Diagnosed 5/12/12. Surgery, radiation, etc. Then induction, collection, but no SCT. On maintenance. Not in full remission — but close. 10 mg Revlimid and Zometa infusions.
I underwent a right total hip in Feb. ’14. Went off Revlimid 2 weeks pre-op (aspirin too). Resumed it 2 weeks after OR. (Aspirin too) 54 years young.
Zimmer device. Stainless nail with combo cup (ceramic and nylon). Orthopod and PA both said bone was like concrete — just no cartilage left / head of femur had worn into an egg, instead of a cue ball. No myeloma lesions.
For coagulation issues, I was placed on Xarelto for 3 weeks. Switched back to Revlimid 10 mg / aspirin 81 grain daily.
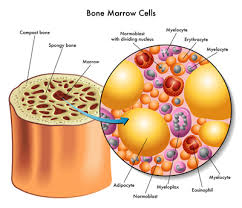
Only problem has been bone healing. Revlimid (IMID) acts like a “beat cop” — swinging a night-stick at teenagers. He chases off the RBC’s (teenagers) accumulating around the device, so the bone matrix formation has been very slow to develop around the nail / acetablum. Functionally, I’m doing okay — albeit, I have not pushed things.
On extra calcium, etc. Zometa, still ( every 3 months, now).
At 6 month check: Great placement of nail, acetablum, screws, etc--but very little bone formation around nail / acetablum. Coming up on 1 yr–in Feb. Hopefully we will then see callous formation/ bone matrixes, bone growth around nail / acetablum.