Recently Diagnosed or Relapsed? Stop Looking For a Miracle Cure, and Use Evidence-Based Therapies To Enhance Your Treatment and Prolong Your Remission
Multiple Myeloma an incurable disease, but I have spent the last 25 years in remission using a blend of conventional oncology and evidence-based nutrition, supplementation, and lifestyle therapies from peer-reviewed studies that your oncologist probably hasn't told you about.
Click the orange button to the right to learn more about what you can start doing today.
- You are here:
- Home »
- Blog »
- Multiple Myeloma »
- Multiple Myeloma Diagnosis- Insurance, Income, Hospital Influence Outcome
Multiple Myeloma Diagnosis- Insurance, Income, Hospital Influence Outcome

“Having private insurance, living in a higher-income region and receiving treatment at an academic institution all appeared associated with significantly longer OS for patients with multiple myeloma…”
Income, Medicare, Medicaid, and where you are treated for multiple myeloma (MM) all can have dramatic results on your overall survival. The question is, can you be receive a multiple myeloma diagnosis, live in small town USA, be lower or middle class and still live a long life as a MM survivor?
I say yes. You will have to work at it but here is my thinking…
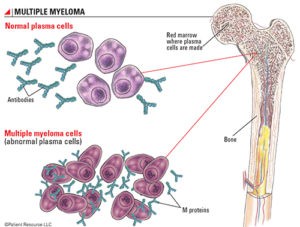
Understand that a multiple myeloma diagnosis is rare at less than 2% of all cancer diagnoses in the U.S. annually. A rare cancer means less research, few cases for oncologists to treat.
All that means that your MM diagnosis puts more pressure on you to do your homework, take responsibility for your health in the coming days, weeks, months and years.
Consulting with a MM specialist about your multiple myeloma diagnosis doesn’t mean that you have to actually sit in the specialists office. Any board certified M.D. can work with a MM specialist.
Secondly, prehabilitate. In other words, get in shape before undergoing your induction therapy and/or your autologous stem cell transplant. Studies show that you will respond better and experience fewer side effects. You can prehabilitate aka get in shape to treat your multiple myeloma diagnosis from anywhere, anytime.
Thirdly, learn about and pursue evidence-based, non-conventional therapies such as
- anti-MM nutrition,
- supplementation, and
- lifestyle therapies.
For example, integrative therapies such as curcumin can enhance the efficacy of your induction therapy. Again, this is not a fancy therapy.
And most importantly, communicate with your fellow multiple myeloma patients, survivors and caregivers. There are a number of online groups for MMers to ask, share, etc. Get the experience of people acutally living with MM not oncologists treating MM.
Be aware that the internet is more about individual experiences and less about large groups but it can help to communicate directly with MMers.
Have you received a mulitple myeloma diagnosis? What stage? What symptoms? Bone pain? Fatigue? Kidney damage? Scroll down the page, post a question or comment and I will reply to you ASAP.
Hang in there,
David Emerson
- MM Survivor
- MM Cancer Coach
- Director PeopleBeatingCancer
Recommended Reading:
- Multiple Myeloma- If I Knew Then What I Know Now
- Cancer Prehabilitation-
- Effective anti-Multiple Myeloma therapy- exercise
- Financial Assistance for Myeloma Patients- The Sooner The Better-
Socioeconomic factors linked to multiple myeloma survival
“Having private insurance, living in a higher-income region and receiving treatment at an academic institution all appeared associated with significantly longer OS for patients with multiple myeloma, according to study results presented at ASCO Annual Meeting.
The affordability of oral antineoplastics (OAM), a notoriously expensive class of drugs often used to treat multiple myeloma, may be linked to the disparity in outcomes, researchers noted. OAM prices have risen rapidly in the past several years.
“The outcome for patients with multiple myeloma has dramatically improved over the last 30 years [due to] the increased use of novel agents and autologous stem cell transplants,” Kamal Chamoun, MD, fellow in stem cell transplant and cellular therapy at University Hospitals of Case Western Reserve University in Cleveland, said during the presentation. “However, this has come with financial toxicities for patients. Multiple myeloma is now the No. 1 cancer treated with oral anticancer medications and these are often very expensive. Studies have shown that the treatment costs have nearly tripled between 2000 and 2014.”
Chamoun and colleagues analyzed data from the National Cancer Database on 117,926 patients (median age at diagnosis, 67 years; range, 19-90; 55% men; 76% white) diagnosed with multiple myeloma between 2005 and 2014 to test their hypothesis that insurance status influenced multiple myeloma survival.
A majority of the patients (57%) lived in areas with median incomes of less than $46,000 per year.
Primary insurance included:
- Medicare (54%; median age, 74 years),
- private insurance (36%; median age, 57 years) and
- Medicaid (6%; median age, 58 years).
- Three percent of patients (median age, 57 years) had no insurance.
Less than half (40%) of all patients were treated at an academic institution.
OS served as the study’s primary endpoint.
After a median follow-up of 30 months (range, 0-145), results of a multivariate analysis showed that OS was significantly worse among patients treated at other hospital types vs. at academic institutions (HR = 1.49; 95% CI, 1.39-1.59) and those with a lower vs. higher median regional income (< 46k vs. 46k; HR = 1.16; 95% CI, 1.08-1.25).
Compared with patients with private insurance, researchers observed poorer outcomes among those with
- Medicare,
- Medicaid or
- no insurance.
When the analysis was limited to patients aged 65 years or older, patients with private insurance appeared to live significantly longer than those with Medicare (median, 41.9 months; 95% CI, 40.1-43.6vs. 30.8 months; 95% CI, 30.3-31.3; P < .0001).”