
Diagnosed with Cancer? Your two greatest challenges are understanding cancer and understanding possible side effects from chemo and radiation. Knowledge is Power!
Learn about conventional, complementary, and integrative therapies.
Dealing with treatment side effects? Learn about evidence-based therapies to alleviate your symptoms.
Click the orange button to the right to learn more.
- You are here:
- Home »
- Blog »
- Skin Cancer »
- Malignant Melanoma-Stage Dictates Prognosis
Malignant Melanoma-Stage Dictates Prognosis
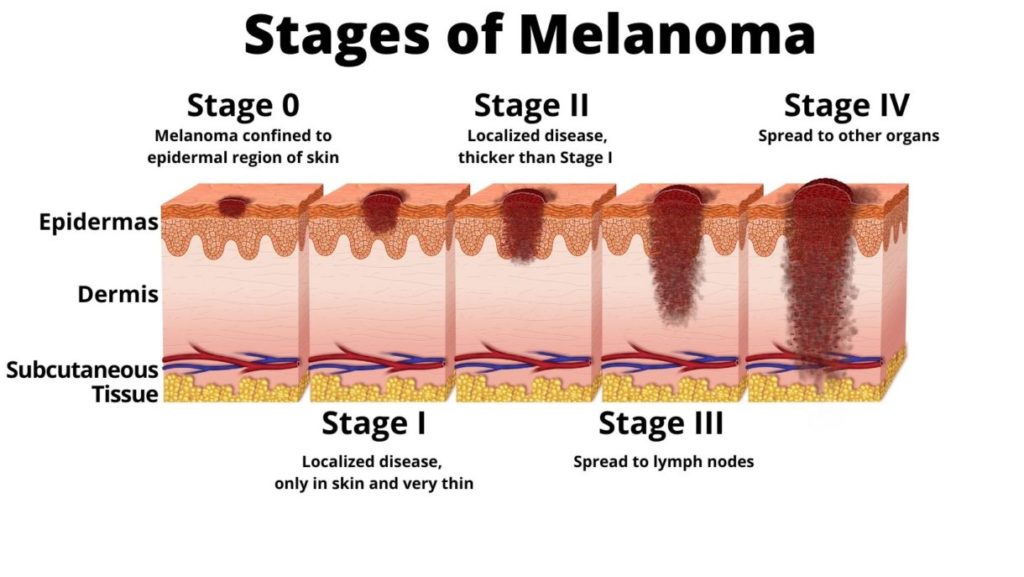
Your Stage of Melanoma at Diagnosis Will Guide Your Treatment Decisions
A diagnosis of skin cancer is difficult. A diagnosis of melanoma, just plain melanoma, is more difficult. And a diagnosis of malignant melanoma may be the worst of all cancer diagnoses. I said “may be” as in this diagnosis could be the worst depending on your stage at diagnosis.
Melanoma at a glance-
The world of skin cancer is wide and complex. To be fair, I cannot blame you for not listening to whatever your oncologist has to say after he/she says “you have skin cancer.” But keep in mind that your diagnosis can run the gamut, according to the study linked and excerpted below from a five-year survival rate of over 90% to less than 10% depending on your stage at diagnosis.
I am a long-term cancer survivor and cancer coach. I field questions from cancer patients, survivors and caregivers daily. The majority of questions I’m asked are from cancer patients who don’t know their stage at diagnosis.
The combination of therapies for malignant skin cancer- both conventional (FDA approved) and evidence-based but not FDA approved, is extensive. The five-year survival averages listed below take into account only conventional therapies. Not evidence-based Integrative, Complementary and Botanical therapies.
Have you been diagnosed with either melanoma or non-melanoma skin cancer? Scroll down the page, post a question or a comment and I will reply ASAP.
Thank you
David Emerson
- Cancer Survivor
- Cancer Coach
- Director PeopleBeatingCancer
Recommended Reading:
- Non-Melanoma Skin Cancer Risk Increases From Radiation
- Preventing Non-Melanoma Skin Cancer Relapse
- How to Identify Skin Cancer in 5 Steps
- Skin Cancer, Vitamin D3 and Sunlight
Malignant Melanoma Staging
-
“Stage IA:
-
Lesions ≤1 mm in thickness with no evidence of ulceration or metastases (T1aN0M0) are associated with a 5-y survival rate of ~97%
Stage IB:
-
Lesions ≤1 mm in thickness with ulceration noted but without lymph node involvement (T1bN0M0) or lesions 1.01-2 mm in thickness without ulceration or lymph node involvement (T2aN0M0) are associated with a 5-y survival rate of ~92%
Stage IIA:
-
Melanomas >1 mm but ≤2 mm in thickness with no evidence of metastases but with evidence of ulceration (T2bN0M0) or lesions 2.01-4.0 mm in thickness without ulceration or lymph node involvement (T3aN0M0) are associated with an overall 5-y survival rate of ~81%
Stage IIB:
-
Melanomas 2.01-4 mm in thickness with ulceration but no lymph node involvement (T3bN0M0) or lesions >4 mm in thickness without ulceration or lymph node involvement (T4aN0M0) are associated with a 5-y survival rate of ~70%
Stage IIC:
-
Lesions >4 mm in thickness with ulceration but no lymph node involvement (T4bN0M0) are associated with a 5-y survival rate of ~53%
Stage IIIA:
-
Patients with any-depth lesion, no ulceration, and 1 positive (micrometastatic) lymph node (T1-4aN1aM0) have a 5-y survival rate of ~70%
-
T1-4aN2aM0 lesions (any-depth lesion, no ulceration, but 2-3 nodes positive for micrometastasis) are associated with a 5-y survival rate of 63%
Stage IIIB:
-
Patients with any-depth lesion, positive ulceration, and 1 lymph node positive for micrometastasis (T1-4bN1aM0) or 2-3 nodes positive for micrometastasis (T1-4bN2aM0) have a 5-y survival rate of 50-53%
-
Patients with any-depth lesion, no ulceration, and 1 lymph node positive for macrometastasis (T1-4a, N1b, M0) or 2-3 nodes positive for macrometastasis (T1-4aN2bM0) have a 5-y survival rate of 46-59%
Stage IIIC:
-
Patients with any-depth lesion, positive ulceration, and 1 lymph node positive for macrometastasis (T1-4bN1bM0); 2-3 nodes positive for macrometastasis (T1-4bN2bM0); or ≥4 metastatic lymph nodes, matted lymph nodes, or in-transit met(s)/satellite(s) have a 5-y survival rate of ~40%
Stage IV:
-
Melanoma metastatic to skin, subcutaneous tissue, or lymph nodes with normal LDH level (M1a) is associated with a 5-y survival rate of ~15%-20%
-
M1b disease (metastatic disease to lungs with normal LDH level) has a 5-y survival rate of 7%
-
M1c disease (metastatic disease to all other visceral organs and normal LDH level or any distant disease with elevated LDH level) is associated with a 5-y survival rate of 10%
Mitotic rate assessment
For mitotic rate assessment, the pathologist counts the number of cells in a certain amount of melanoma tissue that are in the process of dividing. A higher mitotic rate means that the cancer is more likely to grow and spread. The mitotic rate is used to stage thin melanoma.

