
Recently Diagnosed or Relapsed? Stop Looking For a Miracle Cure, and Use Evidence-Based Therapies To Enhance Your Treatment and Prolong Your Remission
Multiple Myeloma an incurable disease, but I have spent the last 25 years in remission using a blend of conventional oncology and evidence-based nutrition, supplementation, and lifestyle therapies from peer-reviewed studies that your oncologist probably hasn't told you about.
Click the orange button to the right to learn more about what you can start doing today.
- You are here:
- Home »
- Blog »
- Multiple Myeloma »
- Circulating Tumor Cells- Myeloma
Circulating Tumor Cells- Myeloma
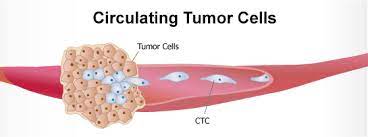
“Circulating tumor cell (CTC) levels can be used to risk-stratify patients with newly diagnosed, transplant-eligible multiple myeloma (MM), according to researchers.”
Circulating tumor cells (CTC), according to the research linked below, can indicate shorter or longer progression-free survival. Circulating tumor cells can indicate the newly diagnosed MM patient’s stage as well.
When you were first diagnosed with multiple myeloma, what if:
- Your CTC at diagnosis, could tell you that you would achieve an “exceptional progression-free survival, regardless of how you responded to your induction therapy?
- Your CTC at diagnosis, could tell you your overall survival (length of life)?
To a large extent, MM is about determining risk. The first challenge that we face is being told that we have an incurable cancer. Incurable but treatable, we are told.
Unfortunately, incurable but treatable doesn’t tell us anything about our risks.
Eventually, MM patients figure out that there is little information available to us to tell us how long we are going to live.
NDMM patients can be diagnosed with a high percentage of plasma cells in their marrow, say 90%, an still achieve complete remission and therefore potentially achieve a long PFS.
Many of us go to online groups to debate the pros and cons of different chemo cocktails or an ASCT, but we do this all in an effort to achieve the longest PFS and OS.
Achieving MRD negative status is a positive indicator of long PFS and OS but there is still considerable risk of relapse…
Regardless of our stage at diagnosis (I,II,III), we all are prescribed the same standard-of-care therapy plan. It’s as if oncology relies on “potentially curative” therapies regardless of diagnostic or staging information.
Identifying CTC’s in the patient’s peripheral blood can change that. For example, if you had “no points” at diagnosis. You may choose to undergo low-dose therapy or a short course (1,2 cycles) of D-RVd.
Conversely, if you had “3 points or higher” at diagnosis, you could hit the gas. Meaning, you could be more confident in multiple cycles of D-RVd, an autologous stem cell transplant and low-dose maintenance therapy.
If you are newly diagnosed with MM, are early stage and have 0 or a low percentage of CTC, it seems to me that you future as a MM survivor looks pretty bright.
Am I reading the study below correctly or not? Let me know.
Thank you,
David Emerson
- MM Survivor
- MM Cancer Coach
- Director PeopleBeatingCancer
Recommended Reading:
- Multiple Myeloma Chemotherapy, Allergy, Hypersensitivity, Side Effects?
- Relapsed, Refractory Multiple Myeloma- Therapy Options
- Multiple Myeloma-10 Mind-Body Cancer Therapies Better than Chemo-
Measuring Circulating Tumor Cells at Diagnosis Can Improve Risk Stratification in Multiple Myeloma
“Circulating tumor cell (CTC) levels can be used to risk-stratify patients with newly diagnosed, transplant-eligible multiple myeloma (MM), according to researchers.
They found that CTC levels were an independent predictor of progression-free survival (PFS) and overall survival (OS) in this patient population. When the researchers considered CTC levels in conjunction with other prognostic factors, they were able to improve risk stratification…
The study included 374 patients with newly diagnosed MM who participated in the GEM2012MENO265 and GEM2014MAIN trials (ClinicalTrials.gov Identifiers: NCT01916252 and NCT02406144). The researchers looked at CTCs in the peripheral blood as well as minimal residual disease (MRD) in bone marrow aspirates.
CTCs were detected in 92% of patients (344/374). In this group, the median percentage of CTCs was 0.017% (range, 0.0002%-16%) or 1 CTC/μL …
The researchers noted a “modest correlation” between CTC levels in the peripheral blood and plasma cells in the bone marrow by morphology and flow cytometry. However, only CTC levels were an independent predictor of PFS and OS.
The percentage of plasma cells in the bone marrow was not significantly associated with PFS. or OS. The percentage of CTCs in the peripheral blood was significantly associated with both PFS and OS.
- The researchers also found that a CTC threshold of 0.01% was an independent predictor of PFS.
- The researchers noted that patients with undetectable CTC levels had “exceptional” PFS, regardless of their MRD status or whether they achieved a complete remission.
- For patients who had detectable CTCs, MRD negativity was associated with improved PFS.
To confirm the prognostic utility of CTCs (at 0.01% or higher), the researchers incorporated this factor into a staging system that included the following other factors: albumin less than 3.5 g/dL, β2-microglobulin greater than or equal to 5.5 mg/L, elevated lactate dehydrogenase, and high-risk cytogenetics. Each risk factor was assigned 1 point.
Patients with higher scores were found to have worse PFS and OS. The median PFS was not reached for patients with no points, 73 months for patients with 1-2 points, and 32 months for patients with 3 or more points.
- The 5-year OS rate was 88% for patients with no points,
- 85% for those with 1-2 points,
- and 57% for patients with a score of 3 or higher.
“Our data support the inclusion of CTCs into the list of laboratory examinations in peripheral blood at diagnosis and urge considering its utility to enhance the current stratifying systems for patients with newly diagnosed, transplant-eligible MM,” the researchers wrote.
Disclosures: Some study authors declared affiliations with biotech, pharmaceutical, and/or device companies. Please see the original reference for a full list of disclosures.
Reference
Garcés J-J, Cedena M-T, Puig N, et al. Circulating tumor cells for the staging of patients with newly diagnosed transplant-eligible multiple myeloma. J Clin Oncol. Published online June 6, 2022. doi:10.1200/JCO.21.01365
How Useful Are Circulating Tumor Cells for Early Diagnosis?
“Liquid vs Tissue- Liquid biopsy is a minimally invasive tool that is easy to use. It is employed to detect cancer, to assess treatment response, or to monitor disease progression. Liquid biopsy produces test material from primary and metastatic (or micrometastatic) sites and provides a more heterogeneous picture of the entire tumor cell population, compared with specimens obtained with tissue biopsy…”


