Recently Diagnosed or Relapsed? Stop Looking For a Miracle Cure, and Use Evidence-Based Therapies To Enhance Your Treatment and Prolong Your Remission
Multiple Myeloma an incurable disease, but I have spent the last 25 years in remission using a blend of conventional oncology and evidence-based nutrition, supplementation, and lifestyle therapies from peer-reviewed studies that your oncologist probably hasn't told you about.
Click the orange button to the right to learn more about what you can start doing today.
- You are here:
- Home »
- Blog »
- Multiple Myeloma »
- Multiple Myeloma Bone Health- Denosumab vs. Bisphophonates?
Multiple Myeloma Bone Health- Denosumab vs. Bisphophonates?
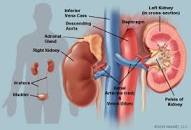
“Prescribers are advised that zoledronic acid (bisphophonates) is associated with reports of renal impairment and renal failure, especially in patients with pre-existing renal dysfunction…”
Hi David- I’m wondering your perception on the best modality to strengthen bones for a multiple myeloma bone health. I’ve heard about Denosumab, and would be interested in your thoughts on it.
Per CRAB acronym, only the Bone part has showed up in my blood work.
Thank You Abundantly! Monica
- MM patients may undergo bone therapies either for months initially, or repeatedly in their lives as MM patients.
- MM patients are often older and my present with reduced kidney function to begin with.
- Lastly, MM proteins themselves, MM as a disease, may cause kidney damage.
- creatinine,
- BUN,
- eGFR
- kidney damage and
- if your serum calcium is above the normal range indicating bone involvement, and
- if you can afford Denosumab,
- MM Survivor
- MM Cancer Coach
- Director PeopleBeatingCancer
Recommended Reading:
- Multiple Myeloma Symptoms Cloud Multiple Myeloma Side Effects-
- Multiple Myeloma- Enhance Bone Health w/ Probiotics-
- Multiple Myeloma Therapy- MRD- Bisphosphonate vs. Supplements
Renal Safety in Patients Treated With Bisphosphonates for Osteoporosis: A Review
Zoledronic acid associated with adverse effects on renal function
“Prescribers are advised that zoledronic acid is associated with reports of renal impairment and renal failure, especially in patients with pre-existing renal dysfunction…”
Denosumab vs Zoledronic Acid in Newly Diagnosed Multiple Myeloma With Bone Disease
“In a phase III trial reported in The Lancet Oncology, Raje et al found that denosumab was noninferior to zoledronic acid in preventing skeletal-related events (SREs) in newly diagnosed multiple myeloma patients with bone disease…
Adverse Events-
The most common grade ≥ 3 adverse events in the denosumab vs zoledronic acid groups were
- neutropenia (15% vs 15%),
- thrombocytopenia (14% vs 12%),
- anemia (12% vs 10%),
- febrile neutropenia (11% vs 10%), and
- pneumonia (8% vs 8%).
Renal toxicity was reported in 10% vs 17%. Any-grade hypocalcemia occurred in 17% vs 12%. Osteonecrosis of the jaw occurred in 4% vs 3% (P = .147). The most common serious adverse event in both groups was pneumonia (8% in both). One patient in the zoledronic acid group died of cardiac arrest that was considered treatment-related.