Recently Diagnosed or Relapsed? Stop Looking For a Miracle Cure, and Use Evidence-Based Therapies To Enhance Your Treatment and Prolong Your Remission
Multiple Myeloma an incurable disease, but I have spent the last 25 years in remission using a blend of conventional oncology and evidence-based nutrition, supplementation, and lifestyle therapies from peer-reviewed studies that your oncologist probably hasn't told you about.
Click the orange button to the right to learn more about what you can start doing today.
- You are here:
- Home »
- Blog »
- Multiple Myeloma »
- Myeloma – Heart Damage Risk 300% Higher!
Myeloma – Heart Damage Risk 300% Higher!

“The risk (cardiomyopathy) ranged from about 60% higher in ovarian cancer to over 300% higher in multiple myeloma.”
Certain multiple myeloma chemotherapy regimens are cardio-toxic (damage your heart). According to the study linked below, multiple myeloma chemotherapy increases the risk of heart damage in patients by as much as 300%.
The solution? Less is more. For example, 3-4 rounds of your induction MM chemotherapy offers less risk of heart damage than 5-6 rounds. Talk with your oncologist about it.
If you’ve just been diagnosed with MM and you’re trying to figure out your therapy plan, you’ve got to wonder if the ends justifies the means when it comes to conventional multiple myeloma chemotherapy.
Your oncologist may want to achieve complete remission- an m-spike of 0. But studies don’t prove that complete remission will help you live longer. Yes, you want to control your MM but you must also balance MM chemotherapy with the damage it causes. And more multiple myeloma chemotherapy will definitely increase your risk of heart damage…
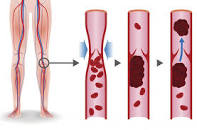
Your increased risk of cardiovascular disease (CVD) in general and cardiomyopathy specifically is in addition to your risk of multiple myeloma (MM) relapse and your risk of a treatment-related secondary cancer. Among other side effect MM patients have to struggle with such as BIPN, endocrine disorders, etc.
Multiple myeloma chemotherapy is toxic and can cause short, long-term and late stage side effects.
I was first diagnosed in early 1994. I underwent SOC therapies until I reached multi-drug resistence (MDR) in 9/97 and was told “there’s nothing more we can do for you…”
CVD in the form of blood clots, atrial fibrillation, and cardiomyopathy all followed over the years.
By wondering if the end justifies the means I am asking if aggressive, expensive, painful therapies (myeloma chemotherapy) that cause short, long-term and late stage side effects are worth it?
To look at this problem differently, let me ask you are question. If you could reduce your risk of short, long-term and late stage side effects, while maintaining a positive prognosis, would you? Even if it means changing your diet, lifestyle, conventional therapy plan, etc?
To Learn More about Chemotherapy-induced Heart Damage- click now
Scroll down the page, post a question or a comment if you would like to learn more.
thanks and hang in there,
David Emerson
- MM Survivor
- MM Cancer Coach
- Director PeopleBeatingCancer
Recommended Reading:
- Living w/ Post-Cancer Fear As a Myeloma Survivor-
- Organic Diet-Fewer Cancer Dx’s, Longer Cancer Survival
- Multiple Myeloma- Tally DVT/VTE Risk Before Revlimid, Thal, Pom, Imnovid
the end justifies the means,
“A good outcome excuses any wrongs committed to attain it. For example, He’s campaigning with illegal funds on the theory that if he wins the election the end will justify the means, or The officer tricked her into admitting her guilt—the end sometimes justifies the means. This proverbial (and controversial) observation dates from ancient times, but in English it was first recorded only in 1583.”
Cancer survivors could be at greater risk of cardiovascular diseases
“…a new study published in The Lancet shows that (multiple myeloma survivors) have a higher risk of cardiovascular disease (CVD) than controls without cancer, due to a number of reasons.
These include the use of chemotherapeutic agents that have direct toxic effects on the heart, the effects of the cancer itself on the blood and vascular system, and risk factors common to both, such as obesity and dietary factors.
A few randomized trials have shown that certain specific CVDs are associated with certain cancer therapies, over the short- to medium-term.
Some observational studies indicated a greater risk of CVDs in people who survived cancer in adolescence and young adulthood compared to age-matched or general population controls. However, not much is known about the absolute increase in risk in cancer survivors as compared to individuals without cancer.
Moreover, the outcome studied in most cases is CVD as a combined outcome, which suggests that only survivors of some cancers have a higher CVD risk.
In contrast, other studies indicate that different cancers are associated with different types of CVD.
The subjects included survivors of the 20 leading cancers which account for over 90% of cancers, and five times as many controls, matched for age and sex. The cancer survivors were classified into 20 groups.
The CVD outcomes observed were:
- Coronary artery disease, including myocardial infarction, angina, revascularization procedures, cardiac arrest
- Stroke, whether ischemic or hemorrhagic
- Cardiac arrhythmia
- Venous thromboembolism (VTE), including pulmonary embolism and deep vein thrombosis
- Cardiac failure and cardiomyopathy
- Pericarditis
- Valvular heart disease
- Disease of the peripheral blood vessels
The study looked at over 100,000 adult cancer patients who had survived at least one year after diagnosis, and more than 520,000 controls. Patients were followed up until one of the following occurred:
- Death
- End of study/ study-associated follow-up
- Any of the study outcomes occurred
The main findings were that in 18 of these cancers, survivors had a 2-9 times higher risk of VTE, or blood clots formed in the veins. The greatest increase was with pancreatic cancer survivors who were at more than 9 times higher risk compared to controls, while prostate cancer patients were at 70% increased risk…
In 10 out of 20 cancers, including blood… the risk of heart failure and cardiomyopathy (permanently weakened heart muscle) was increased. The risk ranged from about 60% higher in ovarian cancer to over 300% higher in multiple myeloma.