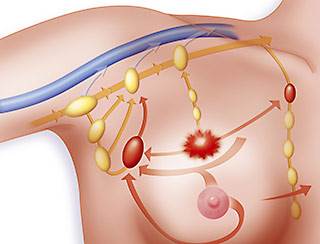
More than one in five of breast cancer patients will develop breast cancer-related lymphedema (BCRL). BCRL is a swelling that can occur in the arm, breast, or chest wall as a result of breast cancer surgery and/or radiation therapy.

Lymphedema is a common and frequently debilitating side effect of treatment for breast cancer. Studies have been limited and have not produced convincing evidence that various interventions are helpful. A new review article about those studies, “Conservative and Dietary Interventions for Cancer-Related Lymphedema: A Systematic Review and Meta-Analysis” is published in the March 15, 2011, issue of the journal Cancer.
It concludes that the “evidence suggests that compression garments and compression bandaging are effective in reducing limb lymphedema.” Regarding breast cancer, it concludes that “the addition of manual lymph drainage massage” provided a “statistically significant beneficial effect.” It also concludes that both exercise and weight loss are strategies that “improve lymphedema symptoms and reduce upper extremity lymphedema volume.”
Lymphedema was a problem for me after my lumpectomy and radiation. I believe Manual Lymph Drainage (MLD) prevented my early stage case from progressing. I have had two recurrences which required more MLD sessions to reduce the swelling and tenderness. These have been followed by long periods of controlled lymphedema.
I know many women who firmly believe that manual lymph drainage has been helpful in decreasing the pain and swelling caused by their lymphedema. For most, it is an ongoing process of attempting to control the problem.
To Learn More about Lymphadema- please read the posts linked below-
I would love to hear from women who are dealing with lymphedema. Was manual lymph drainage helpful? Too expensive? Covered by insurance? How does lymphedema affect your life?
Mary Miller- Breast Cancer- Profile in Courage
What are some methods for manual lymph drainage?
- Basic Technique: Start by applying gentle pressure with your fingertips in a circular motion. Begin at the base of the neck and move downwards towards the collarbone. Repeat this motion on the other side of the neck. Then, continue moving downwards towards the armpits, following the natural path of the lymphatic vessels.
- Pumping Movements: Use rhythmic pumping movements with your hands to stimulate lymphatic flow. This involves applying gentle pressure and releasing in a repetitive motion. Start at the base of the neck and work downwards towards the collarbone, then move to the armpits, and finally down towards the groin area.
- Stretching: Incorporate gentle stretching movements into the massage to help release tension and improve lymphatic flow. This can include stretching the arms, neck, and shoulders while applying gentle pressure.
- Rotary Technique: Use a circular or rotary motion with your fingertips to stimulate lymphatic flow in specific areas. This can be particularly useful for targeting areas of congestion or swelling.
- Deep Breathing: Encourage deep breathing during the massage to enhance the movement of lymphatic fluid. Instruct the person receiving the massage to take slow, deep breaths while you perform the techniques.
- Sequence: Follow a specific sequence when performing manual lymph drainage to ensure thorough coverage of the lymphatic system. Typically, you’ll start at the neck, move down to the arms, then the trunk, and finally the legs.
- Light Pressure: Apply gentle, consistent pressure throughout the massage. Avoid using too much force, as this can hinder lymphatic flow and cause discomfort.
- Consistency: Perform manual lymph drainage regularly to maintain the benefits. Depending on the individual’s needs, this may be done daily or a few times per week.
- Professional Training: Consider receiving training from a certified lymphedema therapist or healthcare professional to learn proper manual lymph drainage techniques. They can provide guidance on specific techniques tailored to individual needs and conditions.
“The findings support the use of compression garments and compression bandaging for reducing lymphedema volume in upper and lower extremity cancer-related lymphedema. Specific to breast cancer, a statistically significant, clinically small beneficial effect was found from the addition of manual lymph drainage massage to compression therapy for upper extremity lymphedema volume…”
“More than one in five of breast cancer patients will develop breast cancer-related lymphedema (BCRL). BCRL is a swelling that can occur in the arm, breast, or chest wall as a result of breast cancer surgery and/or radiation therapy. BCRL can negatively impact comfort, function, and quality of life.
Manual lymphatic drainage (MLD) is a hands-on therapy that is commonly used for BCRL and often as part of complex decongestive therapy (CDT). CDT consists of MLD, compression bandaging, lymph-reducing exercises (LREs), and skin care.
The Review Questions
Is MLD safe and effective in treating BCRL?
Study Characteristics
We found six trials published through May 2013, totaling 208 participants.
Key Results
When women were treated with a course of intensive compression bandaging, their swelling went down about 30% to 37%. When MLD was added to the intensive course of compression bandaging, their swelling went down another 7.11%. Thus, MLD may offer a benefit when added to compression bandaging.
Examining this finding more closely showed that this significant reduction benefit was observed in people with mild-to-moderate lymphedema when compared to participants with moderate-to-severe lymphedema. Thus, our findings suggest that individuals with mild-to-moderate BCRL are the ones who may benefit from adding MLD to an intensive course of treatment with compression bandaging. This finding, however, needs to be confirmed by further research.
When women were given a standard elastic compression sleeve plus MLD and compared to women who received a standard compression sleeve plus a non-MLD treatment, results were mixed (sometimes favoring MLD and sometimes favoring neither treatment.)
One-year follow-up suggests that once the swelling had been reduced, participants were likely to keep their swelling down if they continued to use a custom-made sleeve.
MLD is safe and well tolerated…”
| Compression garment (CG) |
| Compression bandaging (CB) |
| Compression systems: specialized garments |
| Electrophysical modalities (eg, low-level laser therapy, electrical stimulation) |
| Elevation |
| Exercise |
| Intermittent pneumatic compression (IPC) pumps |
| Manual lymph drainage (MLD) massage |
| Self-massage (SM) techniques |
| Decongestive lymphatic therapy (DLT) |
| Dietary/weight loss intervention |
RESULTS
We identified 157 papers, of which 48 were considered potentially relevant. Independent review of these 48 papers led to the inclusion of 25 studies involving 1018 participants.13-37 Studies were carried out in 14 different countries/regions worldwide. Study methodology varied significantly, particularly in regard to the chosen intervention and comparison treatment (Table 2). Of the included studies, 2 authors provided additional information on study methods16, 18 and 1 author provided additional data for use in the meta-analysis.18 Kappa statistics for agreement between the reviewers on the inclusion of trials and quality score was 0.7 and 0.9, respectively…”