
Diagnosed with Cancer? Your two greatest challenges are understanding cancer and understanding possible side effects from chemo and radiation. Knowledge is Power!
Learn about conventional, complementary, and integrative therapies.
Dealing with treatment side effects? Learn about evidence-based therapies to alleviate your symptoms.
Click the orange button to the right to learn more.
- You are here:
- Home »
- Blog »
- side effects ID and prevention »
- Diagnosed with Melanoma? Get a Second Opinion!
Diagnosed with Melanoma? Get a Second Opinion!
These results show that diagnoses ranging from moderately atypical lesions to early stage invasive melanoma are neither accurate nor reproducible, say the authors.
While I am the first person to be cynical about conventional oncology I am also the first person to admit that diagnosing cancer is difficult. The article below talks about melanoma. But pathologists have similar challenges with many cancers including breast, colorectal and prostate cancer. Challenging diagnoses is one of the many reasons to get a second opinion.
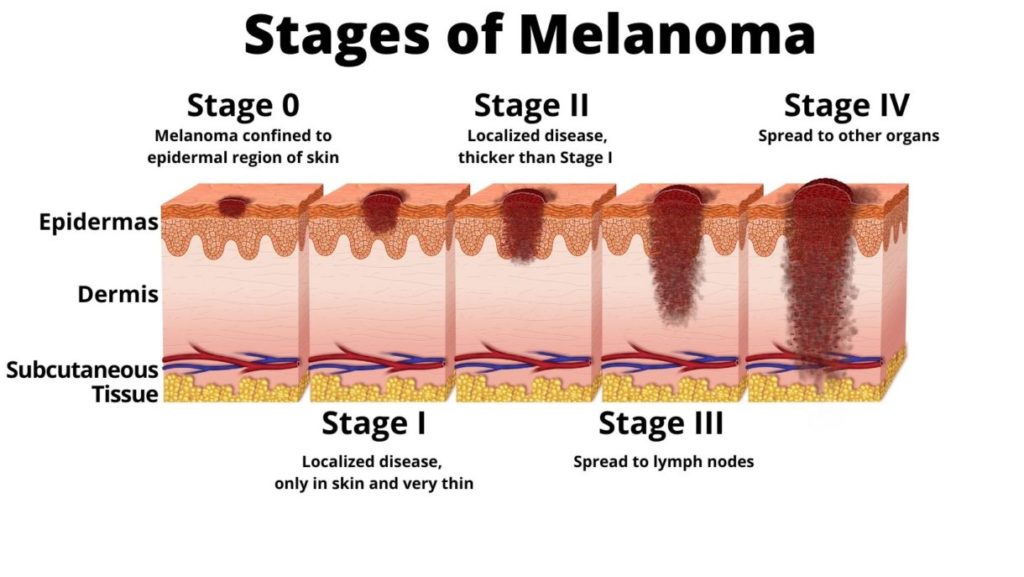
Further, a diagnosis of any cancer is not a zero/sum game. Just because your oncologist is told by the pathologist that the sample removed from your skin is in fact melanoma, it is then challenging to determine the stage and therapy plan-
To complicate this issue further conventional oncology has few if any effective therapies for melanoma yet there are several integrative therapies shown to enhance the efficacy of specific chemotherapy regimens.
- Is the cancer aggressive or slow growing?
- What is the age and health of the patient? How will the patient respond to chemotherapy and or radiation?
- Do I treat the cancer more or less aggressively ? Is it about quantity or quality of life?
I am a long-term survivor of an “incurable” cancer called multiple myeloma. I am also a cancer coach. Have you been diagnosed with melanoma? Scroll down the page, post a question or comment and I will reply to you ASAP.
