
Diagnosed with Cancer? Your two greatest challenges are understanding cancer and understanding possible side effects from chemo and radiation. Knowledge is Power!
Learn about conventional, complementary, and integrative therapies.
Dealing with treatment side effects? Learn about evidence-based therapies to alleviate your symptoms.
Click the orange button to the right to learn more.
Early-stage Cervical Cancer- Hysterectomy
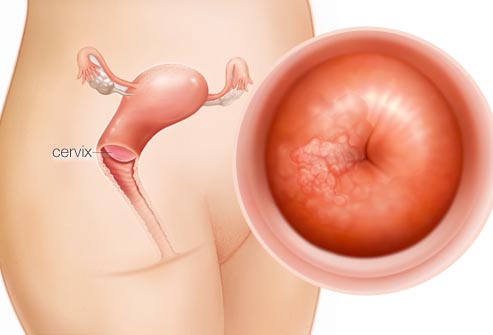
This post is trying to make two specific points for the early-stage cervical cancer patient. First, a hysterectomy may be curative. Second, it is worth your while to work with the best possible surgeon to perform your hysterectomy.
Early-stage cancers in general, are much easier to treat than cancers that have spread regionally or throughout the body. This is why surgery to remove or debulk the cancer may be curative for the cancer patient.
According to the research linked below, the early-stage cervical cancer patient won’t experience intraoperative adverse events. Probably but your risks of problems will be reduced if your surgeon is experienced, knowledgable, etc. In every industry I know of, experience matters.
What are the potential risks and benefits of a hysterectomy for the cervical cancer patient?
A hysterectomy can be a treatment option for cervical cancer, and it involves the removal of the uterus. The decision to undergo a hysterectomy involves weighing the potential risks and benefits. It’s important to note that individual circumstances may vary, and the final decision should be made in consultation with a healthcare professional. Here are some general risks and benefits associated with a hysterectomy for cervical cancer:
Benefits:
- Cure for Early-Stage Cancer: For women with early-stage cervical cancer, a hysterectomy can be curative, removing the cancerous tissue and preventing the spread of the disease.
- Improved Quality of Life: For some women, a hysterectomy may alleviate symptoms such as pelvic pain, abnormal bleeding, or discomfort associated with cervical cancer.
- Reduced Cancer Risk: Removing the uterus eliminates the risk of developing cervical cancer in the future.
Risks:
- Surgical Risks: As with any surgical procedure, there are inherent risks such as infection, bleeding, and reactions to anesthesia.
- Infertility: Hysterectomy results in the loss of fertility because it involves the removal of the uterus. If preserving fertility is a concern, alternative treatments may be explored.
- Hormonal Changes: Removal of the uterus may lead to hormonal changes, as the ovaries may or may not be removed during the procedure. This can induce menopause, with associated symptoms like hot flashes and mood swings.
- Impact on Sexual Function: Some women may experience changes in sexual function or libido after a hysterectomy. However, the impact varies from person to person.
- Psychological and Emotional Impact: Losing the ability to conceive and bear children can have emotional and psychological effects. It’s crucial to discuss these aspects with healthcare providers and seek support when needed.
- Potential Spread of Cancer: In cases where cancer has spread beyond the cervix, a hysterectomy alone may not be sufficient, and additional treatments such as radiation or chemotherapy may be required.
As both a cancer survivor and cancer coach, I have to also stress the importance of nutrition, supplementation and lifestyle therapies such as frequent, moderate exercise for the early- stage cervical cancer patient.
If you are interested in learning about other evidence-based non-conventional cervical cancer therapies, let me know- David.PeopleBeatingCancer@gmail.com
David Emerson
- Cancer Survivor
- Cancer Coach
- Director PeopleBeatingCancer
The clinical significance of intraoperative adverse events in laparoscopic radical hysterectomies for early-stage cervical cancer
Objective- Surgical quality plays a vital role in the treatment of malignant tumors. We investigated the classification of intraoperative adverse events (iAE) (ClassIntra) in relation to the surgical quality control of laparoscopic radical hysterectomies…
Results- Overall, 48 (24.6%) patients experienced 71 iAE. The iAE group was associated with significantly longer operative times (mean: 270 vs. 245 min, P < 0.001), greater blood loss (mean: 215 vs. 120 mL, P < 0.001), and longer postoperative hospital stays (median: 16 vs. 11 days). Larger tumors and poor technical performance significantly increased the risk of iAE (P < 0.05). Multivariate analysis revealed that iAE were the only independent risk factors for postoperative complications (hazard ratio, 15.100; 95% confidence interval: 4.735–48.158, P < 0.001). Moreover, patients who experienced iAE had significantly lower satisfaction scores and poorer quality of life (P < 0.05).
Conclusions- ClassIntra may serve as an effective adjunctive tool for surgical quality control in laparoscopic radical hysterectomies…
Cervical cancer is the fourth most common malignancy. It ranks fourth as the cause of death among women worldwide [1]. Surgery remains the cornerstone of early stage cervical cancer treatment [2]. Surgical outcomes, including adverse events (i.e., intra-, and post-operative complications), reflect surgical quality. Adverse events may, in turn, have an impact on survival outcomes [3, 4]. With an increase in surgical volume and the complexity of preoperative comorbidities, concerns regarding surgical adverse events have been continuously rising…
In conclusion, iAE identified by the ClassIntra grade were significantly associated with postoperative complications and recovery as well as with patient satisfaction and QOL. This grade should be routinely applied in surgical quality control and clinical decision making, particularly in future clinical trials. For the broader application of ClassIntra grade in the field of gynecologic oncology, further studies will be performed in patients with other gynecologic malignancies.”


