Recently Diagnosed or Relapsed? Stop Looking For a Miracle Cure, and Use Evidence-Based Therapies To Enhance Your Treatment and Prolong Your Remission
Multiple Myeloma an incurable disease, but I have spent the last 25 years in remission using a blend of conventional oncology and evidence-based nutrition, supplementation, and lifestyle therapies from peer-reviewed studies that your oncologist probably hasn't told you about.
Click the orange button to the right to learn more about what you can start doing today.
- You are here:
- Home »
- Blog »
- Multiple Myeloma »
- MRD After Induction- ASCT?
MRD After Induction- ASCT?
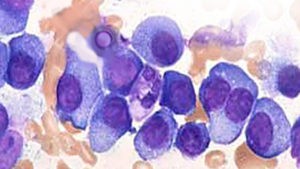
If you have been diagnosed with multiple myeloma (MM) and you undergo bortezomib (velcade), lenalidomide (revlimid) and dexamethasone (VRd) according to the study linked below, you have a 29% chance of reaching minimal residual disease negative (MRD) status.
If you reach MRD- status after your induction therapy, the question you have to ask yourself, your caregiver and your oncologist is “will more chemotherapy give me a higher quality of life and a longer length of life (longer overall survival)?
The answer to the first part of this question has got to be no. More toxicity will almost certainly cause more short, long-term and late stage side effects which usually means a reduced quality of life.
The answer to the second question, will more therapy mean a longer overall survival, can only be answered by evidence-based research. My understanding is that once a MM patient reaches MRD- status, he/she then has the greatest chances for the longest length of life aka OS.
Conventional oncology makes a lot of money from autologous stem cell transplants. Your oncologist may resist the idea of you not having an ASCT.
But if you reach MRD- after induction therapy only, my belief is that you are doing well. More toxicity may not help and it certainly can hurt.
One bad cell for every million good cells is a tiny amount of MM in your blood. More toxic chemotherapy has not been shown to improve the average overall survival rates. MM patients don’t live longer on average, if they undergo more chemotherapy after they reach MRD- status.
The key to overall survival, in my experience, are the many evidence-based, non-toxic therapies that you can follow after you reach MRD- status.
To learn more about evidence-based, non-toxic therapies shown to be cytotoxic (kill) multiple myeloma, scroll down the page, post a question or comment and I will reply to you ASAP.
Hang in there,
David Emerson
- MM Survivor
- MM Cancer Coach
- Director PeopleBeatingCancer
Recommended Reading:
- MRD Testing Cheaper Than Multiple Myeloma Maintenance Therapy!
- Medicare Covers MRD Test for Multiple Myeloma
- “MRD is the Goal in Multiple Myeloma” Dr. Raphael Fonseca
Bortezomib, Lenalidomide, and Dexamethasone as Induction Therapy Prior to Autologous Transplantation in Multiple Myeloma
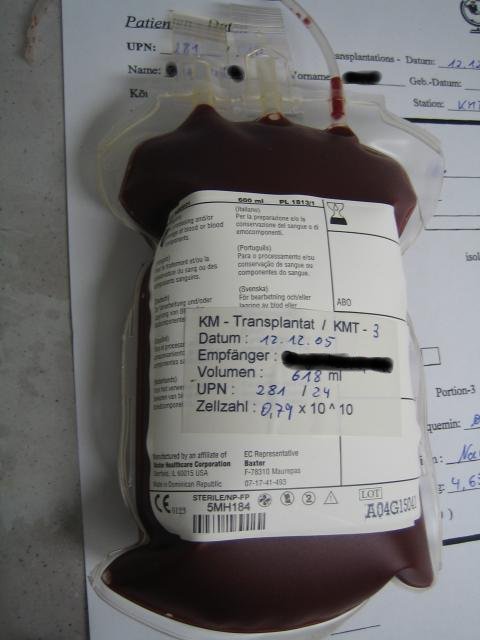
Achieving and maintaining high-quality response is the treatment goal for patients with newly diagnosed multiple myeloma (NDMM). The phase 3 PETHEMA/GEM2012 study, in 458 patients {less than or equal to} 65 years old with NDMM, is evaluating bortezomib (subcutaneous) + lenalidomide + dexamethasone (VRD) for 6 cycles followed by autologous stem cell transplant (ASCT) conditioned with intravenous busulfan + melphalan vs melphalan and posttransplant consolidation with 2 cycles of VRD.
We present grouped response analysis of induction, transplant, and consolidation. Responses deepened over time; in patients who initiated cycle 6 of induction (n = 426), the {greater than or equal to} very good partial response rates were 55.6% by cycle 3, 63.8% by cycle 4, 68.3% by cycle 5, and 70.4% after induction.
The complete response rate of 33.4% after induction in the intent-to-treat (ITT) population, which was similar in the 92 patients with high-risk cytogenetics (34.8%), also deepened with further treatment (44.1% after ASCT and 50.2% after consolidation).
Rates of undetectable minimal residual disease (median 3 × 10−6 sensitivity) in the ITT population also increased from induction (28.8%) to transplant (42.1%) and consolidation (45.2%).
The most common grade {greater than or equal to} 3 treatment-emergent adverse events during induction were neutropenia (12.9%) and infection (9.2%). Grade {greater than or equal to} 2 peripheral neuropathy (grouped term) during induction was 17.0%, with a low frequency of grade 3 (3.7%) and grade 4 (0.2%) events.
VRD is an effective and well-tolerated regimen for induction in NDMM with deepening response throughout induction and over the course of treatment.”