-energy Fractures
If you are a NDMM with renal/kidney damage at diagnosis, consider denosumab instead of a bisphosphonate therapy. Beware that denosumab is much more expensive than Bisphosphonate therapy and make sure that your health insurance will cover it.
Both Bisphosphonates as well as Denosumab have been shown to increase the risk of ONJ. Talk to your oncologist of course, and consider undergoing bone strengthening drugs for months rather than years.
Like all conventional multiple myeloma therapy, MM patients must weigh the risks and benefits of taking the drug, how long, what does, etc.
If you have been diagnosed with multiple myeloma always remember that there are a host of non-toxic therapies that have been researched and shown to enhance bone mineral density aka bone health.
- Exercise (weight-bearing)
- Supplementation (vitamin D3, others)
- Nutrition (green leafy veggies, others)
All have been shown to strengthen our bones. While FDA approved therapies such as Bisphosphonates and Denosumab may be a short-term fix, I believe that our long-term solutions come in the form of evidence-based, non-toxic therapies.
To Learn More About Kidney Failure in Multiple Myeloma click now
Let me know if you have any questions or comments.
Thank you,
David Emerson
- MM Survivor
- MM Cancer Coach
- Director Galen Foundation
Multiple Myeloma Symptom, Side Effect, Cause of Death
Recommended Reading:
- Long-Term Multiple Myeloma Survivor- If I Knew Then What I Know Now
- Multiple Myeloma Survivor- Relapse w/ Kidney Involvement-
- Multiple Myeloma Side Effect- Osteonecrosis of the Jaw-
What to make of the new warning on bisphosphonates
“In October 2010, the FDA issued a warning that long-term use of bisphosphonates — the class of drugs most widely prescribed for preventing and treating osteoporosis — may increase the risk of unusual fractures of the thigh. Reports of these fractures began to emerge in 2007.
The bone breaks involved occur just below the hip joint (subtrochanteric) and in the long part of the thighbone (diaphyseal). They generally happen with little or no trauma and, in some cases, have occurred in both femurs. About half the time, patients notice pain or weakness in the affected thigh for weeks to months before the break. These fractures are atypical and rare, accounting for less than 1% of all osteoporotic hip and thigh fractures. So far, there is no way of telling in advance who is most vulnerable…
The Role of Bisphosphonates in Multiple Myeloma: Mechanisms, Side Effects, and the Future
“Zoledronic acid and pamidronate are two potent anticatabolic nitrogen-containing bisphosphonates (BPs) used extensively in diseases with high bone turnover such as multiple myeloma (MM).
In this review we focus on their biology and their current and future use in MM, and highlight some of the most common and emerging side effects.
Although the primary target cells for BPs are osteoclasts, new insights suggest other cell types of the bone microenvironment as possible targets, including osteoblasts, endothelial cells, immune cells, and cancer cells. Here, we focus on the current guidelines for the use of BPs in MM and address side effects such as renal toxicity, osteonecrosis of the jaw, and low-energy fractures.
Prevention Of Skeletal Related Events In Multiple Myeloma: Focus On The RANK-L Pathway In The Treatment Of Multiple Myeloma
“More than 90% of patients with multiple myeloma (MM) have osteolytic bone lesions which increase the risk of skeletal-related events (SRE). The cytokine milieu in the bone marrow microenvironment (BMME) of MM plays a key role in myeloma bone disease by impairing the balance between osteoclastogenesis and osteoblastogenesis…
Prevention of SRE is currently accomplished by the inhibition of osteoclasts. Bisphosphonates (BPs) are pyrophosphate analogues that cause apoptosis of osteoclasts and have been proven to prevent and delay SRE.
Denosumab, a fully humanized monoclonal antibody that binds and inhibits receptor activator of nuclear factor-ĸB ligand (RANKL), a key molecule in the BMME crucial for osteoclastogenesis, is also approved for the prevention of SRE in MM. The addition of BPs and denosumab to standard MM treatment affords a survival benefit for patients with MM…”
Caution Urged When Considering Denosumab in Patients With Multiple Myeloma Who Have Normal Renal Function
“Of note, while bisphosphonates, which are eliminated through the kidneys, are not recommended in patients with severe renal dysfunction given their association with renal toxicity,4 the pharmacokinetics and pharmacodynamics of denosumab are not affected by kidney function, although hypocalcemia has been reported in some patients with renal impairment receiving denosumab without adequate calcium supplementation.2…
The study authors commented that routine use of denosumab in patients with multiple myeloma “is difficult to justify except in patients with renal dysfunction or in those unable to tolerate bisphosphonates” given the increased expense and more frequent dosing of denosumab compared with bisphosphonate therapy, as well as the rapid bone loss associated with the discontinuation of denosumab.1
In their concluding remarks, the study authors stated that “further research should examine the role of rebates and reimbursements as incentives for the widespread adoption of more costly drugs that have not demonstrated superiority.”1″

