
Diagnosed with Cancer? Your two greatest challenges are understanding cancer and understanding possible side effects from chemo and radiation. Knowledge is Power!
Learn about conventional, complementary, and integrative therapies.
Dealing with treatment side effects? Learn about evidence-based therapies to alleviate your symptoms.
Click the orange button to the right to learn more.
- You are here:
- Home »
- Blog »
- side effects ID and prevention »
- GERD and Diet
GERD and Diet
Gastroesophageal Reflux Disease, GERD and diet- what you eat, day in, day out, makes a difference in your risk of Barrett’s Esophagus (BE) and your risk of Esophageal Cancer (EC).
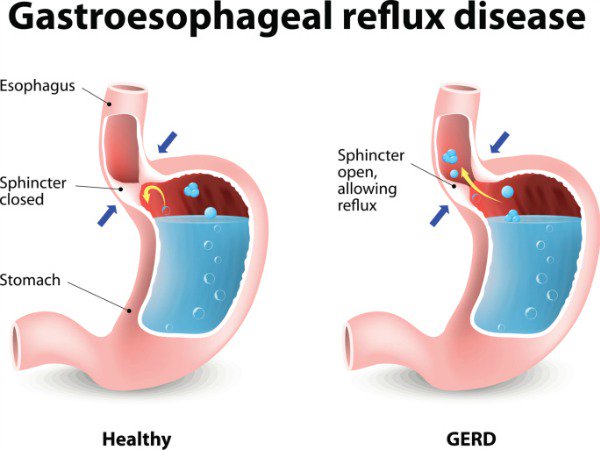
As the first article linked and excerpted below states, “GERD occurs when the contents, especially acid, of the stomach back up into the esophagus, leading to symptoms or lesions of the esophageal mucosa.” Therefore, every time you feel that burning, your stomach contents are causing lesions of the esophageal mucosa.
I am a long-term cancer survivor with a side effect called radiation-induced dysphagia. Radiation to my neck due to my cancer and damaged my neck muscles. This damage weakened the sphincter at the juncture of my esophagus and stomach. As a result of the weakened sphincter, if I’m not careful, stomach acids will enter my esophagus and cause GERD.
Experience has taught me that prevention is preferable to trying to cure problems once they occur. While I can feel stomach acid entering my esophagus once-in-a-while, preventing this feeling and damage is preferable.
My point is GERD and diet is an important therapy. I think the articles below will teach GERD patients a lot about what to eat and what not to eat.
Do you have GERD? If you’d like to learn more about both conventional and non-conventional therapies send me an email at David.PeopleBeatingCancer@gmail.com
Hang in there,
David Emerson
- Cancer Survivor
- Cancer Coach
- Director PeopleBeatingCancer
How Does Diet Affect Gastroesophageal Reflux Disease?
“What dietary recommendations are appropriate for gastroesophageal reflux disease (GERD)? While 85% of patients identify at least one food associated with reflux symptoms, misconceptions about diet in GERD are widespread…
GERD occurs when the contents, especially acid, of the stomach back up into the esophagus, leading to symptoms or lesions of the esophageal mucosa.
…several hygienic-dietary rules are integrated into the therapeutic management of GERD. Some, such as elevating the head of the bed and allowing a 2- to 3-hour gap between meals and bedtime, have proven effective.
Diet and obesity also play a role in the onset of GERD symptoms. Thus, hygienic-dietary rules are an integral part of current recommendations.
“Weight loss is effective in reducing reflux symptoms and should be recommended,” stated Frank Zerbib, MD, head of Hepatology, Gastroenterology, and Digestive Oncology at University Hospital of Bordeaux in France, during the presentation.”
Furthermore, most patients with GERD identify foods that may trigger their symptoms, even if there is no evidence to support this in the literature. However, it has been shown that reducing the consumption of these foods is effective…
Caloric Intake and Lipid Content
A high-calorie meal slows gastric emptying, thus prolonging gastric distension, reducing LES tone, and promoting the onset of TLESRs. Several studies have emphasized that at equivalent caloric intake, lipid composition has no impact on LES tone and the number of TLESRs in healthy patients or those with GERD. However, with equivalent caloric intake, and thus equivalent acid exposure, the presence of lipids in the meal increases the perception of reflux. This “reflux hypersensitivity” effect induced by lipids is caused by the endogenous release of CCK and its action on vagal afferents. This effect also is observed in the perception of functional dyspepsia symptoms.
Several studies have established a correlation between saturated fat consumption and the presence of GERD symptoms.
