Diagnosed with Cancer? Your two greatest challenges are understanding cancer and understanding possible side effects from chemo and radiation. Knowledge is Power!
Learn about conventional, complementary, and integrative therapies.
Dealing with treatment side effects? Learn about evidence-based therapies to alleviate your symptoms.
Click the orange button to the right to learn more.
Skin Cancer Over-diagnosis
Skin cancer over-diagnosis is a significant and growing problem in the United States. The challenge is that term “skin cancer” is a catch-all term that, in many people’s minds and can be melanoma, non-melanoma skin cancer, melanoma in-situ, and finally actinic keratosis.
Each of these is a separate diagnosis with a specific definition and level of risk.
I am not a skin cancer survivor. I was diagnosed with a rare blood cancer called multiple myeloma in early 1994. I write about skin cancer as often as possible because:
- My autologous stem cell transplant in ’95 increased my risk of skin cancer-
- I sat in the sun frequently ask a kid and burned my skin increasing my risk of skin cancer-
- Two close friends from college died from skin cancer-
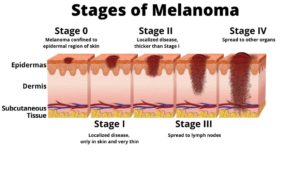
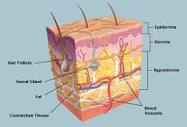
Melanoma– Melanoma is a cancer that develops from melanocytes, the skin cells that produce melanin pigment, which gives skin its color.
Non-melanoma Skin Cancer (basel, squamous cell) More than 5.4 million cases of nonmelanoma skin cancer were treated in over 3.3 million people in the U.S. in 2012, the most recent year new statistics were available.
Melanoma In-Situ– Melanoma in-situ is also called stage 0 melanoma. It means there are cancer cells in the top layer of skin (the epidermis). The melanoma cells are all contained in the area in which they started to develop and have not grown into deeper layers of the skin. Some doctors call in situ cancers pre cancer.
Actinic Keratosis– If you have an actinic keratosis (AK) on your skin, you have one of the most common skin conditions that dermatologists treat.1 It is estimated that more than 40 million Americans develop actinic keratoses (AKs) each year.2
A diagnosis of actinic keratosis increases your risk of non-melanoma skin cancer and a diagnosis of non-melanoma skin cancer increases your risk of a diagnosis of melanoma.
Melanoma at a glance-
- Risks– UV Exposure, HPV, Genetics, Skin Pigment, Moles, Immunosuppression, Previous Skin Cancer Diagnosis,
- Symptoms- Mole, Shape (A,B,C,D,E), Itching, Bleeding,
- Diagnosis- Visual Inspection, Skin Biopsy,
- Prognosis– Staging, In-situ, I, II, III, IV, Five year survival rates
- Therapy– Conventional, Non-Conventional, Integrative, Alternative
How to Identify Skin Cancer
It’s important to closely examine your skin for any new or changing moles or growths, and to do so on a regular basis. When checking your body for SC, doctors advise the following ABCDE rule:
1) Asymmetry – Healthy moles should be round and symmetrical.
2) Border – A clearly defined border is common in healthy skin growths and should not be blurred or faded.
3) Color – Pay attention to the color of your moles. Any that contain several shades of black, brown, or blue should be examined by a dermatologist.
4) Diameter – Any moles larger than a ¼ inch in diameter may need to be looked at by a professional.
5) Evolving – If you have a mole or skin growth that is changing in shape, size, or color, make an appointment with a trained dermatologist immediately for further examination.
As you can see, a diagnosis of “skin cancer” can be various degrees of seriousness. When the research linked and excepted below talks about skin cancer over-diagnosis, I think it is probable that a person receives a diagnosis of melanoma when the skin sample is actually non-melanoma skin cancer or melanoma in-situ.
In other words, reading these many similar yet different terms for skin discoloration, it is easier to understand how and why there are so many skin cancer mis-diagnoses in the United States each year.
The reality is that you will probably be diagnosed with some type of skin cancer in your life. And there is a good chance that this diagnosis is incorrect. Or I should say that it is in your best interest to have a second opinion to confirm your diagnosis- whatever it is.
Have you been diagnosed with actinic keratosis, non-melanoma skin cancer or melanoma in-situ? If you’d like to learn more about evidence-based nutrition, supplementation and lifestyle therapies to reduce your risk of a full melanoma diagnosis send me an email at David.PeopleBeatingCancer@gmail.com
Hang in there,
David Emerson
- Cancer Survivor
- Cancer Coach
- Director PeopleBeatingCancer
Ecological study estimating melanoma overdiagnosis in the USA using the lifetime risk method
“Objectives To quantify the proportion of melanoma diagnoses (invasive and in situ) in the USA that might be overdiagnosed…
Results Between 1975 and 2018 the adjusted lifetime risk of being diagnosed with melanoma (invasive and in situ) increased from 3.2% (1 in 31) to 6.4% (1 in 16) among white men, and from 1.6% (1 in 63) to 4.5% (1 in 22) among white women.
Over the same period, the adjusted lifetime risk of being diagnosed with melanoma in situ increased from 0.17% (1 in 588) to 2.7% (1 in 37) in white men and 0.08% (1 in 1250) to 2.0% (1 in 50) in white women.
An estimated 49.7% of melanomas diagnosed in white men and 64.6% in white women were overdiagnosed in 2018. Among people diagnosed with melanomas in situ, 89.4% of white men and 85.4% of white women were likely overdiagnosed in 2018.
Conclusions Melanoma overdiagnosis among white Americans is significant and increasing over time with an estimated 44 000 overdiagnosed in men and 39 000 in women in 2018. A large proportion of overdiagnosed melanomas are in situ cancers, pointing to a potential focus for intervention.”
Study Concludes Most Melanoma Overdiagnoses Are In Situ
“TOPLINE: Melanoma in situ drives most cases of melanoma overdiagnoses, Surveillance, Epidemiology, and End Results (SEER) analysis found…
- The increase in melanoma diagnoses in the United States, while mortality has remained flat, has raised concerns about overdiagnosis of melanoma, cases that may not result in harm if left untreated. How much of the overdiagnoses can be attributed to melanoma in situ vs invasive melanoma is unknown…
TAKEAWAY:
- Researchers found that between 1975 and 2018, the adjusted lifetime risk of being diagnosed with melanoma in situ increased from 0.17% to 2.7% in White men and 0.08% to 2% in White women.
- An estimated 49.7% and 64.6% of melanomas diagnosed in White men and White women, respectively, were overdiagnosed in 2018.
- Among individuals diagnosed with melanoma in situ, 89.4% of White men and 85.4% of White women were likely overdiagnosed in 2018.
IN PRACTICE: “A large proportion of overdiagnosed melanomas (skin cancer over-diagnosis) are in situ cancers, pointing to a potential area to focus for an intervention de-escalation of the intensity of treatment and survivorship care,” the authors wrote.