Recently Diagnosed or Relapsed? Stop Looking For a Miracle Cure, and Use Evidence-Based Therapies To Enhance Your Treatment and Prolong Your Remission
Multiple Myeloma an incurable disease, but I have spent the last 25 years in remission using a blend of conventional oncology and evidence-based nutrition, supplementation, and lifestyle therapies from peer-reviewed studies that your oncologist probably hasn't told you about.
Click the orange button to the right to learn more about what you can start doing today.
- You are here:
- Home »
- Blog »
- Multiple Myeloma »
- Genotoxicity- Stem Cell Transplants
Genotoxicity- Stem Cell Transplants

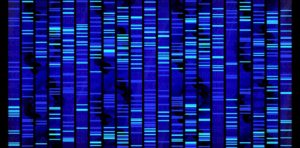
Genotoxicity is when chemotherapy causes DNA damage. Aggressive chemo aka high-dose chemo given during stem cell transplantation causes DNA damage.
Even small doses of chemotherapy and radiation both cause DNA damage. I am singling out auto/allo stem cell transplantation because of the high-dose nature of the chemotherapy administration.
The questions are two-
- What happens to cancer survivors when their DNA is damage and
- Does chemotherapy-induced DNA damage heal?
My guess is that your oncologist never told you anything about your aggressive, high-dose chemotherapy causing DNA damage. According to the study linked below published in 2018, genotoxicity had not been studied much.
According to the study linked and excerpted below, DNA damage can last for years. The main long-term challenge, according to the article, is that DNA damage increases your risk of a treatment-induced secondary cancer.
As for therapies to possibly heal genotoxicity, I will go to my usual immune enhancing non-conventional therapies:
If you are considering a stem cell transplant for multiple myeloma, my cancer, you may not be worrying about the 10-20, long-term damage caused by high dose chemotherapy. I am researching and writing this post so that you have the information. You can make the decision for yourself.
Have you already had an auto or allo stem cell transplant? Are you considering having one? Consider therapies to heal your DNA damage before, during and after your high-dose chemotherapy.
Scroll down the page, post a question or comment and I will reply ASAP.
Hang in there,
David Emerson
- Cancer Survivor
- Cancer Coach
- Director PeopleBeatingCancer
Chemotherapy-induced genotoxic damage to bone marrow cells: long-term implications
“In conclusion- significant increases in genotoxicity were seen in supportive BM cells following both in vitro and in vivo chemotherapeutic treatment. In vitro treatment at a clinically relevant dose induced genotoxicity that persisted for 48 h after treatment removal, significantly; this is later than the point at which a SCT would be administered clinically and may have important clinical implications.
Genotoxic damage to BM MSC following in vivo treatment appears to be a long-term effect, with significant damage persisting even 17 years after completion of therapy.
Clinically, genotoxic damage to the BM micro-environment may have significant impacts on haematopoiesis, including ability to support an SCT and increasing the risk of developing second primary malignancies…”
Clinical implication within the BM
For the first time, we show long-term genotoxic effects following chemotherapy in BM stromal cells. Persisting aberrations have previously been detected in other haematological cell types following chemotherapy, with increased sister chromatid exchanges seen in peripheral blood lymphocytes up to 9 months after completion of therapy for breast cancer (21,22).
Similarly, Lambert and Holmberg (51) detected chromosomal aberrations in lymphocytes from ovarian cancer patients up to 10 years later, with 14% of individuals developing second primary tumours. However, another study reported that the majority of DNA base modifications in lymphocytes were repaired within 24 h, although the study examined oxidative damage primarily (52).
Genotoxicity can also vary between tissues, with persisting chromosomal aberrations detected in rat lymphocytes for up to 20 weeks after CY treatment, whereas clastogenic effects in BM were repaired within 72 h (53). A study by Yeh et al.(4) reported cytogenetic changes in BM MSC but only in patients who were treated with both chemotherapy and radiotherapy, with no cytogenetic changes detected in patients treated with chemotherapy only.
Clinically, significant damage to the BM micro-environment may have a number of ramifications. Severe damage may result in increased apoptosis or senescence and consequently depletion of the stem cell pool. In haematopoietic stem cells, this can manifest as clonal haematopoiesis (54,55), identified as a predictor of development of second primary malignancies (56,57). Potentially, this effect could also occur in the mesenchymal compartment.
Surviving cells containing genetic lesions may also be affected functionally, which if occurring within MSC might significantly impact on haematopoiesis and ability to support a transplant. Failure to engraft occurs in up to 25% of SCTs, depending on stem cell source, conditioning regimen and recipient–donor disparity (12). GF carries a dismal prognosis, with survival remaining very low in patients who undergo a second transplant. In a large study investigating 122 patients experiencing primary GF, following a second transplant, overall 1-year survival was only 11% (58). If links between engraftment and MSC health can be further studied, it may be possible to identify individuals most at risk of MSC damage and possible GF.
Persistence of genetic aberrations/lesions can also lead to genetic instability and increased risk of developing a subsequent malignancy.
This is currently a complication in up to 15% of chemotherapy-treated individuals, with many of these malignancies arising within the BM (15,59). Analysis of damage to the marrow micro-environment may allow identification of those at greatest risk, enabling dose-stratification or treatment modification to improve outcome and quality of life.
In conclusion, significant increases in genotoxicity were seen in supportive BM cells following both in vitro and in vivo chemotherapeutic treatment. In vitro treatment at a clinically relevant dose induced genotoxicity that persisted for 48 h after treatment removal, significantly; this is later than the point at which a SCT would be administered clinically and may have important clinical implications.
Genotoxic damage to BM MSC following in vivo treatment appears to be a long-term effect, with significant damage persisting even 17 years after completion of therapy. Clinically, genotoxic damage to the BM micro-environment may have significant impacts on haematopoiesis, including ability to support an SCT and increasing the risk of developing second primary malignancies”