
Diagnosed with Cancer? Your two greatest challenges are understanding cancer and understanding possible side effects from chemo and radiation. Knowledge is Power!
Learn about conventional, complementary, and integrative therapies.
Dealing with treatment side effects? Learn about evidence-based therapies to alleviate your symptoms.
Click the orange button to the right to learn more.
- You are here:
- Home »
- Blog »
- side effects ID and prevention »
- Chemotherapy-induced Heart Damage Breast Cancer
Chemotherapy-induced Heart Damage Breast Cancer
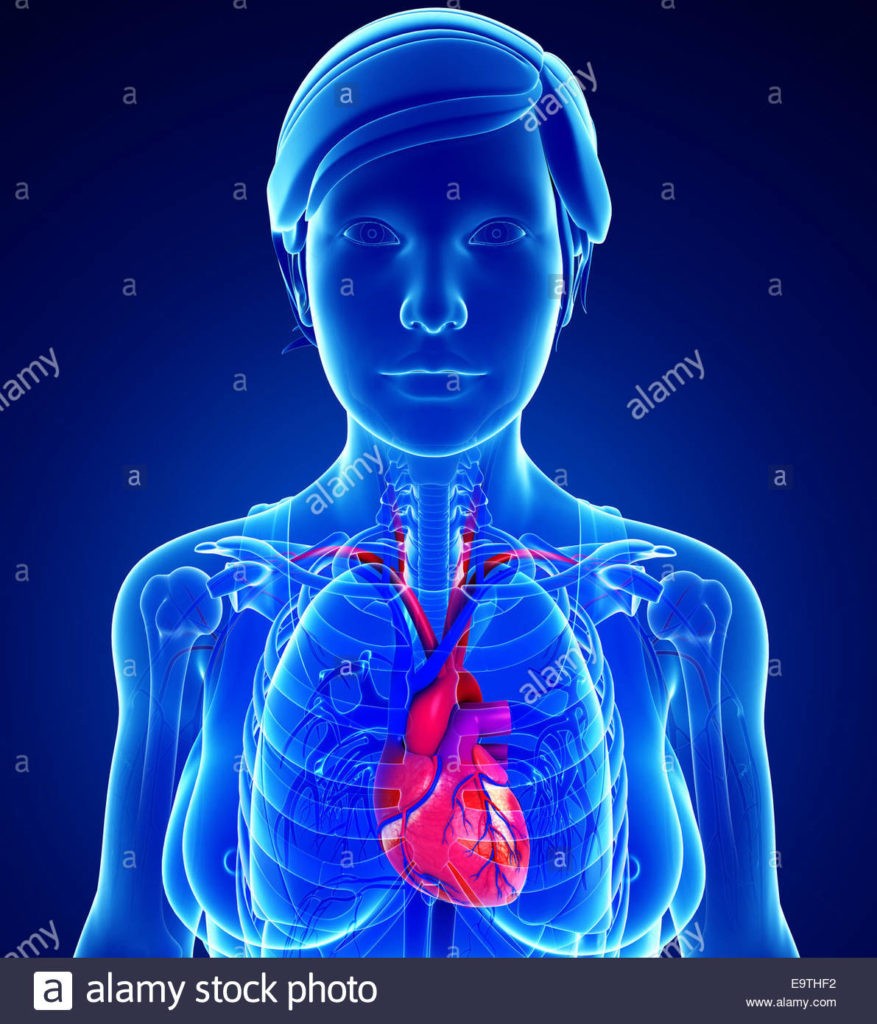
Chemotherapy-induced Heart Damage in Breast Cancer patients is a serious short, long-term and late stage side effect. Both chemotherapy and radiation have been shown to cause heart damager. While the study linked and excerpted below does a reasonable job of explaining chemotherapy-induced heart damage in breast cancer, there are several key failing of the study.
I understand chemotherapy-induced cardiomyopathy intimately because I underwent four different cardiotoxic chemo regimens during my conventional therapies for multiple myeloma in ’95 and ’96 including:
- Vincristine
- Doxorubicin
- Cytoxan/cyclophosphomide
- Busulphan
- Melphalan
and then was diagnosed with CIC in December of 2010 fully 15 years after this cardiotoxic chemo.
What causes chemotherapy-induced heart damage in Breast Cancer?
- Chemotherapy Drugs: Certain chemotherapy drugs used to treat breast cancer, such as anthracyclines (e.g., doxorubicin, epirubicin) and trastuzumab (Herceptin), can be cardiotoxic. They can cause damage to the heart muscle cells, leading to conditions like cardiomyopathy (weakening of the heart muscle) or heart failure.
- Free Radical Formation: Chemotherapy drugs can generate free radicals, which are highly reactive molecules that can damage cells, including those in the heart.
- Inflammation: Chemotherapy can cause inflammation in the body, including the heart tissue, which can contribute to heart damage.
- Impaired DNA Repair: Some chemotherapy drugs interfere with the repair mechanisms of DNA in heart muscle cells, leading to cell damage and dysfunction.
- Individual Susceptibility: Not all patients experience chemotherapy-induced heart damage, suggesting that individual factors, such as genetics, pre-existing heart conditions, age, and lifestyle, may play a role in determining susceptibility.
