
Diagnosed with Cancer? Your two greatest challenges are understanding cancer and understanding possible side effects from chemo and radiation. Knowledge is Power!
Learn about conventional, complementary, and integrative therapies.
Dealing with treatment side effects? Learn about evidence-based therapies to alleviate your symptoms.
Click the orange button to the right to learn more.
- You are here:
- Home »
- Blog »
- side effects ID and prevention »
- Cardiotoxicity Prevention
Cardiotoxicity Prevention
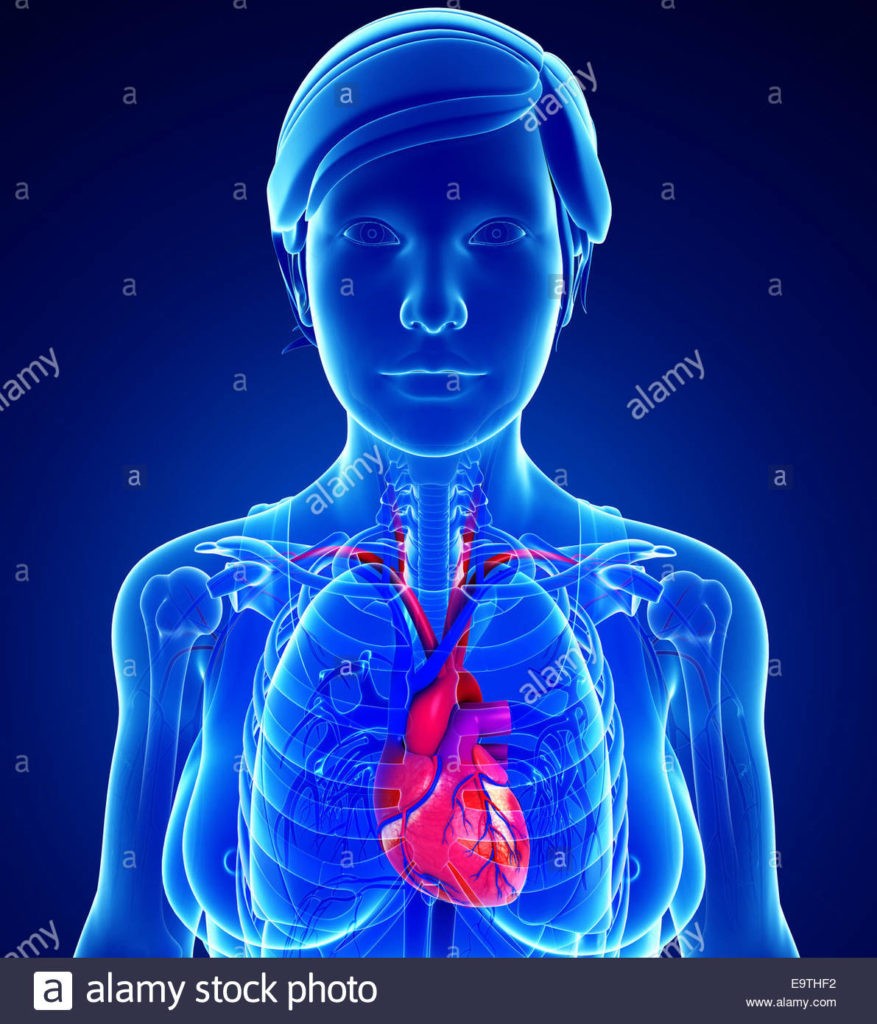
Cardiotoxicity prevention is particularly important to me. I am a long-term cancer survivor who developed chemotherapy-induced cardiomyopathy and chronic atrial fibrillation in late 2010- fully 15 years AFTER undergoing several different known cardiotoxic chemotherapy regimens.
As both a cancer survivor and cancer coach, I have to operate with the belief that chemotherapy and radiation, at least in low doses, are necessary to manage cancer.
This being the case, cardiotoxic prevention is essential for all cancer patients undergoing either/or/both cardiotoxic chemo regimens and radiation anywhere near the heart.
I have never understood how the FDA can approve a cancer therapy as “safe and effective.” More to the point, I cannot understand how my oncologists Dr. Berger and Dr. Lazarus prescribed multiple cardiotoxic regimens while knowing that there was a good chance I would develop heart damage that could potentially kill me.
The study linked below studies short-term cardiotoxicity prevention. It is important to understand that:
- a percentage of patients undergoing cardiotoxic therapies will develop heart damage immediately-
- a percentage of patients will develop heart damage within a few years post therapy administration-
- and a percentage of patients, like me, will develop heart damage years after undergoing cardiotoxic chemo regimens-
First, do no harm?
What FDA approved cancer therapies can damage the patient’s heart?
- Anthracyclines: Drugs like doxorubicin, daunorubicin, and epirubicin are commonly used in chemotherapy for various cancers. They are effective against cancer cells but can also cause damage to the heart muscle, leading to conditions like cardiomyopathy and heart failure.
- Trastuzumab (Herceptin): This targeted therapy is used to treat breast cancer that is HER2-positive. While effective against cancer, trastuzumab can sometimes lead to heart problems, including heart failure.
- Tyrosine kinase inhibitors (TKIs): Drugs like imatinib, sunitinib, and dasatinib are used to treat certain types of leukemia and other cancers. They can sometimes cause heart problems such as hypertension, heart failure, and heart rhythm disturbances.
