
Recently Diagnosed or Relapsed? Stop Looking For a Miracle Cure, and Use Evidence-Based Therapies To Enhance Your Treatment and Prolong Your Remission
Multiple Myeloma an incurable disease, but I have spent the last 25 years in remission using a blend of conventional oncology and evidence-based nutrition, supplementation, and lifestyle therapies from peer-reviewed studies that your oncologist probably hasn't told you about.
Click the orange button to the right to learn more about what you can start doing today.
- You are here:
- Home »
- Blog »
- Multiple Myeloma »
- Transplant Ineligible Myeloma- Darzalex (DRd)
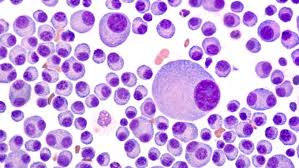
Transplant Ineligible Myeloma- Darzalex (DRd)
“daratumumab was approved for use in combination with lenalidomide and dexamethasone for patients with newly diagnosed multiple myeloma who are ineligible for autologous stem cell transplantation”
There’s good news and bad news…at least for newly diagnosed multiple myeloma (MM) patients who are INeligible for an autologous stem cell transplant (ASCT). Daratumumab, revlimid, dexamethasone (DRd) has been approved for you.
As the study below explains, this newly approved triplet was extremely effective at putting this group of MM patients into remission. The challenge is the toxicity that you will be exposed to. Toxicity can lead to adverse events aka side effects.
The reason why you are INeligible for an ASCT, standard care for MM patients, is because you are too old, frail or perhaps you have co-morbidities such as heart issues, kidney issues, etc. My point here is that chemotherapy is toxic. Even a triplet such as Daratumumab, plus lenalidomide (revlimid) and low-dose dexamethasone (DRd).
Your goal is about balancing quantity-of-life with quality-of-life. In my opinion anyway.
Please consider evidence-based but non-toxic, non-conventional MM therapies. If you are reading this post before you have begun this toxic induction triplet, consider “Pre-habilitation.” Let me know if you’d like more info about how to do that.
In short, please understand that just because a therapy is tested and approved by the FDA, it doesn’t mean that there are not serious risks for the MM patient. Especially those MM patients Ineligible for an ASCT.
Scroll down the page, post a question or comment to learn more about evidence-based non-conventional MM therapies.
Hang in there,
David Emerson
- MM Survivor
- MM Cancer Coach
- Director PeopleBeatingCancer
Recommended Reading:
- Complete Remission vs. Overall Survival in Multiple Myeloma-
- Mind-Body Therapy- Essential Reading for the Newly Diagnosed Myeloma Patient
- Frailty Index Predicts Myeloma Outcome
Daratumumab-Based Therapy for Patients With Newly Diagnosed Multiple Myeloma Who Are Ineligible for Transplantation
“On June 27, 2019, daratumumab was approved for use in combination with lenalidomide and dexamethasone for patients with newly diagnosed multiple myeloma who are ineligible for autologous stem cell transplantation.1,2
Approval was based on findings in the open-label phase III MAIA trial (ClinicalTrials.gov identifier NCT02252172).2,3 In the trial, 737 patients were randomly assigned to receive daratumumab plus lenalidomide and low-dose dexamethasone (DRd; n = 368) or lenalidomide and low-dose dexamethasone (Rd; n = 369). Patients received 28-day cycles of lenalidomide at 25 mg on days 1 through 21 and dexamethasone at 40 mg on days 1, 8, 15, and 22. Daratumumab was given at 16 mg/kg once weekly during cycles 1 and 2, every 2 weeks during cycles 3 through 6, and every 4 weeks thereafter. Treatment was continued until disease progression or unacceptable toxicity.
The median age of patients was 73 years (range = 45–90 years; 44% aged ≥ 75 years); 92% were white; 52% were male; an Eastern Cooperative Oncology Group performance status was 0 for 34%, 1 for 50%; and ≥ 2 for 17%; the International Staging System stage was I in 27%, II in 43%, and III in 29%...
Daratumumab carries warnings/precautions for infusion reactions, interference with crossmatching and red blood cell antibody screening, neutropenia, and thrombocytopenia.
