Recently Diagnosed or Relapsed? Stop Looking For a Miracle Cure, and Use Evidence-Based Therapies To Enhance Your Treatment and Prolong Your Remission
Multiple Myeloma an incurable disease, but I have spent the last 25 years in remission using a blend of conventional oncology and evidence-based nutrition, supplementation, and lifestyle therapies from peer-reviewed studies that your oncologist probably hasn't told you about.
Click the orange button to the right to learn more about what you can start doing today.
- You are here:
- Home »
- Blog »
- Multiple Myeloma »
- Multiple Myeloma, CAR-T Cell Therapy and Heart Failure-
Multiple Myeloma, CAR-T Cell Therapy and Heart Failure-

The outcome of interest (for CAR-T Cell patients) included cardiovascular (CV-heart failure) events defined as a combination of arrhythmia, heart failure exacerbation, cardiogenic shock, and CV death.
CAR-T Cell therapy is a source of hope for multiple myeloma patients and survivors. Though the research has been limited thus far, the majority of relapsed/refractory MMers respond to CAR-T cell therapy. The challenge then, is to determine the average length of response for RRMMers and also, at what cost does this response come? Cost being both physical and financial? Does CAR T-cell therapy cause CV aka heart failure?
According to the opinion article and study linked and excerpted below, the physical cost to a patient’s heart might be substantial.
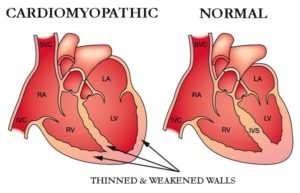
Editor’s Note- I was first diagnosed with MM in early 1994. I was recently diagnosed with chemotherapy-induced cardiomyopathy. The chemotherapy regimens I underwent in 1995 were cardiotoxic. The issue of CAR-T cell therapy being cardiotoxic is near and dear to my heart…
Let’s say that you’ve relapsed several times and your remissions are getting shorter and shorter. You’ve heard great things about the new CAR-T cell therapy. If your oncologist tells you that you can expect, on average an 11 month remission from CAR-T cell therapy therapy, that may sound great.
But then he/she tells you that the chances of heart damage from CAR-T cell therapy is high. And then you read that CAR-T therapy might be as much as $475,000. What do you do?
Please learn about evidence-based but non-conventional, non-toxic therapies shown to limit heart failure among patients undergoing cardio-toxic chemotherapy regimens. Consider CoQ10, curcumin, omega-3 fatty acids, others.
To learn more about triplet therapies for RRMM survivors, scroll down the page, post a question or comment and I will reply to you ASAP.
Thank you,
David Emerson
- MM Survivor
- MM Cancer Coach
- Director PeopleBeatingCancer
Recommended Reading:
- Multiple Myeloma: Car-T Cell Immunotherapy Update
- Cautious Optimism for CAR-T Cell Therapy in Multiple Myeloma
- CAR-T Cell Therapy- One Myeloma Patient’s Experience
Troponin
“…Elevated troponin levels are prognostically important in many of the conditions in which they are used for diagnosis.[29]
In a community-based cohort study indicating the importance of silent cardiac damage, troponin I has been shown to predict mortality and first coronary heart disease event in men free from cardiovascular disease at baseline.[30] …”
The Cardiovascular Effects of Chimeric Antigen Receptor T-Cells
The cytokines might be causing damage to the heart, Raza Alvi, MD, says
“In this study, we evaluated the medication called CAR-T, or chimeric antigen receptor therapy. We studied the cardiovascular effects of this study, and the effect of this medication on the people who are taking CAR-T. This medication is usually a very revolutionary medication because it’s given to patients who relapse regardless of whether they were given chemotherapy and other therapies given for cancer or cancer treatment.
This is a very novel study because there has been no trial done before in adults who received this therapy for cancer treatment. We found basically that the people who were given CAR-T, that after CAR-T, their cardiac troponin levels went up.
We also looked at people who have cytokine-release syndrome, CRS, and we also studied patients who have the cardiovascular events. We found that, interestingly actually, that the people who had all these cardiovascular events, they happen in the people who had positive troponins. Same thing — also with all these people who actually had these events — they happen in the people who had grade two and higher CRS. We wanted to see if there is any connection between the CRS and the cardiac troponins and the cardiovascular events. This is not a part of this study, but a continuation.
We wanted to study the people who receive IL-6 receptor antagonist for the treatment of the CRS. And we wanted to see if that has any effect on the cardiovascular events. We also found out that the people who received this treatment, that there is an effect. We basically found out that people who have the timing between the development of the symptoms of the CRS to the medication given, it was higher, or you can say the duration was longer, and the people who had an event compared with the people who don’t have an event.
Now, saying that, we actually are speculating, in that there’s a possibility that the cytokines released are the result of the CRS — they might be causing damage to the heart, where you already know that they do have a multi-organ effect. So, we think that it might cause damage to the heart, which is also causing the elevation of the troponins, as well as subsequent cardiovascular events.
The clinical implication is that basically what can happen is that if patients who have elevated troponins, if we give the treatment for the IL-6 inhibitor, we might be able to prevent the CRS, as well as the subsequent cardiovascular events. But a limitation for this study is that it is retrospective, it’s a small study. And we would like to have more data, a larger study, and replicate the study in a prospective manner to see if we can replicate the results.
And maybe, when a person has elevated troponins, if we give the treatment before waiting for the person to develop CRS, maybe we can prevent the cardiovascular events in the future.”
THE CARDIOVASCULAR EFFECTS OF CHIMERIC ANTIGEN RECEPTOR T-CELLS
“Methods-We performed a retrospective single center review of all 82 patients who received CAR-T between Jan 2016 and Jun 2018. Cardiovascular testing was performed at the discretion of the primary attending and was not pre-specified. Data of interest included measures of left ventricular ejection fraction and cardiac troponin. The outcome of interest included cardiovascular (CV) events defined as a combination of arrhythmia, heart failure exacerbation, cardiogenic shock, and CV death.
Results-Of the 82 patients,
- 66 (80%) received CAR-T for diffuse large B-cell lymphoma,
- 11 (13%) for multiple myeloma and
- 5 (7%) for other cancers.
The mean age of the cohort was 60±11 years and included 69% males, 8% diabetics, 31% with hypertension, 6% with a history of coronary artery disease, 2% with a history of heart failure (HF), and 5% with a history of arrhythmias.
Among these 82 patients, 36 had troponin measured pre- and post-CAR-T, 21 of the 36 (58%) had a significant increase in troponin with CAR-T. Similarly, 19 of 82 had an echocardiogram pre-and post-CAR-T, of whom 4 had a new reduction in ejection fraction (21%). Patients with a post-CAR-T increase in troponin had higher pre-CAR-T left ventricular (LV) mass, larger LV dimensions and an increased left atrial size compared to those who did not have an increase in troponin with CAR-T.
In follow-up, there were 8 cardiovascular events (10%, new arrhythmias (n=6), and cardiogenic shock leading to death (n=2)). Among patients with cardiovascular events, serum troponin was elevated among all prior to that event.
Conclusion-An elevation is serum troponin is common among patients treated with CAR-T, is associated with pre-existing cardiac structural abnormalities and associated with subsequent cardiovascular events.”