
Diagnosed with Cancer? Your two greatest challenges are understanding cancer and understanding possible side effects from chemo and radiation. Knowledge is Power!
Learn about conventional, complementary, and integrative therapies.
Dealing with treatment side effects? Learn about evidence-based therapies to alleviate your symptoms.
Click the orange button to the right to learn more.
Reversing Osteoporosis
Yes, reversing osteoporosis is possible. I say this as a long-term survivor of a blood cancer that can cause osteoporosis or osteopenia. Virtually all survivors of my cancer, multiple myeloma, risk bone damage. Managing bone mineral density is a lifetime endeavor.
Further, according to research, 10 million Americans have been diagnosed with osteoporosis and another 44 million have low bone density and are at risk of breaking a bone.
The problem of osteoporosis is real. And reversing osteoporosis is possible. But it will take some education followed by effort.
What nutritional supplements have been shown to enhance bone health?
- Calcium: Essential for bone health, calcium is a key component of bone tissue. Adequate calcium intake is crucial, especially during periods of rapid bone growth, such as childhood, adolescence, and older adulthood.
- Vitamin D: Works synergistically with calcium to promote bone health by aiding in the absorption of calcium from the intestine. Vitamin D also helps regulate calcium and phosphorus levels in the blood, which are important for bone mineralization.
- Vitamin K: Plays a role in bone metabolism and helps activate proteins involved in bone mineralization. It’s particularly important for synthesizing osteocalcin, a protein that binds calcium to the bone matrix.
- Magnesium: Contributes to bone structure and strength by aiding in the absorption of calcium into bone tissue. It also plays a role in converting vitamin D into its active form, which is necessary for calcium absorption.
- Phosphorus: Works alongside calcium to form hydroxyapatite crystals, the primary mineral component of bone. Adequate phosphorus intake is necessary for bone mineralization and strength.
- Vitamin C: Necessary for collagen synthesis, which is an essential component of bone matrix. Collagen provides the framework for bone mineralization.
- Zinc: Supports bone formation and mineralization by activating enzymes involved in bone metabolism. Zinc deficiency can impair bone growth and healing.
- Omega-3 fatty acids: Found in fish oil and certain plant sources, omega-3 fatty acids may help reduce bone loss by decreasing inflammation and promoting bone formation.
- Boron: Some research suggests that boron may play a role in bone health by influencing calcium and magnesium metabolism and stimulating the production of hormones that promote bone growth.
The key issue that I would like to highlight is that conventional bone health medications such as
- bisphophonates and
- denosumab
are useful therapies for the short-term management of bone health. However, taking either of these therapies long-term can saddle you with a growing risk of side effects- particularly osteonecrosis of the jaw (ONJ).
So evidence-based non-conventional therapies such as:
- exercise,
- diet,
- nutritional supplementation
- whole body vibration, etc.
are the solution to long-term bone health and reversing osteoporosis.
Have you been diagnosed with osteoporosis? Or one of the diseases listed below that can lead to weak bones? Please believe me when I say that enhancing bone mineral density in hopes of reversing ostoporosis is the key to your quality of life as you age.
If you have any questions about either conventional of non-conventional bone heal therapies feel free to email me at David.PeopleBeatingCancer@gmail.com
Good luck,
David Emerson
- Cancer Survivor
- Cancer Coach
- Director PeopleBeatingCancer
Is It Possible to Reverse Osteoporosis?
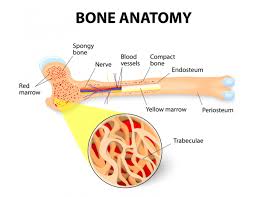
“Fractures, particularly hip and spine fractures, are a major cause of mortality and morbidity among older individuals. The term “osteoporosis” indicates increased porosity of bones resulting in low bone density; increased bone fragility; and an increased risk for fracture, often with minimal trauma…
Modifiable factors include mechanical loading of bones through exercise activity, maintaining a normal body weight, and ensuring adequate intake of micronutrients (including calcium and vitamin D) and macronutrients.
Medications such as glucocorticoids that have deleterious effects on bones should be limited as far as possible.
Endocrine, gastrointestinal, renal, and rheumatologic conditions and others, such as cancer, which are known to be associated with reduced bone density and increased fracture risk, should be managed appropriately…
A deficiency of the gonadal hormones (estrogen and testosterone) and high blood concentrations of cortisol are particularly deleterious to bone. Hormone replacement therapy in those with gonadal hormone deficiency and strategies to reduce cortisol levels in those with hypercortisolemia are essential to prevent osteoporosis and also improve bone density over time.
The same applies to management of conditions such as anorexia nervosa, relative energy deficiency in sports,
- inflammatory bowel disease,
- celiac disease,
- cystic fibrosis,
- chronic kidney disease, and
- chronic arthritis.
Once osteoporosis has developed, depending on the cause, these strategies may not be sufficient to completely reverse the condition, and pharmacologic therapy may be necessary to improve bone density and reduce fracture risk.
This is particularly an issue with postmenopausal women and older men. In these individuals, medications that increase bone formation or reduce bone loss may be necessary…
Medications that reduce bone loss (reversing osteoporosis) include bisphosphonates and denosumab; these are also called “antiresorptive medications” because they reduce bone resorption by cells called osteoclasts.
Bisphosphonates include:
and these medications have direct effects on osteoclasts, reducing their activity…
In 2019, the Endocrine Society published guidelines for managing postmenopausal osteoporosis. The guidelines recommend lifestyle modifications, including
- attention to diet,
- calcium and
- vitamin D supplements,
- and weight-bearing exercise
for all postmenopausal women. They also recommend assessing fracture risk using country-specific existing models…
It’s important to recognize that all pharmacologic therapy carries the risk for adverse events, and it’s essential to take the necessary steps to prevent, monitor for, and manage any adverse effects that may develop...
Furthermore, the occurrence of vertebral compression fractures often requires bisphosphonate treatment regardless of bone density, particularly in patients on chronic glucocorticoid therapy…