Median progression-free survival based on International Myeloma Working Group criteria was not reached in the DRd group vs 31.9 months in the Rd group (hazard ratio = 0.56, P < .0001). Overall response rate was 92.9% vs 81.3% (P < .0001), and complete response or better was achieved in 47.6% vs 24.9% (P < .0001)…
Daratumumab can cause severe and serious infusion reactions, including anaphylactic reactions. Approximately half of all patients in clinical trials experienced an infusion reaction. Daratumumab should be administered by a health-care professional, with immediate access to emergency equipment and appropriate medical support to manage infusion reactions…
DARATUMUMAB IN UNTREATED MYELOMA…
Product labeling provides instructions on preinfusion and postinfusion medication. Patients should be premedicated with corticosteroids, antihistamines, and antipyretics. When dexamethasone is the background regimen–specific corticosteroid, the dexamethasone treatment dose will serve as premedication on daratumumab infusion days. Use of low-dose oral methylprednisolone (or its equivalent) should be considered on the day after daratumumab infusion; postinfusion medication may not be needed if a background regimen–specific corticosteroid is administered the day after daratumumab infusion. Use of postinfusion medications such as short- and long-acting bronchodilators and inhaled corticosteroids should be considered in patients with a history of chronic obstructive pulmonary disease Antiviral prophylaxis for herpes zoster reactivation should be given within 1 week after starting daratumumab and continued for 3 months after treatment.
Safety Profile
In clinical trial experience with daratumumab, the most common adverse events of any grade (≥ 20% of patients) have been infusion reactions, neutropenia, thrombocytopenia, fatigue, nausea, diarrhea, constipation, vomiting, muscle spasms, arthralgia, back pain, pyrexia, chills, dizziness, insomnia, cough, dyspnea, peripheral edema, peripheral sensory neuropathy, and upper respiratory tract infection.
In the MAIA trial, the most common adverse events of any grade in the daratumumab group occurring with a ≥ 5% higher frequency than in the Rd group were diarrhea (57% vs 46%), upper respiratory tract infection (52% vs 36%), infusion reactions (41% vs 0%), constipation (41% vs 36%), peripheral edema (41% vs 33%), fatigue (40% vs 28%), back pain (34% vs 26%), dyspnea (32% vs 20%), nausea (32% vs 23%), asthenia (32% vs 25%), cough (30% vs 18%), bronchitis (29% vs 21%), muscle spasms (29% vs 22%), and pneumonia (26% vs 14%). The most common grade 3 or 4 adverse events included pneumonia (15% vs 8%), fatigue (8% vs 4%), diarrhea (7% vs 4%), and hyperglycemia (7% vs 4%). The most common grade 3 or 4 laboratory abnormalities were neutropenia (56% vs 39%), lymphopenia (52% vs 42%), and leukopenia (35% vs 24%). Serious adverse reactions with a 2% greater incidence in the DRd group vs the Rd group were pneumonia (15% vs 8%), bronchitis (4% vs 2%), and dehydration (2% vs <1%).
Daratumumab carries warnings/precautions for infusion reactions, interference with cross-matching and red blood cell antibody screening, neutropenia, and thrombocytopenia. Patients should have a blood type and screen prior to starting treatment; if a patient needs a blood transfusion, the blood bank should be informed that a patient has received daratumumab.
Complete blood cell counts should be monitored periodically during treatment. Daratumumab is contraindicated in patients with a history of severe hypersensitivity to daratumumab or any of the components of the formulation. ■
REFERENCES
1. U.S. Food and Drug Administration: FDA approves daratumumab for multiple myeloma ineligible for autologous stem cell transplant. Available at www.fda.gov/drugs/resources-information-approved-drugs/fda-approves-daratumumab-multiple-myeloma-ineligible-autologous-stem-cell-transplant. Accessed July 23, 2019.
2. Darzalex (daratumumab) injection prescribing information, Janssen Biotech, June 2019. Available at www.accessdata.fda.gov/drugsatfda_docs/label/2019/761036s020lbl.pdf. Accessed July 23, 2019.
3. Facon T, Kumar S, Plesner T, et al: Daratumumab plus lenalidomide and dexamethasone for untreated myeloma. N Engl J Med 380:2104-2115, 2019.