To Learn More About Melanoma- click now
Thank you,
David Emerson
- Cancer Survivor
- Cancer Coach
- Director PeopleBeatingCancer
Recommended Reading:
- Non-Melanoma Skin Cancer Risk Increases From Radiation
- Preventing Non-Melanoma Skin Cancer Relapse
- How to Identify Skin Cancer in 5 Steps
- Skin Cancer, Vitamin D3 and Sunlight
Study raises concern over accuracy of melanoma diagnoses
“The results show that diagnoses can vary among pathologists, particularly for cases in the middle of the disease spectrum, suggesting the potential for both overdiagnosis and under diagnosis…
Diagnosis relies on visual assessment of skin samples (biopsies) under a microscope by a pathologist, but the reliability of the criteria used to diagnose these skin lesions have never been established with rigorous standards…
The study was inspired by Dr Elmore’s experience as a patient undergoing a skin biopsy, which resulted in three different independent interpretations, ranging from benign to invasive melanoma. Ten years later she is healthy and doing research on the topic…
The highest levels of accuracy were found for class I mild lesions (92%) and class V high stage invasive melanoma (72%) – these cases are at the polar ends of the disease spectrum…
In contrast, interpretations for cases in the middle of the spectrum had noticeably lower accuracy, as less than half of the diagnoses were in concordance with the reference diagnosis; class II moderately atypical lesions (25%); class III severely atypical lesions and melanoma in situ (40%); and class IV early stage invasive melanoma (43%)…
Many pathologists agree overdiagnosis of skin cancer happens, but don’t change diagnosis behavior
“As the most serious type of skin cancer, a melanoma diagnosis carries emotional, financial and medical consequences. That’s why recent studies finding that there is an overdiagnosis of melanoma are a significant cause for concern.
“Overdiagnosis is the diagnosis of disease that will not harm a person in their lifetime. If melanoma is being overdiagnosed, it means that too many people are getting the scary news that they have cancer, and receiving and paying for unnecessary treatment,” said Kathleen Kerr, professor of biostatistics in the UW School of Public Health.
Kerr recently published results of a study involving more than 100 dermatopathologists — pathologists who specialize in skin diseases and who diagnose melanoma — to find out if they believe that melanoma overdiagnosis is a public health issue in the U.S. and whether that belief affects their own conclusions. The pathologists were given biopsy slides to diagnose and were surveyed on their perceptions of overdiagnosis.
Kerr discussed the results of this study, published April 20 in JAMA Dermatology, in the following Q&A with UW News:
- How can you know if a disease is being overdiagnosed?
- Why does this happen when it comes to melanoma?
- What did find in your study?
- What do you think is the importance of this finding?
Leave a Comment:
4 comments
Hi. I was diagnosed with in situ melanoma 20 years ago and had it excised. A few months ago I noticed a freckle on the scar so had another biopsy. It is also in situ. Two excision later WITH NO VISIBLE CANCER they still didn’t get clear margins. The plan is to wait two months to heal then go back and take more skin. If you can’t see anything, yet biopsy shows cancer cells they can be anywhere and everywhere. Is this the best approach? Lord knows where else it might be since it’s invisible to the eye!
ReplyHi Timmie-
I am not well-versed on pre-melanoma but it sounds to me as though you and your Drs. are being cautious. This is good. Meaning, melanoma ins-site is pre-melanoma, not cancer. But there are some cancer cells there so to be safe, you are removing them. This is all you can do. If this therapy (removing cells) ever becomes painful or causes infections or anything like this, you maybe being overly cautious.
All to say, you sound like you are making an effort to not let your pre-melanoma become full melanoma.
David Emerson
ReplyI have Myeloma diagnosed in April. I have been to the mm institute in Little Rock Arkansas and to MD Anderson. I don’t have any lesions or kidney issues.
I am petrified about chemo and most days feel like I’d rather die than go through it. MD wants me to begin in one week and I’m trying to decide what to do. I am 66, weigh 97lbs. & have been very healthy up until now. I would love to hear from you.
Hi Waverly-
I am sorry for your MM diagnosis. Several things. First of all, both UAMS and MDA are top notch MM centers. They are conventional and aggressive but they are two of the best if you choose to go that route.
Secondly, it sounds like you are early MM or stage 1. You say you have no bone involvement and no kidney damage. Have you been told your monoclonal protein aka m-spike? Depending on your stage you may be better off not undergoing an autologous stem cell transplant at this point.
Thirdly, research confirms that an ASCT now or later make no difference to an MMers overall survival. Your oncologist should understand if you tell him/her to wait. I can send you the study that confirms this.
Lastly, there are a host of evidence-based therapies (nutrition, supplementation, lifestyle, etc.) that are anti-mm. I have remained in complete remission for years by living an evidence-based, non-toxic, anti-mm lifestyle.
The bottom line is that you can take your treatment one step at a time. There is no benefit to having an ASCT now.
Let me know if you have any questions.
Hang in there,
David Emerson
Reply

