Recently Diagnosed or Relapsed? Stop Looking For a Miracle Cure, and Use Evidence-Based Therapies To Enhance Your Treatment and Prolong Your Remission
Multiple Myeloma an incurable disease, but I have spent the last 25 years in remission using a blend of conventional oncology and evidence-based nutrition, supplementation, and lifestyle therapies from peer-reviewed studies that your oncologist probably hasn't told you about.
Click the orange button to the right to learn more about what you can start doing today.
- You are here:
- Home »
- Blog »
- Multiple Myeloma »
- ASCT- Permanent Myelosuppression?
ASCT- Permanent Myelosuppression?
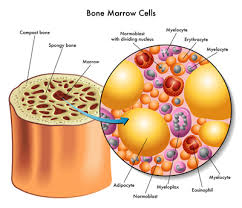
Permanent Myelosuppression caused by high-dose, aggressive treatment of an autologous stem cell transplant happens. The challenge is that it is impossible to determine how often ASCT caused permanent bone marrow damage.
If you are considering undergoing an autologous stem cell transplant, what is your risk of permanent myelosuppression? Keep reading…
I’m not talking about the temporary decreases of red, white blood cells and/or platelets that can happen with various chemotherapy regimens. Most of the time when your blood markers drop, the come back to normal.
Permanent myelosuppression, or long-lasting bone marrow damage, is a known potential complication of autologous stem cell transplantation. However, the frequency of this complication can vary widely depending on several factors:
- Underlying Condition: The type and stage of the disease being treated can influence the likelihood of myelosuppression. Some diseases, such as aggressive or advanced-stage cancers, may require more intense treatment regimens, increasing the risk of myelosuppression.
- Pre-Transplant Health: The patient’s overall health prior to the transplant can affect the likelihood of complications. Patients who are in good general health may have a lower risk of experiencing severe and permanent myelosuppression.
- Treatment Intensity: The intensity of the conditioning regimen (chemotherapy and/or radiation therapy) used before the transplant can impact the severity of myelosuppression. Higher doses of conditioning therapy are more likely to cause severe and long-lasting effects.
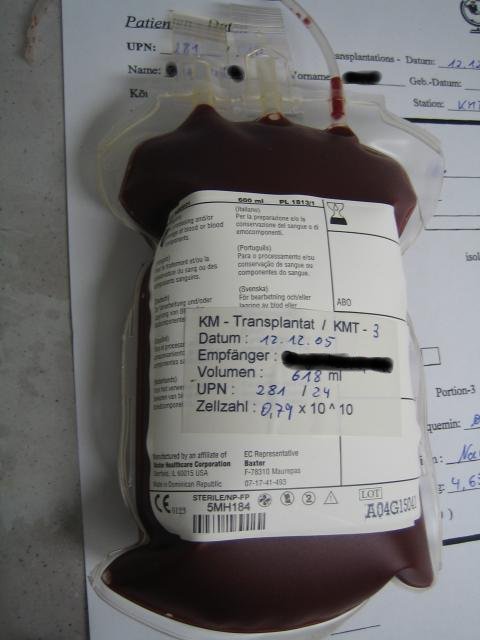
- Type of Stem Cells: The source of the stem cells can also play a role. In autologous transplants, the patient’s own cells are used, which can reduce the risk of graft-versus-host disease (a complication more commonly associated with allogeneic transplants). However, the intensity of conditioning therapy can still lead to myelosuppression.
- Age and General Health of the Patient: Older patients or those with pre-existing health conditions may be more susceptible to complications, including myelosuppression.
- Medical Team Experience: The expertise of the medical team performing the transplant can impact the overall success and safety of the procedure.
If you are struggling with myelompression consider these therapies-
To Learn More About Low Levels of bone marrow read the posts linked below
- Multiple Myeloma Chemotherapy- Low Platelets
- Myeloma- Long-term Bone Marrow Injury
- Multiple Myeloma Symptom/Side Effect-Anemia aka Fatigue
Ultimately, the specific risk of permanent myelosuppression should be discussed with the treating healthcare team, as they will be familiar with the patient’s individual medical history and condition. They can provide the most accurate and up-to-date information regarding the potential risks and benefits of autologous stem cell transplantation in any given situation.
Are you considering an autologous stem cell transplant? To learn more about Pre-Habilitation email me at
David.PeopleBeatingCancer@gmail.com
David Emerson
- MM Survivor
- MM Coach
- Director PeopleBeatingCancer
Recommended Reading:
- Diagnosed w’ Non-hodgkin lymphoma followed by Multiple Myeloma
- Multiple Myeloma Diagnosis and Staging
- Multiple Myeloma Chemotherapy- When Cancer Treatment Might Kill You
Cancer therapy-induced residual bone marrow injury-Mechanisms of induction and implication for therapy
“Bone marrow (BM) suppression is the important dose-limiting side effect of chemotherapy and radiotherapy for cancer. Although acute myelosuppression is an immediate concern for patients undergoing cancer therapy, its management has been improved significantly in recent years by the use of various hematopoietic growth factors.
However, many patients receiving chemotherapy and/or ionizing radiation (IR) also develop residual (or long-term) BM injury (a sustained decrease in HSC reserves due to an impairment in HSC self-renewal) after the recovery from acute myelosuppression.
Unlike acute myelosuppression, residual BM injury is latent and long lasting and shows little tendency for recovery.
Following additional hematopoietic stress such as subsequent cycles of consolidation cancer treatment or autologous BM transplantation, residual BM injury can deteriorate to become a hypoplastic or myelodysplastic syndrome…
Implication for cancer therapy-
The cellular responses to chemotherapy and IR include apoptosis and senescence. In a multicellular organism, these responses act synergistically to eliminate damaged cells and those that are predisposed to becoming cancerous.
However, these responses must be tightly controlled to ensure optimal survival for the organism, e.g. eliminating cells with a high risk of cancer while preserving a subset of stem cells necessary for adequate tissue repair. This is of particular importance in the maintenance of hematopoietic homeostasis since failure to eliminate damaged cells may lead to hematopoietic malignancy, while excessive cellular destruction of HPCs and HSCs will lead to acute myelosuppression and residual BM injury.
In this regard, p53 and p16Ink4a may work as a “double-edged sword” at the center of this regulation. If p53 activation is dysregulated or the cells are incapable of terminating p53 activation after DNA repair, it could be detrimental.
For example, it has been found that “super” p53 (p53+/m) mice which express a mutant but constitutively active form of p53, have a shortened life span [92]. It has been suggested that this constitutive activation gradually depletes adult tissue stem cells, leading to accelerated senescence or aging. ..”
What Factors Influence Hematological Recovery in Patients Who Receive CAR-T Therapies?
“A few weeks after receiving chimeric antigen receptor (CAR) T-cell (CAR-T) therapy, many patients experience prolonged reductions in blood cell counts, possibly making them more vulnerable to infections…
Two recent studies characterized the extent and duration of post–CAR-T cytopenia among patients receiving CAR-T therapy for hematological malignancies — with 1 study offering insights on some of the possible factors that may influence hematological count recovery…
…“recovery” being defined as reaching safe levels, and without requiring transfusions or treatment with growth factors…