- You are here:
- Home »
- Blog »
- Uncategorized »
- Radiation for Breast Cancer- The Risk of Angiosarcoma is Real
Radiation for Breast Cancer- The Risk of Angiosarcoma is Real

…209 (0.1%) of the 184,823 patients who received radiotherapy developed radiotherapy-associated angiosarcoma (RAAS) of the breast and/or chest wall, at a mean latency of 8 years and a median of 6 years.
The risk of radiotherapy-associated angiosarcoma is low. According to the article below, one tenth of a percent. As a long-term cancer survivor who lives with a number of long-term and late stage adverse events aka side effects my advice is as follows: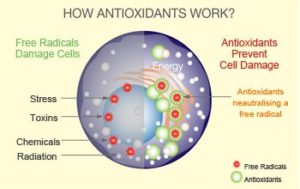
- While the identification of RAAS is important and will enter your “risk/reward” thinking when deciding if your therapy should include radiation, you probably shouldn’t decide against radiation because of RAAS exclusively
- Like other late stage side effects, your risks are real. My advice is to live as anti-relapse, as anti-cancer a lifestyle as you can once you complete your active therapy.
- This means you want to exercise frequently but moderately, eat a nutrious a diet as possible, include those supplements that research has shown are anti-angiogenic and or reduce your risk of breast cancer relapse.

My point is that once we are diagnosed with cancer, any cancer, and choose to undergo toxic therapies, there will be short, long-term and late stage side effects that we have to face. My belief and experience is to minimize those risks through nutrition, supplementation and lifestyle therapies as much as possible.
Scroll down the page and post a question or comment to learn more about evidence-based, non-toxic therapies.
Thank you,
David Emerson
- Cancer Survivor
- Cancer Coach
- Director PeopleBeatingCancer
Recommended Reading:
- Organic Diet-Fewer Cancer Dx’s, Longer Cancer Survival
- Risk of Therapy-Related Second Cancer “Exponentially Higher”
Angiosarcoma After Breast Radiation — Risk is Low, but Real
“After radiotherapy for breast cancer, approximately one in 1000 women will go on to develop radiotherapy-associated angiosarcoma (RAAS), and surgery alone is sufficient to treat the disease in most cases…
“As clinicians, we should be aware of the fact that there is a risk for an angiosarcoma, that it does not occur in patients who do not receive radiation, and that we should inform patients before radiotherapy about this rare, but serious, late complication,”…
For the current study, the team assembled the largest cohort to date, drawing on the nationwide Netherlands Cancer Registry to examine all patients with stages I–III primary breast cancer who were treated with or without radiotherapy between 1989 and 2015. The total population consisted of 295,577 patients who had a median age at diagnosis of 58 years and a median follow-up after breast cancer diagnosis of 7.7 years. The researchers report that, of the 111,754 patients who did not receive radiotherapy, none developed angiosarcoma…
In contrast, 209 (0.1%) of the 184,823 patients who received radiotherapy developed RAAS of the breast and/or chest wall, at a mean latency of 8 years and a median of 6 years…
Irrespective of treatment, RAAS was associated with an overall 5-year survival rate of 40.5%, falling to 25.2% at 10 years…
She said, “The benefits of radiotherapy exceed the risk of developing an angiosarcoma, and therefore we should not change follow-up schemes or stop treating patients with radiotherapy…”
Primary and secondary angiosarcoma of the breast
“Angiosarcoma is a rare soft tissue tumor of the breast. It occurs in both a primary form without a known precursor, and a secondary form that has been associated to a history of irradiated breast tissue. These forms differ in many ways including median age, precipitating factors, and presentation. Both forms have a malignant behavior and a poor prognosis. The endeavor of this paper is to review what is known about the presentation, diagnostic and therapeutic modalities to date…
Summary
Angiosarcoma of the breast in all presentations is rare. The primary and secondary forms are clinically distinct entities (Table 1). The median age of primary AS in most series is near 40, 30 years younger than that of secondary AS. The lesions of primary AS usually arise in the parenchyma of non-irradiated breast as opposed to those of secondary AS which arise in the dermal and subcutaneous layers of the skin of radiated fields, 7-10 years post radiation and may not necessarily involve the parenchyma. As the use of breast conservation therapy has increased over the last 30 years, it is assumed that the incidence of secondary AS will likely increase and that a judicious approach to delivery of adjuvant radiotherapy in the treatment of breast cancer should be considered.”

