
Diagnosed with Cancer? Your two greatest challenges are understanding cancer and understanding possible side effects from chemo and radiation. Knowledge is Power!
Learn about conventional, complementary, and integrative therapies.
Dealing with treatment side effects? Learn about evidence-based therapies to alleviate your symptoms.
Click the orange button to the right to learn more.
- You are here:
- Home »
- Blog »
- Skin Cancer »
- Actinic Keratosis, Non-Melanoma, Melanoma In-Situ
Actinic Keratosis, Non-Melanoma, Melanoma In-Situ
Actinic Keratosis is a form of pre-cancer. Basel Cell and Squamous Cell Cancers are common forms of skin cancer called Non-Melanoma skin cancer and are rarely fatal. Melanoma In-situ is also skin cancer but stage 0 and is also rarely fatal
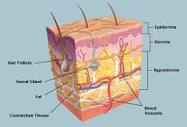
The skin is a human beings largest organ. The list of potential problems that can occur to our skin is long and complex. Like most of what’s discussed on PeopleBeatingCancer, my interest in skin cancer are those therapies that are evidenced-based, non-conventional and non-toxic and that can help the largest number of skin cancer patients.
- Actinic Keratosis (AK)- according to research more then 58 million Americans have one or more AK spots
- Non-Melanoma Skin Cancer- (NMSC) according to research 3.6 million cases of basal cell carcinoma and 1.8 million cases of squamous cell carcinoma are diagnosed in the U.S. annually-
- Melanoma Skin Cancer In-Situ- according to research 97,920 cases of melanoma in situ (noninvasive), are diagnosed annually in the United Stats.
In my experience, the primary issue for any cancer is risk and rewards. Risk/reward that the cancer damages the patient. Risk/reward that the therapy damages the patient. A cancer diagnosis, any cancer, is all about risk/reward.
PeopleBeatingCancer.org focuses on the these three forms of skin diseases and non-conventional therapies due to their specific risk/reward profile. While the diagnosis of either AK, NMSK or Melanoma In-situ brings a risk of death, this risk is low. And evidence-based, non-conventional therapies bring a low risk of side effects with a potential to reduce the patient’s risk of death.
- To Learn More About Non-Toxic Therapies for Pre-Cancer- click now
- To Learn More About Actinic Keratosis- click now
David Emerson
- Cancer Survivor
- Cancer Coach
- Director PeopleBeatingCancer
Recommended Reading-
- Non-Melanoma Skin Cancer Risk Increases From Radiation
- Preventing Non-Melanoma Skin Cancer Relapse
- How to Identify Skin Cancer in 5 Steps
- Skin Cancer, Vitamin D3 and Sunlight
Skin Cancer (Including Melanoma)
“Skin cancer is the most common type of cancer. The main types of skin cancer are
Melanoma stages I-IV is much less common than the other types but much more likely to invade nearby tissue and spread to other parts of the body. Most deaths from skin cancer are caused by melanoma. Explore the links on this page to learn more about skin cancer prevention, screening, treatment, statistics, research, clinical trials, and more…”
Actinic Keratosis
Untreated AKs follow one of three paths:
- they can either persist as AKs,
- regress,
- or progress to invasive skin cancer,
As AK lesions are considered to be on the same continuum with squamous cell carcinoma (SCC).[17] AK lesions that regress also have the potential to recur.
- Progression: The overall risk of an AK turning into invasive cancer is low. In average-risk individuals, likelihood of an AK lesion progressing to SCC is less than 1% per year.[88][89] Despite this low rate of progression, studies suggest that a full 60% of SCCs arise from pre-existing AKs, reinforcing the idea that these lesions are closely related.[88][89]
- Regression: Reported regression rates for single AK lesions have ranged between 15–63% after one year.[90]
- Recurrence: Recurrence rates after 1 year for single AK lesions that have regressed range between 15–53%.[90]
Basal-cell cancer is a very common skin cancer. It is much more common in fair-skinned individuals with a family history of basal-cell cancer and increases in incidence closer to the equator or at higher altitude. There are approximately 800,000[55] new cases yearly in the United States alone. Up to 30% of White people develop basal-cell carcinomas in their lifetime.[56] In Canada, the most common skin cancer is basal-cell carcinoma (as much as one third of all cancer diagnoses), affecting 1 in 7 individuals over a lifetime.[57]
In the United States approximately 3 out of 10 White people develop a basal-cell carcinoma during their lifetime.[56] This tumor accounts for approximately 70% of non-melanoma skin cancers. In 80 percent of all cases, basal-cell carcinoma affects the skin of head and neck.[56] Furthermore, there appears to be an increase in the incidence of basal-cell cancer of the trunk in recent years.[56]
Most sporadic BCC arises in small numbers on sun-exposed skin of people over age 50, although younger people may also be affected. The development of multiple basal-cell cancer at an early age could be indicative of nevoid basal-cell carcinoma syndrome, also known as Gorlin Syndrome.[58]
Risk of Invasive Cutaneous Squamous Cell Carcinoma After Different Treatments for Actinic Keratosis
“Question What is the risk of cutaneous squamous cell carcinoma (cSCC) in patients with multiple actinic keratoses (AKs), and which factors contribute to an increased risk?
Meaning Olsen grade III AK was identified as a marker for an increased risk of cSCC, as was the need for additional treatment.
Low plasma coenzyme Q10 levels as an independent prognostic factor for melanoma progression
“Background: Abnormally low plasma levels of coenzyme Q10 (CoQ10) have been found in patients with cancer of the breast, lung, or pancreas.
Objective: A prospective study of patients with melanoma was conducted to assess the usefulness of CoQ10 plasma levels in predicting the risk of metastasis and the duration of the metastasis-free interval…
Results: CoQ10 levels were significantly lower in patients than in control subjects (t test: P < .0001) and in patients who developed metastases than in the metastasis-free subgroup (t test: P < .0001). Logistic regression analysis indicated that plasma CoQ10 levels were a significant predictor of metastasis (P = .0013)…
Conclusions: Analysis of our findings suggests that baseline plasma CoQ10 levels are a powerful and independent prognostic factor that can be used to estimate the risk for melanoma progression.

