
Recently Diagnosed or Relapsed? Stop Looking For a Miracle Cure, and Use Evidence-Based Therapies To Enhance Your Treatment and Prolong Your Remission
Multiple Myeloma an incurable disease, but I have spent the last 25 years in remission using a blend of conventional oncology and evidence-based nutrition, supplementation, and lifestyle therapies from peer-reviewed studies that your oncologist probably hasn't told you about.
Click the orange button to the right to learn more about what you can start doing today.
- You are here:
- Home »
- Blog »
- Multiple Myeloma »
- Transplant-INeligible Multiple Myeloma
Transplant-INeligible Multiple Myeloma
All newly diagnosed myeloma patients are prescribed the standard-of-care MM therapy plan. Therefore, there are only two kinds of newly diagnosed multiple myeloma (NDMM) patients in this world. You are either eligible for an autologous stem cell transplant or you diagnosed as transplant-INeligible multiple myeloma.
How many transplant-ineligible multiple myeloma patients are diagnosed each year? It turns out that number is difficult to determine. Let’s try anyway…
In an effort to figure out the percentage of transplant-ineligible multiple myeloma diagnoses, I will start with the basics. According to the NCI, 34,470 people were diagnosed with MM in 2022.
Further, I will add that the FDA approved standard-of-care for all newly diagnosed myeloma patients is the treatment plan is:
- Induction therapy
- Autologous stem cell transplant
- low-dose maintenance therapy
I mention this to say that all NDMM patients, regardless of age or stage, who are newly diagnosed with myeloma are told that they should undergo an ASCT. All 100% of over 34,000 NDMM patients in 2022 were told this.
According to research Only 20% to 50% of patients with multiple myeloma undergo autologous stem cell transplantation (ASCT).
But this statistic doesn’t tell us how many NDMM patients are considered to be transplant-ineligible. Some newly diagnosed myeloma patients will be Ineligible for an ASCT, some NDMM patients will not want this therapy.
Again, this statistic doesn’t give us the answer to how many transplant-ineligible NDMM patients are diagnosed each year either.
If up to half of all NDMM patients do not undergo an ASCT annually and half of all MM patients are ineligible for inclusion into clinical trails, I believe that a big chunk of NDMM patients are Ineligible for an ASCT. But how big is that chunk???
I estimate that 40-50% of NDMM patients are considered to be transplant-ineligible multiple myeloma. Because most MM research is based on patients having an ASCT, it means that NOT having an ASCT means that these patients must think outside-the-box about how to treat their MM.
What his transplant-ineligible multiple myeloma?
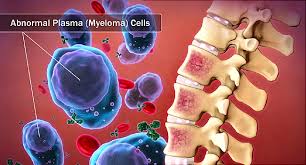
Transplant-ineligible multiple myeloma refers to a subset of patients with multiple myeloma who are not considered suitable candidates for stem cell transplantation (also known as a bone marrow transplant). Multiple myeloma is a type of cancer that affects plasma cells, a type of white blood cell found in the bone marrow.
Stem cell transplantation is a treatment option for some patients with multiple myeloma, where high-dose chemotherapy is used to eliminate cancer cells, followed by the infusion of healthy stem cells to help the bone marrow recover. However, not all patients are eligible or suitable for this procedure.
Transplant ineligibility may be due to various factors, such as
- age,
- overall health,
- existing medical conditions,
- or the presence of other complications that make the transplantation process too risky for the patient.
In such cases, alternative treatment approaches, including various chemotherapy regimens and targeted therapies, are considered to manage the disease and improve the patient’s quality of life. Treatment decisions are typically made based on individual patient characteristics and the stage of the disease.
What does the average newly diagnosed multiple myeloma patient look like?
If you are too sick, frail or have advanced MM to be deemed transplant ineligible, what does this say about your prognosis? It says that you must depend on
- novel therapies for the treatment of your MM
- evidence-based non-conventional theories for the treatment of your MM
For the record, I have an ASCT and the only thing it did for me was to saddle me with a host of short, long-term and late stage side effects. I believe that chemotherapy and radiation must be used judiciously. Conventional oncology over treats NDMM patients. An ASCT is an example of what I consider over-treatment.
Are you considered to be non-transplant eligible? If you would like to learn more about evidence-based non-conventional therapies let me know- David.PeopleBeatingCancer@gmail.com
Hang in there,
David Emerson
- MM Survivor
- MM Cancer Coach
- Director PeopleBeatingCancer
This Frontline Therapy Is Better in Transplant-Ineligible Multiple Myeloma: Study
“The study found that frontline triple therapy with daratumumab plus lenalidomideand dexamethasone led to significantly longer time to next treatment (PFS) or time to death (OS) compared with the triple combination that includes bortezomib instead of daratumumab…
Despite the lack of head-to-head randomized trials in this setting, several indirect comparisons have suggested that the daratumumab regimen carries an efficacy edge…
For instance, an indirect comparison of patients who received the daratumumab regimen in the MAIA trial with those who received the bortezomib regimen in the SWOG S0777 trial revealed a 40% lower risk for disease progression or death among patients treated with daratumumab…
After making these adjustments, the study included data on 302 patients who received frontline therapy with the daratumumab regimen and 341 who received the bortezomib regimen. Patients who underwent hematopoietic stem cell transplant before or during therapy were excluded, as were those who had prior primary solid tumors, hematologic malignancies, or amyloidosis.
During a 20.2-month median follow-up for patients on daratumumab, 98 (32%) switched to a new therapy or died. During a 21.5-month median follow-up for those on bortezomib, 175 (51%) switched treatments or died.
The median time to death was 37.8 months in the daratumumab group vs 18.7 months in the bortezomib group. Overall, patients who received the daratumumab regimen had a 42% lower risk for death or time-to-next treatment (adjusted hazard ratio…