- Immune checkpoint inhibitors: Drugs like pembrolizumab, nivolumab, and ipilimumab are immunotherapy agents used to treat various cancers. While they boost the immune system’s ability to fight cancer, they can also lead to immune-related adverse events, including inflammation of the heart muscle (myocarditis) and other cardiac issues.
- Proteasome inhibitors: Drugs like bortezomib and carfilzomib are used to treat multiple myeloma and some other cancers. They can sometimes cause heart rhythm disturbances and heart failure.
- Radiation therapy: While not a drug, radiation therapy aimed at treating cancer can also inadvertently damage the heart, particularly when the tumor is located near the heart. This can lead to conditions such as coronary artery disease, pericarditis, and cardiomyopathy.
Possible non-conventional therapies for cardiotoxicity prevention
- Meditation and Mindfulness: Practices like meditation and mindfulness can reduce stress, lower blood pressure, and improve overall cardiovascular health. They promote relaxation and may help in managing risk factors associated with heart disease.
- Yoga: Yoga combines physical postures, breathing exercises, and meditation. It has been associated with lower blood pressure, improved lipid profiles, and reduced stress levels, all of which contribute to heart health.
- Acupuncture: Some studies suggest that acupuncture may help lower blood pressure and reduce inflammation, both of which are beneficial for heart health. It’s also believed to help regulate the autonomic nervous system, which influences heart function.
- Tai Chi: This mind-body practice involves slow, gentle movements along with deep breathing and meditation. Tai Chi has been shown to improve cardiovascular fitness, lower blood pressure, and reduce stress.
- Music Therapy: Listening to music, particularly soothing or calming music, has been associated with lower heart rates and blood pressure. Music therapy may also help reduce anxiety and improve mood, indirectly benefiting heart health.
- Aromatherapy: Certain essential oils, such as lavender and rosemary, have been linked to relaxation and stress reduction. Using aromatherapy techniques may help manage stress levels, which can have a positive impact on heart health.
- Herbal Supplements: Some herbal supplements, such as garlic, hawthorn, and turmeric, have been studied for their potential cardiovascular benefits. However, it’s important to use caution and consult with a healthcare professional before taking any herbal supplements, as they may interact with medications or have side effects.
- Massage Therapy: Regular massage therapy may help reduce stress, promote relaxation, and improve circulation, all of which can contribute to better heart health.
- Chiropractic Care: While primarily known for treating musculoskeletal issues, chiropractic adjustments may also positively influence the autonomic nervous system, which regulates heart function. Some individuals report improvements in blood pressure and overall well-being with regular chiropractic care.
- Biofeedback: Biofeedback techniques teach individuals to control physiological processes such as heart rate and blood pressure using relaxation and mental imagery. Learning to manage these processes can help reduce stress and improve heart health.
Research and personal experience has taught me that cancer patients should adopt a complementary approach to their therapy. In the case of cardiotoxicity prevention, that would mean combining conventional therapies that your oncologist prescribes with non-conventional therapies such as heart healthy nutrition, moderate exercise and those therapies listed above.
Are you a cancer patient who is about to undergo chemo or radiation? Or are you a cancer survivor who has developed chemotherapy-induced cardiomyopathy or AFib?
If you are interested in learning more about both convention and non-conventional cancer management email me at David.PeopleBeatingCancer@gmail.com
Hang in there,
David Emerson
- Cancer Survivor
- Cancer Coach
- Director PeopleBeatingCancer
PROACT: Do ACE Inhibitors Help Prevent Cardiotoxicity in Patients Treated For Breast Cancer or Lymphoma?
“To determine whether ACE inhibitors could help to prevent anthracycline cardiotoxicity (cardiotoxicity prevention), researchers conducted a multicenter, open-label trial which randomized 111 patients (average age 57 years, 78% women, 98% White British) undergoing treatment for breast cancer (62%) or non-Hodgkin lymphoma (38%) to enalapril or placebo at 13 sites in the U.K. All patients had negative troponin results at the start of the study and were due to receive six cycles (≥300 mg/m2 doxorubicin equivalent) of anthracycline chemotherapy…
Results of the PROACT trial found there was no significant between-group difference in the primary endpoint of the proportion of patients who experienced a troponin T release, which occurred in 77.8% of the enalapril group and 83.3% of the standard of care group (adjusted odds ratio, 0.65; p=0.405). Additionally, there was no significant difference between groups in terms of troponin I…
Based on the findings, researchers said ACE inhibitors are not likely to play a role in future cardiotoxicity prevention efforts associated with anthracyclines. “The field probably needs to find another [drug] candidate before starting again on another preventative study,” said Austin.”
Understanding Troponin, an Important Protein
“Troponins are proteins released into the bloodstream if there’s heart damage. Lab results below the 99th percentile mean normal function. Higher levels could mean a heart attack or another cardiac problem…
With a conventional troponin test, it can take hours before increased levels of troponin are detectable. Using this test too soon can produce a false negative…
Troponin proteins help regulate muscle contraction. They’re split into three subunits:
- troponin C (TnC), which binds to calcium, initiates muscle contraction, and helps move TnI
- troponin I (TnI), which works with TnC to pull the muscle fibers
- troponin T (TnT), which anchors the troponin proteins to a separate protein called tropomyosin
Troponin tests measure levels of either TnI or TnT…
Troponin levels are measured in nanograms per milliliter (ng/mL). High-sensitivity tests measure troponin levels in nanograms per liter (ng/L).
Normal levels fall below the 99th percentile in the blood test. If troponin results are above this level, it may indicate heart damage or heart attack. Reference ranges for troponin levels will vary by test lab…



