Diagnosed with Cancer? Your two greatest challenges are understanding cancer and understanding possible side effects from chemo and radiation. Knowledge is Power!
Learn about conventional, complementary, and integrative therapies.
Dealing with treatment side effects? Learn about evidence-based therapies to alleviate your symptoms.
Click the orange button to the right to learn more.
- You are here:
- Home »
- Blog »
- Multiple Myeloma »
- MRD, Multiple Myeloma and Medicare
MRD, Multiple Myeloma and Medicare
The first and only test authorized by the FDA to detect and monitor minimal residual disease (MRD) in multiple myeloma (MM)…has received coverage for Medicare patients.
I am a multiple myeloma survivor on Medicare. Because MM is an older person’s disease with an average patient age of 67, I think that the majority of MM patients are also on Medicare. According to the article linked below, Medicare now covers (pays for) Minimal Residual Disease (MRD) testing for Medicare patients.
I never used to think too much about MM diagnostic testing. Frankly, I considered testing to be a commodity. For example, blood and urine testing can be performed by almost any hosptital (I think?).
Yes, there are differences between different types of imaging studies, for example what MRIs show compared to a PET scan but these tests have been around so long and oncology has no problem prescribing them and getting them covered aka paid for.
Minimal Residual Disease testing is a bit different. MRD is new it seems as if MRD status may directly impact a MM patient’s therapy plan. There is reason to believe that if a newly diagnosed MM patient achieved MRD negative status after undergoing his/her induction therapy, that he/she may not benefit from also undergoing an autologous stem cell transplant (ASCT).
If the patient will enjoy, on average, a longer progression-free survival or a longer overall survival, then there is no need for, no benefit to undergoing an expensive procedure that is sure to bring short, long-term and late stage side effects- an ASCT. At least the patient must ask him or herself the question.
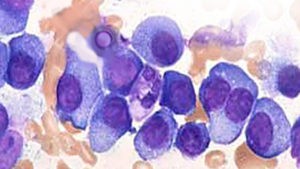
The most important issue to a long-term MM survivor like me is if multiple myeloma can be managed once it reaches MRD negative status. Meaning, once a patient’s MM has been beaten down completely enough to reach MRD negative status- one MM cell per 1 million bone marrow cells, can the patient live a normal life and die of old age some time in the distant future?
Once the patient’s MM is only one cancer cell per 1 million bone marrow cells can his/her MM be kept in complete remission with evidence-based, non-conventional, non-toxic therapies?
Have you been diagnosed with multiple myeloma? What therapies are you considering? Scroll down the page, post a question or a comment and I will reply to you ASAP.
Thank you,
David Emerson
- MM Survivor
- MM Cancer Coach
- Director PeopleBeatingCancer
Recommended Reading:
- Costs, Health Ins, E.O.B.s and More- Multiple Myeloma-
- Survey Cites Need for Multiple Myeloma Cancer Coaching
- MRD Negative Plus MDR Means No ASCT in Myeloma?
Diagnostic Test Assessing MRD in Patients With MM and ALL Receives Medicare Coverage
“The first and only test authorized by the FDA to detect and monitor minimal residual disease (MRD) in multiple myeloma (MM) and B-cell acute lymphoblastic leukemia (ALL) has received coverage for Medicare patients. ClonoSEQ, from Adaptive Biotechnologies, received Medicare coverage aligned with the assay’s FDA label and includes assessing MRD at multiple time points throughout therapy.
So far coverage was announced with Palmetto GBA, a Medicare Administrative Contractor that has jurisdiction in Alabama, Georgia, North Carolina, South Carolina, Tennessee, Virginia, and West Virginia.
