
Diagnosed with Cancer? Your two greatest challenges are understanding cancer and understanding possible side effects from chemo and radiation. Knowledge is Power!
Learn about conventional, complementary, and integrative therapies.
Dealing with treatment side effects? Learn about evidence-based therapies to alleviate your symptoms.
Click the orange button to the right to learn more.
- You are here:
- Home »
- Blog »
- side effects ID and prevention »
- Managing Oral Mucositis
Managing Oral Mucositis
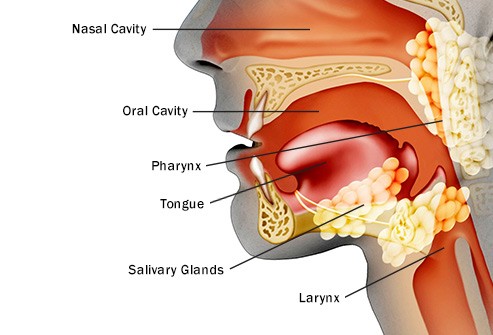
Managing oral mucositis isn’t easy. According to research, 90% of all head and neck cancer patients undergoing chemo and radiation develop this side effect.
As a cancer survivor who underwent radiation to his neck (C5), I can attest to both the benefits and risks of radiation therapy (RT).
In my opinion, the most notable aspect of the clinical trial discussed below is that conventional oncology offers little to manage oral mucositis. Yet, a non-conventional therapy such as probiotics, can provide real prevention, limit duration and/or severity of OM.
What can happen if a cancer patient develops oral mucositis?
Pain and Discomfort
- Severe Pain: Patients may experience intense pain and discomfort in the mouth, making it difficult to eat, drink, and speak.
- Ulceration: The condition can cause painful sores and ulcers in the mouth, further contributing to discomfort.
2. Nutritional Challenges
- Difficulty Eating and Drinking: Painful sores can make it challenging to consume food and liquids, leading to decreased nutritional intake.
- Weight Loss: Inadequate nutrition and hydration can result in significant weight loss and malnutrition.
- Dehydration: Reduced fluid intake due to pain can lead to dehydration.
3. Infection Risk
- Infection Susceptibility: Open sores in the mouth can serve as entry points for bacteria, increasing the risk of oral infections.
- Systemic Infections: These local infections can potentially spread, leading to systemic infections, especially in immunocompromised cancer patients.
4. Impact on Cancer Treatment
- Treatment Delays: Severe mucositis may necessitate a delay or modification in cancer treatment to allow the mouth to heal, potentially affecting the overall treatment efficacy.
- Dose Reductions: Doctors may need to reduce the dosage of chemotherapy or radiation to manage mucositis, which can impact treatment outcomes.
5. Quality of Life
- Reduced Quality of Life: The pain and difficulties associated with oral mucositis can significantly reduce a patient’s quality of life.
- Psychological Impact: Chronic pain and discomfort can lead to emotional and psychological distress, including depression and anxiety.
6. Healthcare Utilization
- Increased Healthcare Visits: Management of oral mucositis often requires additional medical visits, treatments, and possibly hospitalizations.
- Higher Medical Costs: The need for supportive care and potential complications can lead to increased healthcare costs.
Management and Prevention
Effective management and preventive strategies are critical for minimizing the impact of oral mucositis:
- Oral Hygiene: Maintaining good oral hygiene can help prevent infections and manage symptoms.
- Medications: Pain relief medications, protective coatings, and other treatments can help manage symptoms.
- Nutritional Support: Nutritional counseling and the use of supplements or alternative feeding methods can help maintain adequate nutrition.
- Preventive Measures: The use of certain medications or treatments, such as low-level laser therapy, may help prevent or reduce the severity of mucositis.
If you are a head and neck cancer patient considering radiation therapy, read more about evidence-based non-conventional therapies to manage oral mucositis.
To learn more about managing oral mucositis-
- Oral Mucositis- Prevent, Treat
- Pediatric Head & Neck Cancer- Mucositis
- Prevent Oral Mucositis in Nasopharyngeal Cancer
If you would like to discuss oral mucositis further, email me at David.PeopleBeatingCancer@gmail.com
Thank you,
David Emerson
- Cancer Survivor
- Cancer Coach
- Director PeopleBeatingCancer
Streptococcus salivarius K12 Alleviates Oral Mucositis in Patients Undergoing Radiotherapy for Malignant Head and Neck Tumors: A Randomized Controlled Trial
“Oral mucositis (OM) is a common debilitating toxicity associated with radiotherapy (RT) for malignant head and neck tumors. This prospective, randomized, double-blind, placebo-controlled trial aimed to evaluate the efficacy and safety of Streptococcus salivarius K12 (SsK12) in reducing the
- incidence,
- duration, and
- severity of severe OM (SOM)…
Patients were instructed to suck SsK12 or placebo lozenges thrice daily from the initiation to the end of RT. OM was evaluated twice a week during RT and once a week thereafter for up to 8 weeks. The primary end point was the incidence of SOM…


