- You are here:
- Home »
- Blog »
- Uncategorized »
- Tamoxifen – Prevent breast cancer in menopausal women?
Tamoxifen – Prevent breast cancer in menopausal women?
“…tamoxifen can save lives and decrease medical costs when taken by menopausal women under 55 years of age as a preventive measure against breast cancer.”
A new study based upon a mathematical model using “simulated 5-year trials” “concludes that tamoxifen can save lives and decrease medical costs when taken by menopausal women under 55 years of age as a preventive measure against breast cancer.”
No real trial was conducted. I have difficulty trusting a mathematical model. I have difficulty factoring in its cost-effectiveness as a reason to take it.
Even assuming their conclusions are correct, there are problems. The average age of menopause in the United States is 51. The authors are talking about virtually every woman using Tamoxifen at menopause. However, one is never quite sure when menopause has arrived. Hormone levels often fluctuate during the premenopausal years. Hormone levels can be tested but I am fairly certain that this is not routinely done. I assume that, in order to maintain the cost-effectiveness, they would have to choose an average age to begin Tamoxifen and that would likely alter the conclusions of their mathematical model.
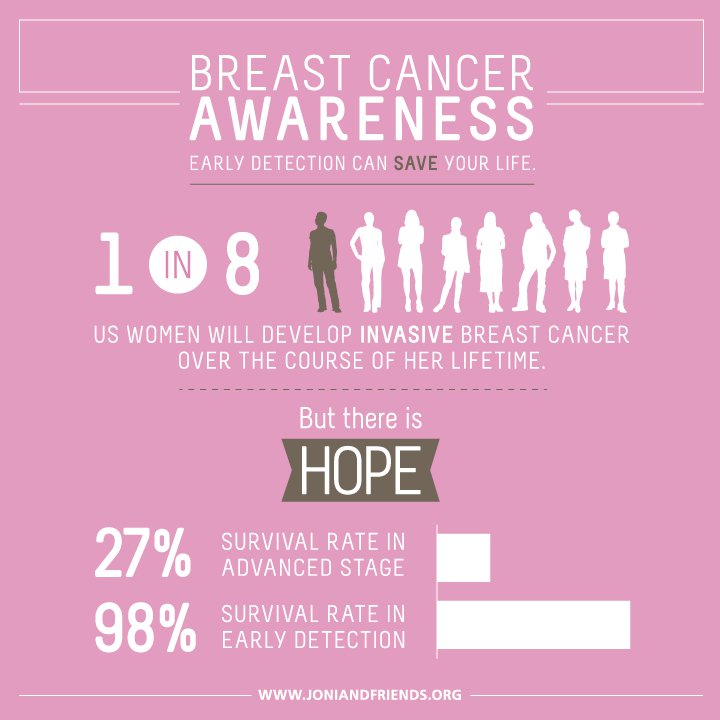
The part about saving lives is interesting. How many people would have to take Tamoxifen in order to save a life?
I would only do such a thing if I had an extremely high chance of getting breast cancer. Other women may feel differently and be willing to risk “thromboembolic” events, cataracts, and higher susceptibility to endometrial cancer” as well as the many less life-threatening side effects such as fatigue, hot flashes, night sweats, vaginal discharge and mood swings, to potentially avoid getting breast cancer.
Tamoxifen can be a life-saving drug. It has an important place in the treatment of breast cancer. Do we really want to recommend that it be taken prophylactically by millions of women?
Mary Miller- Breast Cancer Profile in Courage
Should tamoxifen be used in breast cancer prevention?
“Breast cancer is the most commonly diagnosed cancer in women. The risk of developing breast cancer can be lowered by maintaining a healthy body weight and avoiding long-term use of combined estrogen and progestogen replacement after menopause.
However, many women are at an increased risk of developing breast cancer secondary to age, early menarche, a family history of breast cancer or a personal history of benign breast disease. These women may now be offered tamoxifen as a chemoprevention therapy.
Five years of tamoxifen treatment results in a reduction in the relative risk of developing estrogen receptor-positive breast cancer of 48%. This benefit outweighs the risk of tamoxifen-related adverse events for many healthy women.
However, the benefit-risk ratio of tamoxifen chemoprevention varies for individual women. The randomized clinical trials evaluating standard-dose tamoxifen versus placebo as chemoprevention therapy are reviewed and analyzed to determine which particular women are most likely to benefit and least likely to experience a tamoxifen-related adverse event.
Tamoxifen decreases the risk of breast cancer associated with aging, having a first-degree relative with the disease, and a personal diagnosis of atypical ductal hyperplasia or lobular carcinoma in situ. Women who have had a hysterectomy and are at low risk of a thromboembolic event have a decreased risk of adverse effects associated with tamoxifen therapy.
The strengths and weaknesses of the Gail model (frequently used to assess an individual’s risk of developing invasive breast cancer over the next 5 years) are highlighted. A method for assessing the benefit-risk ratio for an individual woman is presented. Alternative breast cancer chemoprevention strategies are considered, including the use of aromatase inhibitors. This article discusses the pros and cons of these various preventive therapies and concludes that at this time, tamoxifen remains the gold standard for breast cancer prevention.
Cost-effectiveness of chemoprevention of breast cancer using tamoxifen in a postmenopausal US population.
“Previous cost-effectiveness analyses of tamoxifen therapy account for breast cancer risk reduction during active treatment but not for its persistent protective effect after active treatment…
Results: Tamoxifen treatment (vs no treatment) saved 29 QALYs in a population of 1000 postmenopausal women aged <55 years with an additional cost of $333,000 over the population’s lifetime (average cost-effectiveness ratio, $11,530 per QALY). Tamoxifen therapy, compared with no treatment, was cost saving when higher risk populations were targeted (5-year risk ≥1.66%). The cost-effectiveness results were sensitive to parameters that characterized menopausal symptoms and adverse side effects of tamoxifen.
CONCLUSIONS: The current results indicated that tamoxifen chemoprophylaxis for postmenopausal women aged <55 years is a cost-effective health policy that reduces breast cancer incidence and improves life expectancy. Focusing on a postmenopausal population aged <55 years minimized the threat of adverse events associated with tamoxifen.”