
Recently Diagnosed or Relapsed? Stop Looking For a Miracle Cure, and Use Evidence-Based Therapies To Enhance Your Treatment and Prolong Your Remission
Multiple Myeloma an incurable disease, but I have spent the last 25 years in remission using a blend of conventional oncology and evidence-based nutrition, supplementation, and lifestyle therapies from peer-reviewed studies that your oncologist probably hasn't told you about.
Click the orange button to the right to learn more about what you can start doing today.
- You are here:
- Home »
- Blog »
- Multiple Myeloma »
- Pre-MM Becomes Full-Blown Multiple Myeloma? Bone Disease-
Pre-MM Becomes Full-Blown Multiple Myeloma? Bone Disease-
“Bone disease is an important issue in multiple myeloma and there is emerging evidence that patients with smoldering multiple myeloma and MGUS also have increased risk of skeletal-related events.”
Hi David- Last year I purchased one of your cancer coaching guides. I can’t remember if it included a phone consult with you or not? I would be interested in having a phone consult with you.
In July 2017 I was diagnosed with a single, extramedulary soft tissue plasmacytoma. I underwent 6 weeks of radiation to the site (lower left shin). There was still a residual lump at the site so in May 2018 I underwent a surgery that removed amyloid tissue, scar tissue and some remaining cancer cells.
I was told all the margins cleared and so I have just been watched for the last 2 years. Blood work has been normal -testing every 3,4, to now 6 months. My last PET was in May of 2019, with no changes from a post operation baseline PET/CT.
I am having an MRI next week to see if any changes have occurred. I requested an MRI, as opposed to a head to toe PET/CT scan because I want to reduce my exposure to radiation.
Last month I had my first bone density scan (age 53, female) and I was diagnosed with osteopenia. Osteoporosis doesn’t run in my family, nor does cancer or Multiple Myeloma.
I am concerned that this could be related to being pre MM. I have a feeling my oncologist, Dr. James Berenson (North Hollywood,CA) will want me to go on bone drugs and am just wondering if there are any more natural solutions or if because of my risk factor for developing MM if it would be advisable to go on those drugs?
I understand you can only be on them for 6 years and then what? If I am only 53 now should I try other approaches so I can use those at a later date?
I have had some autoimmune thyroid issues and so I have steered clear of gluten and have tried limiting the amount of dairy I consume so that could have contributed to my situation as well. I did notice that after completing radiation that’s when my nails became paper thin and they have never regained the strength they once had.
So that’s the background. Let me know what the structure would be for a phone consult if you think you can provide some helpful information to the current situation I am in. Thanks so much!! Linda
Hi Linda,

- Dr. James Berenson is an extremely knowledgeable MM specialist. He specializes in low-dose management of MM.
- Dr. Berenson may encourage you to undergo bisphosphonate therapy (bone drugs) but we can discuss reducing the dose, reducing the infusion rate, etc.
- The choice is yours re your bone health- there are a host of evidence-based but non-toxic bone therapies- you can undergo bisphosphonates now and/or later- your choice.
- MM Survivor
- MM Cancer Coach
- Director PeopleBeatingCancer
Recommended Reading:
- Multiple Myeloma Side Effects- Radiation-Induced Lumbosacral Plexopathy
- Multiple Myeloma Bone Therapy- Cissus Quadrangularis
- Lytic Lesions Increase Risk of Death in Multiple Myeloma
- Multiple Myeloma Symptoms, Side Effects- Vitamin D3
Bone disease in multiple myeloma and precursor disease: novel diagnostic approaches and implications on clinical management
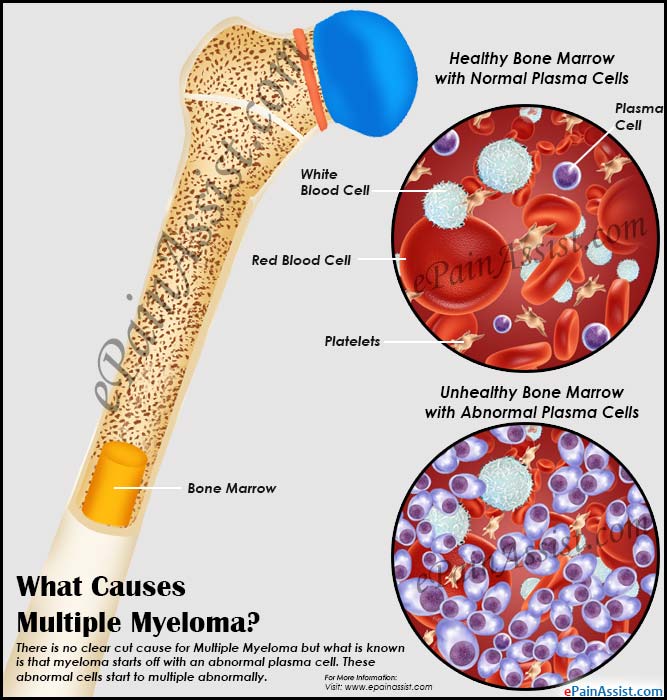
“The manifestations of bone involvement in patients with multiple myeloma (MM) can have devastating clinical effects and increase mortality. Recent studies demonstrate that patients with the precursor conditions smoldering MM (SMM) and monoclonal gammopathy of undetermined significance (MGUS) show evidence of bone disease and increased risk of fractures. The understanding of the pathogenesis of bone disease in MM has expanded in recent years…
Multiple myeloma is consistently preceded by a premalignant state,
MGUS is defined by a monoclonal protein spike less than 3 g/dl and less than 10% plasmacytosis in the bone marrow with no end organ damage (Table 1) [21]. While patients with MGUS are asymptomatic, they may have increased morbidity and mortality [22–24]. Smoldering multiple myeloma is defined by ≥3 g/dl monoclonal proteins in the blood and/or ≥10% plasmacytosis in the bone marrow, in the absence of end organ damage (Table 1)…
We recently performed a population-based study on fracture risk in patients with MGUS [27]. We identified 5326 MGUS patients diagnosed from 1958 to 2006, and compared them with 20,161 matched controls. MGUS patients had a 1.6-fold increased risk of any fracture at 10 years, with a significantly higher risk of suffering axial (skull, vertebral/pelvis and sternum/costae) compared with distal (arm and leg) fractures…
Bone disease is an important issue in multiple myeloma and there is emerging evidence that patients with smoldering multiple myeloma and MGUS also have increased risk of skeletal-related events. New imaging modalities have improved the detection of lytic lesions and may have an effect on prognosis and treatment strategies. In addition, novel agents active against multiple myeloma – such as bortezomib which seems to have anabolic effects and agents specifically inhibiting osteoclastogenesis – will probably decrease the morbidity and hopefully prolong survival of multiple myeloma patients in the future…”


