Recently Diagnosed or Relapsed? Stop Looking For a Miracle Cure, and Use Evidence-Based Therapies To Enhance Your Treatment and Prolong Your Remission
Multiple Myeloma an incurable disease, but I have spent the last 25 years in remission using a blend of conventional oncology and evidence-based nutrition, supplementation, and lifestyle therapies from peer-reviewed studies that your oncologist probably hasn't told you about.
Click the orange button to the right to learn more about what you can start doing today.
- You are here:
- Home »
- Blog »
- Multiple Myeloma »
- Multiple Myeloma CAR-T
Multiple Myeloma CAR-T
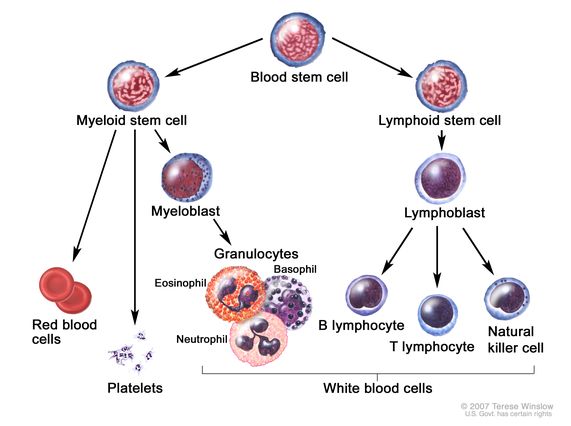
“Personalized immunotherapy using a chimeric antigen receptor (CAR) involves genetically modifying a patient’s own T cells so that they can identify and kill malignant plasma cells.10 The first B-cell maturation antigen (BCMA)–directed CAR-T cell immunotherapy, idecabtagene vicleucel (ide-cel), was approved in the United States for patients with RRMM after exposure to ≥ 4 prior LOT11“
CAR-T therapy, that is to say, genetically modifying a myeloma patient’s own T cells so that they can identify and kill multiple myeloma, has a great deal of potential. Like all new myeloma therapies however, oncology has a long way to go before this therapy is ready for primetime, as they say.
The point of this post is to provide an update of CAR-T therapy for multiple myeloma. From the perspective of a myeloma survivor.
Side Effects-
Every MM study claims the therapy to be studied, is safe and effective. The issue is to dig deeper into what safe and effective really means for the RR/MM patients. According to the studies linked below, CAR-T therapy:
- Cytokine release syndrome (CRS) was only seen in 17% of patients,
- with only one case of grade 3 toxicity and
- one case of possible neurotoxicity.
These side effects mean that CAR-T cell therapy has come a long way. By this I mean that CAR-T therapy was associated with a host of side effects in previous trials. Coupled with an ORR of 100%, I have to say that CAR-T therapy is looking better and better.
Efficacy-
According to the studies below, the overall response rate (ORR) was 100% amongst myeloma patients who had relapsed and become refractory to chemo regimens at least three times. That means that these patients were refractory to most if not all other myeloma therapies.
How long does CAR-T therapy last?
“Median duration of response was not estimable. Median progression-free survival (PFS) and overall survival (OS) were not reached; 27-month PFS and OS rates were 54.9%, respectively. Overall response rates were high across all subgroups (95.1%-100%).
Duration of response, PFS, and/or OS were shorter in patients with high-risk cytogenetics, International Staging System stage III, high tumor burden, or plasmacytomas.”
Cost-
The cost of CAR-T therapy is currently this therapy’s biggest weak spot. Information around the Internet is saying that CAR-T therapy ranges from $500,000 to more than $1,000,000. That’s a problem…
Though my assessments of CAR-T therapy are not automatic, I have been following this therapy with regular posts and it is interesting to read about the growth and maturation of this potentially revolutionary myeloma treatment.
- Myeloma- CAR-T Cell- Not Ready
- CAR-T Cell Multiple Myeloma Update
- Myeloma Therapies- Cautious Optimism for CAR-T Cell
- Newest Treatment for Myeloma
David Emerson
- MM Survivor
- MM Cancer Coach
- Director PeopleBeatingCancer
T cell
P-BCMA-101 CAR T is Effective and Safe for Refractory Myeloma, Even at Lower Doses
“Results from the PRIME study, presented at the ASH Annual Meeting & Exposition, found that P-BCMA-101, an autologous chimeric antigen receptor-T cell (CAR T) therapy, was effective and safe for patients with relapsed/refractory multiple myeloma (RRMM), even in low-dose and outpatient regimens.