The Role of Carbohydrates
While the protein component of a meal has little impact on esophagogastric physiology, carbohydrates produce effects on esophagogastric motility that are mediated by their fermentation products, especially short-chain fatty acids (SCFAs), which are synthesized in the colon. Colonic perfusion of these SCFAs leads to fundus relaxation, reduced LES tone, and increased TLESRs. Moreover, in patients with GERD, adding prebiotics (fructo-oligosaccharide) to the meal content increases the number of TLESRs, acid reflux, and symptoms by amplifying colonic fermentation and SCFA production.
Several studies have evaluated low-carbohydrate diets in GERD. A small study of eight patients with morbid obesity on a very low–carbohydrate diet observed benefits on symptoms and esophageal acid exposure in pH probe testing.
A randomized French study of 31 patients with refractory GERD found no significant difference between a low fermentable oligo-, di-, monosaccharides, and polyols diet and usual dietary advice.
A recent American study of 95 veterans found an improvement in pH in the group reducing simple sugars but symptomatic improvement in all groups reducing sugar consumption in general.
Therefore, based on all these data, according to Zerbib, “high-calorie meals, rich in fats or carbohydrates, promote the onset of reflux episodes and their perception. Diets low in fats and carbohydrates should be recommended…”
Acid Reflux Diet: 8 Foods to Avoid & Eat
“8 Foods to Avoid With Acid Reflux
Acid reflux foods to avoid:
- Chocolate — Everyone’s favorite treat comes with a dark side; chocolate contains caffeine, cocoa, and plant chemicals that can all trigger heartburn. Also, a chemical in cocoa relaxes the LES, making it easier for stomach contents to leak into your esophagus.
- Peppermint — Known for soothing an irritable bowel, peppermint has the opposite effect on acid reflux. Peppermint relaxes the muscles used for digestion, and a relaxed LES is a leaky LES.
- Fatty foods — If you feel like fatty foods make you sluggish, you’re right. They relax your LES and are slower to digest than other foods. When food sits in your stomach longer, your body responds by making more acid. Fried foods like onion rings are obvious culprits, but meats like prime rib or bacon, and whole milk dairy products also cause symptoms.
- Spicy foods — Spicy foods make acid reflux worse in two ways. First, the capsaicin in many spicy foods can slow digestion. But before it even gets that far, it can irritate an already irritated esophagus on its way down.
- Acidic foods and drinks — Acidic foods are common triggers of acid reflux. Foods like citrus fruits and juices, tomatoes and tomato products, pineapple, and vinaigrette salad dressings all have a high acid content, contributing to an already acidic environment.
- Garlic — Garlic, especially raw, is known to cause heartburn and upset stomach in healthy people. That makes it even more likely to cause issues for those who suffer from acid reflux.
- Onions — Raw onions don’t just make you cry; they stimulate acid production. That extra acid puts you at risk for heartburn.
- Drinks containing alcohol, caffeine, or carbonation — Alcohol and caffeine both relax the LES, allowing acid to leak up your esophagus. The bubbles in carbonation expand your stomach, pushing stomach contents up against the LES. That makes soda, coffee and tea, and alcoholic beverages all triggers. Be especially careful with mixed drinks, which could combine triggers.
8 Foods That Help Acid Aeflux
Here is a list of foods to eat with acid reflux:
- Vegetables and non-citrus fruits — Aside from the “bad” foods listed above, nearly all fruits and vegetables help reduce stomach acid. They’re also low fat, low sugar, and provide fiber and important nutrients. Bananas, melons, broccoli, asparagus, and green beans are low in acid and known to reduce stomach acid levels.
- Whole grains — High fiber, whole-grains like brown rice, oatmeal, and whole-grain breads help stop symptoms. They are a good source of fiber and may help absorb stomach acid, reducing the risk of symtoms.
- Lean protein — Low-fat, lean sources of protein also reduce symptoms of acid reflux. Good choices are chicken, seafood, tofu, and egg whites. The best ways to prepare them are baked, broiled, poached, or grilled.
- Beans, peas, and lentils — Along with being good sources of fiber, beans, peas, and lentils also provide protein, vitamins and minerals.
- Nuts and seeds — Many nuts and seeds provide fiber and nutrients and may help absorb stomach acid. Almonds, peanuts, chia, pomegranate, and flaxseeds are all healthy choices.
- Yogurt — Not only is yogurt soothing to an irritated esophagus, but it provides probiotics that support your digestive tract. It’s also good source of protein.
- Healthy fats — Fat is a necessary nutrient but eating too many fatty foods can trigger symptoms. Replacing unhealthy fats with unsaturated fats can help. Avocados, olive oil, walnuts, and soy products are good choices for healthy fats.
- Ginger — Ginger has anti-inflammatory properties and has been used throughout history for gastrointestinal problems. Ginger can be added to smoothies, soups, stir fry, or other dishes, or steeped as a tea.