MRD refers to the number of cancer cells present and can be used to monitor treatment response and help predict patient outcomes. MRD testing can assess disease burden and monitor for remission and detect relapse…
MRD assessment is becoming standard practice for patient management in blood cancers…”
Minimal residual disease predicts superior survival in patients with multiple myeloma: a meta-analysis
“MRD is a better predictor of PFS and OS than conventional complete response
To evaluate the impact of MRD status on PFS in patients who had achieved conventional CR, data were pooled from five studies involving 574 patients (396 MRD-negative, 178 MRD-positive.8,25,26,28,31 For OS, data were pooled from six studies involving 616 patients (430 MRD-negative, 186 MRD-positive).8,19,25,26,28,31 In patients achieving CR, the presence of MRD predicted shorter PFS (HR 0.44; 95% CI 0.34–0.56; P < 0.00001) (Figure 3A) and OS (HR 0.47; 95% CI 0.33–0.67; P = 0.00006) (Figure 3B). Median PFS was 56 months for MRD-negative patients and 34 months for MRD-positive patients (Figure 3C) and median OS was 112 and 82 months, respectively (Figure 3D); PFS rates were 70% and 46% at 3 years, 48% and 27% at 5 years, and 37% and 14% at 7 years, respectively. Similarly, the OS rate was higher for MRD-negative patients compared with MRD-positive patients at 3 years (94% vs 80%), 5 years (80% vs 61%), and 7 years (67% vs 47%). Tests of heterogeneity found no significant differences among the studies for PFS (χ2 = 2.68, 4 df; P = .61) and OS (χ2=4.22, 5 df; P = .62).
Among the published analyses that were not restricted to CR patients, the impact of MRD on outcomes was less clear.12–14,16–18,29,30 One study found no significant difference in outcomes between patients with or without detectable MRD.14 Others noted that MRD status did not correlate with standard response criteria.17,18 In the study conducted by Rawstron et al.,6 it was noted that 34 of 246 (26%) MRD-negative patients did not achieve conventional CR, including 29 (12%) who had less than very good partial response (VGPR). Patients who were MRD-negative but failed to achieve CR had similar PFS and OS as those who were MRD-positive. Further analyses by this group suggested that log reduction in MRD (assessed as a continuous variable, rather than using a threshold for MRD positivity vs negativity), negated the significance of response in multivariate analyses for both PFS and OS.32
None of the trials directly compared the ability of two different treatment approaches to induce MRD-negative status. However, five studies evaluated MRD status before and after ASCT.6,12,17,18,20 All five indicated that ASCT increased the proportion of patients with MRD-negative status.
The prognostic value of MRD status in relation to other prognostic factors, e.g., high-risk cytogenetics
Eleven articles reported results from univariate and/or multivariate analyses regarding the ability of MRD status to predict outcomes.13,16,18,21–26,28,30 In all 11 trials, MRD was shown to be a significant predictor of outcomes. Notably, only six articles mentioned cytogenetics: high-risk cytogenetics, defined as any t(4;14), t(14;16), or del(17p),33 was a negative predictor of PFS (or time to progression [TTP] or event free survival [EFS]) in 3 reports,18,24,26 and OS in 2 reports.18,26 In the study by Paiva et al.,26 the combination of MRD status and cytogenetics was highly predictive of TTP, and the combination of MRD status, cytogenetics, and age was predictive of OS. Only one study reported that MRD status predicted PFS and OS in patients with unfavorable cytogenetics (defined as gain[1q], del[1p32], t[4;14], t[14;20], t[14;16], and del[17p]).6 Our meta-analysis of these latter studies6,26 indicated that the best OS is seen in patients with favorable cytogenetics who achieve MRD negativity compared with patients who are either high-risk or MRD-positive; worst results are seen in patients with high-risk cytogenetics who remain MRD-positive (P < .001) (Supplementary Figure). In a more recent analysis, cytogenetics (favorable vs unfavorable vs unknown/not evaluable) and log reduction in MRD were the only significant predictors of both PFS and OS in multivariate analysis.32
The impact of maintenance therapy on MRD
Ten studies mentioned maintenance therapy,6,8,12,15,17,18,25–27,29 but only two specifically evaluated MRD status after maintenance therapy. In one article, lenalidomide maintenance therapy was reported to increase response status in 4 patients and MRD status in 5 patients12 In the MM-IX study, more MRD-positive patients became MRD-negative during thalidomide maintenance compared with patients on no maintenance (8/29 [28%] vs 1/29 [3%]).6 Furthermore, more MRD-negative patients remained MRD-negative with thalidomide maintenance than with no maintenance (24/25 [96%] vs 11/16 [69%]; P = .026)…”