
Recently Diagnosed or Relapsed? Stop Looking For a Miracle Cure, and Use Evidence-Based Therapies To Enhance Your Treatment and Prolong Your Remission
Multiple Myeloma an incurable disease, but I have spent the last 25 years in remission using a blend of conventional oncology and evidence-based nutrition, supplementation, and lifestyle therapies from peer-reviewed studies that your oncologist probably hasn't told you about.
Click the orange button to the right to learn more about what you can start doing today.
- You are here:
- Home »
- Blog »
- Multiple Myeloma »
- Multiple Myeloma and Repurposed Drugs?
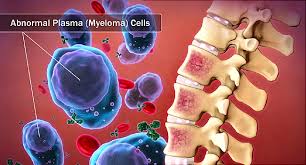
Multiple Myeloma and Repurposed Drugs?
“With well-established pharmacokinetics and an excellent toxicity profile, this low-cost agent is a strong candidate for drug repurposing as an oncological treatment…”
David Emerson
- MM Survivor
- MM Cancer Coach
- Director PeopleBeatingCancer
Recommended Reading:
Repurposing Drugs in Oncology (ReDO)—mebendazole as an anti-cancer agent
“Mebendazole, a well-known anti-helminthic drug in wide clinical use, has anti-cancer properties that have been elucidated in a broad range of pre-clinical studies across a number of different cancer types. Significantly, there are also two case reports of anti-cancer activity in humans. The data are summarised and discussed in relation to suggested mechanisms of action.
Based on the evidence presented, it is proposed that mebendazole would synergise with a range of other drugs, including existing chemotherapeutics, and that further exploration of the potential of mebendazole as an anti-cancer therapeutic is warranted. A number of possible combinations with other drugs are discussed in the Appendix…
Conclusion- The evidence for an anti-cancer effect of mebendazole treatment comes from in vitro, in vivo, in silico, and human data. Mechanistically, the microtubule action is well characterised in the laboratory and provides a similar rationale to some of the major classical chemotherapeutic drug classes, such as the taxanes and vinca alkaloids.
With well-established pharmacokinetics and an excellent toxicity profile, this low-cost agent is a strong candidate for drug repurposing as an oncological treatment, both in combination with the existing standard treatments and alongside other candidate repurposing agents in a number of specific cancer types.
We have outlined a number of these multi-drug combinations in the hope that clinicians can act upon this information to initiate clinical trials as a matter of some urgency.”
The mechanism of treatment of multiple myeloma with metformin by way of metabolism
“Introduction: Multiple myeloma (MM) is a malignant hematologic tumor. Although many new drugs are currently found to significantly improve the median survival, MM is still not curable due partly to drug resistance recurrence. Epidemiological studies have shown that patients with type 2 diabetes have a high risk of malignancy, and patients’ treatment with metformin could reduce the risk of cancer as well as associated mortality.
Material and methods: We used chemotherapeutics – melphalan combined with metformin or the single drug – to treat RPMI8226 cells and used a series of tests to detect the drug sensitivity, apoptotic rate, DNA damage and the concentration of ATP. SPSS 17.0 was used to analyze the data.
Results: The inhibitory effect of melphalan on RPMI8226 cells was significantly increased after metformin was added (p < 0.05), and the inhibitory effect was enhanced with the increasing concentration of melphalan. The comet assay showed that metformin increased melphalan-induced DNA damage and increased the apoptotic rate from 12.7 ±2.8% to 18.8 ±1.5% (p < 0.05). In the ATP concentration test, the concentration of ATP in the tumor cells was significantly decreased from 0.42 ±0.01 µmol/l to 0.08 ±0.02 µmol/l (p < 0.05).
Conclusions: Metformin can promote DNA damage induced by melphalan and decrease the concentration of ATP in the process of repairing DNA damage to hinder the anti-apoptotic process of tumor cells, which showed the pesticide effect of the enhanced sensitivity of multiple myeloma cells to melphalan…”
How I manage the toxicities of myeloma drugs
“The treatment of multiple myeloma is considered a continuously evolving paradigm as a result of the growing availability of new and highly effective drugs, including:
- first- and second-generation proteasome inhibitors,
- immunomodulatory agents,
- and monoclonal antibodies.
Clinical trials advocate long-term rather than short-term treatment schedules with combinations of these new anti–myeloma drug classes.
Although the overall toxicity profile of the recommended regimens can be considered favorable, their increasing complexity and prolonged use warrant a heightened vigilance for early and late side effects, a priori because real-life patients can be more frail or present with 1 or more comorbidities.
The treatment decision process, at diagnosis and at relapse, therefore requires myeloma physicians to carefully balance efficacy and toxicity profiles for each individual patient. Early and/or unnecessary tapering or treatment discontinuation for drug-related adverse events may not only reduce patients’ quality of life, but also negatively impact their outcome. Accurate knowledge in recognizing and managing the potential side effects of present-day treatment regimens is therefore a cornerstone in myeloma care.
Using 5 case vignettes, we discuss how to prevent and manage the most common nonhematological adverse events of anti–myeloma treatment regimens containing proteasome inhibitors, immunomodulatory drugs, and monoclonal antibodies…”