P-BCMA-101 is a novel CAR T therapeutic option targeting B-cell maturation antigen (BCMA). PRIME is a phase I/II clinical trial designed to assess safety and efficacy of this treatment in patients with RRMM who have received least three previous lines of therapy…
The treatment achieved a strong safety profile for a CAR T product.
- Cytokine release syndrome (CRS) was only seen in 17% of patients,
- with only one case of grade 3 toxicity and
- one case of possible neurotoxicity.
No patients required ICU admission or other aggressive measures. Based on the safety results, the protocol was amended to allow for fully outpatient treatment administration.
Following indications of better responses at lower doses, additional cohorts were added at the lower end of the dose range. Four patients were subsequently treated with biweekly infusion cycles,
- combination therapy with rituximab or lenalidomide pre- and post-lymphodepletion, or
- single administration at the lowest dose.
- There was a 100% ORR across these cohorts at two-month follow up.
Responses are ongoing, and the safety profile in these patients was similar to the overall population.
“Current clinical data are consistent with preclinical findings that the novel design of P-BCMA-101 can produce significant efficacy, with remarkably low toxicity allowing for outpatient administration. Low doses appear highly efficacious and the modifications to manufacturing appear to have notably improved efficacy,” the researchers concluded.”
Ciltacabtagene Autoleucel, an Anti–B-cell Maturation Antigen Chimeric Antigen Receptor T-Cell Therapy, for Relapsed/Refractory Multiple Myeloma: CARTITUDE-1 2-Year Follow-Up
“At a MFU of 27.7 months (N = 97), the overall response rate was 97.9% (95% CI, 92.7 to 99.7); 82.5% (95% CI, 73.4 to 89.4) of patients achieved a stringent complete response. Median duration of response was not estimable. Median progression-free survival (PFS) and overall survival (OS) were not reached; 27-month PFS and OS rates were 54.9% (95% CI, 44.0 to 64.6) and 70.4% (95% CI, 60.1 to 78.6), respectively. Overall response rates were high across all subgroups (95.1%-100%). Duration of response, PFS, and/or OS were shorter in patients with high-risk cytogenetics, International Staging System stage III, high tumor burden, or plasmacytomas…
- Grade 3/4 thrombocytopenia occurred in 60 patients; 20 (33.3%) had recovered to grade ≤ 2 by day 30, and 35 (58.3%) recovered by day 60.
- Grade 3/4 neutropenia was reported in 95 patients; 66 (69.5%) had recovered to grade ≤ 2 by day 30 and 85 (89.5%) by day 60.
- Grade 3/4 lymphopenia occurred in 96 patients; 84 (87.5%) had recovered to grade ≤ 2 by day 30 and 88 (91.7%) by day 60…
- pneumonia (10.3%),
- hypophosphatemia (7.2%),
- increased gamma-glutamyl transferase (6.2%),
- hypertension (6.2%),
- fatigue (5.2%), and
- increased AST (5.2%)
Secondary primary malignancies-
In total, 20 secondary primary malignancies (SPMs) were reported in 16 patients; all were unrelated to cilta-cel. Nine patients had hematologic SPM, including one case of low-grade B-cell lymphoma, six cases of myelodysplastic syndrome, and three cases of fatal acute myeloid leukemia (AML; one patient had both myelodysplastic syndrome and fatal AML). Four patients had squamous cell carcinoma; one of these also had basal cell carcinoma. One patient had basal cell carcinoma that was present before cilta-cel infusion. One patient each had malignant melanoma, adenocarcinoma, or myxofibrosarcoma, and one patient had prostate cancer in addition to his squamous cell carcinoma and AML reported above…
Deaths- A total of 30 deaths occurred during the study after cilta-cel infusion (CAR-T) (Fig 1 and Appendix Table A3, online only). No deaths occurred within the first 30 days, two occurred within 100 days, and 28 occurred > 100 days post infusion…