“I was in a very emotional state at the time (of my breast cancer diagnosis) and can only imagine the fear and uncertainty a second operation would have created for me and my family.”
A new observational study of 2206 women who had lumpectomies for invasive breast cancer at four different institutions reveals that 509 of them had second operations in attempts to achieve wider clear margins, or in some cases to achieve cancer free margins. The procedure is called re-excision. That seems like a very high number, but some doctors had much higher rates
The conclusion is that “substantial surgeon and institutional variation were observed in re-excision following [lumpectomy] in women with invasive breast cancer.”
The study does not reveal if there were attempts during the original surgeries to determine that the margins were clear or sufficient, thus reducing the chances that a second operation would have to be done at a later time. The writers do say that they were not able to evaluate whether the surgeons had utilized something called “intraoperative assessment of margins.” I would like to think that this would always be done, but this statement implies that it may not. I have been unable to find out for sure. I did find several studies about new devices that are being created to help in evaluating margins during breast cancer surgery. I hope they will help.
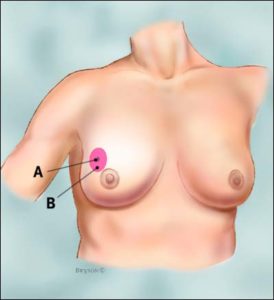
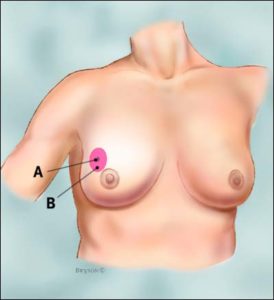
In my 2003 breast cancer surgery they discovered one margin of less than 0.05 mm in thickness close to the chest wall. Because of this they apparently paused during the surgery and had what is listed on the pathology report as an “Intraoperative Consultation.” They then did a re-excision and found the re-excised tissue to be “unremarkable” and the later final pathology report found it to be free of cancer.
My surgeon obviously did do an intraoperative assessment of the margins. I do not know if this required a radiologist or a pathologist to be on the surgical team or how much extra time this might have taken. Whatever it required, I am very grateful that I did not have to return for a second lumpectomy. I was in a very emotional state at the time and can only imagine the fear and uncertainty a second operation would have created for me and my family.
Maybe all breast surgeons do intraoperative assessment of the margins and later, in a large number of cases, still believe additional surgery is required. I do know that I would want to know beforehand if my surgeon would be doing such an assessment and if what he considered to be an adequate clear margin.
It turns out that breast surgeons have considerable disagreement about what constitutes an acceptable margin, and how much difference the size of the clear margin makes regarding survival. This is yet another unknown that makes decision making so difficult for the new breast cancer patient.
Mary Miller- Breast Cancer Profile In Courage
Recommended Reading:
Context Health care reform calls for increasing physician accountability and transparency of outcomes. Partial mastectomy is the most commonly performed procedure for invasive breast cancer and often requires reexcision. Variability in reexcision might be reflective of the quality of care…
Results A total of 2206 women with 2220 invasive breast cancers underwent partial mastectomy and 509 patients (22.9%; 95% CI, 21.2%-24.7%) underwent reexcision (454 patients [89.2%; 95% CI, 86.5%-91.9%] had 1 reexcision, 48 [9.4%; 95% CI, 6.9%-12.0%] had 2 reexcisions, and 7 [1.4%; 95% CI, 0.4%-2.4%] had 3 reexcisions). Among all patients undergoing initial partial mastectomy, total mastectomy was performed in 190 patients (8.5%; 95% CI, 7.2%-9.5%). Reexcision rates for margin status following initial surgery were 85.9% (95% CI, 82.0%-89.8%) for initial positive margins, 47.9% (95% CI, 42.0%-53.9%) for less than 1.0 mm margins, 20.2% (95% CI, 15.3%-25.0%) for 1.0 to 1.9 mm margins, and 6.3% (95% CI, 3.2%-9.3%) for 2.0 to 2.9 mm margins. For patients with negative margins, reexcision rates varied widely among surgeons (range, 0%-70%; P = .003) and institutions (range, 1.7%-20.9%; P < .001). Reexcision rates were not associated with surgeon procedure volume after adjusting for case mix (P = .92).
“Conclusion Substantial surgeon and institutional variation were observed in reexcision following partial mastectomy in women with invasive breast cancer…”