- Cumulative Dose: The risk of heart damage may increase with higher cumulative doses of cardiotoxic chemotherapy drugs over time.
- Combination Therapies: Combining different chemotherapy drugs or adding other treatments like radiation therapy may further increase the risk of heart damage.
- Pre-existing Cardiovascular Conditions: Patients with pre-existing cardiovascular conditions, such as hypertension or coronary artery disease, may be at higher risk of chemotherapy-induced heart damage.
What are the failings of the study linked below?
The study linked below primarily focus’ on chemotherapy-induced heart damage in breast cancer patients as a short-term side effect. The study goes so far as to talk about resolving the heart damage completely if the problem is identified early in the patient’s survivorship.
Secondly and possibly more importantly, are evidence-based non-conventional therapies shown to support and possibly heal chemotherapy-induced heart damage in breast cancer patients. I myself supplement with
If cancer patients ask their oncologists about evidence-based non-conventional therapies taken before, during and after chemotherapy in an effort to reduce or prevent chemotherapy-induced cardiomyopathy, it is probable that the board certified oncologist will simply dismiss nutritional supplementation.
My only goal in writing this post is to educate current and future breast cancer patients considering cardiotoxic chemotherapy.
I take each of the supplements listed above. I exercise (moderately) each day. I eat as cleanly (lots of fruits and veggies) as I can. I do not take any conventional heart medications.
If you would like to learn more about cancer- both conventional and non-conventional therapies, email me at David.PeopleBeatingCancer@gmail.com
Good luck,
David Emerson
- Cancer Survivor
- Cancer Coach
- Director PeopleBeatingCancer
Assessment of Chemotherapy-Induced Cardiac Dysfunction in Breast Cancer Patients: A Prospective Study
“Advances in cancer treatment have markedly improved survival rates but have also heightened morbidity due to treatment-related side effects. Despite this, the literature remains scarce on predicting the incidence of acute cardiac toxicity resulting from chemotherapy…
Our study aimed to assess the cardiovascular complications of cancer therapy in breast cancer patients, with particular emphasis on therapy-related cardiac dysfunction…
Early detection, modification of chemotherapy regimens, and prompt initiation of CTRCD therapy can lead to substantial recovery of cardiac dysfunction…
However, cancer therapy-related adverse effects are a matter of concern among physicians involved in the care of cancer patients. Some cancer treatments have adverse side effects, of which cardiovascular complications are the most important and worrisome. Thus, chemotherapy is now proven to be a “double-edged sword.” Cancer patients who were successfully treated with chemotherapy are suffering from cardiovascular diseases-
For instance, anthracyclines, trastuzumab, and some tyrosine kinase inhibitors have a detrimental effect on myocardial function…
The oxidative stress hypothesis elucidates anthracycline-induced toxicity, emphasizing reactive oxygen species generation and lipid peroxidation damaging cardiomyocyte membranes [6-9]. In a study by Cardinal et al. involving 2625 patients (mean follow-up: 5.2 years), cardiotoxicity incidence after anthracycline treatment was 9%, with 98% occurring within the first asymptomatic year [7,10].
Risk factors include:
- cumulative dose,
- infusion regimen,
- preexisting cardiac conditions,
- hypertension,
- concomitant chemotherapy,
- and age over 65 years [11].
Cyclophosphamide, cisplatin, ifosfamide, and taxanes (paclitaxel and docetaxel) are among the conventional chemotherapies capable of inducing myocardial dysfunction and heart failure…
Large-scale clinical trials indicate cardiac dysfunction rates ranging from 7% to 34%, with heart failure rates between 0% and 4%. When trastuzumab is administered alongside anthracyclines, heart failure rates are 6.2% after one year and <20.1% after five years. Among patients receiving trastuzumab, cardiotoxicity is the primary cause of treatment interruption in 13.5% of cases [9,12]…
Radiation exposure is associated with an increased risk of ischemic heart disease in patients with breast cancer. Radiation to the left breast is of particular concern given its anatomical proximity to the heart, and studies have shown increased cardiovascular events in patients receiving left-sided radiotherapy compared to the right side. Marked interstitial myocardial fibrosis is common in radiation-induced cardiotoxicity [9]…
Preventive strategies for cardiotoxicity involve
- early diagnosis,
- limiting cumulative doses,
- prolonged administration time (infusion over 24 – 96 hours),
- strengthening the monitoring of cardiotoxicity,
- and the use of liposomal anthracycline.
Non-pharmacological measures should be promoted, including
- a healthy diet,
- smoking cessation,
- regular exercise,
- and weight control.
Prior to starting potential cardiotoxic chemotherapy, risk stratification and echocardiography should be done to determine the baseline left ventricular function. Early detection of decreased ventricular function allows modification of the chemotherapy regimen, either by increasing the interval between doses or reducing the total cumulative dose of potentially toxic agents…
Conclusions In conclusion, despite limitations, our study highlights the significant incidence of acute cardiac toxicity among breast cancer patients. Essential hypertension, left breast involvement, and high doses of radiotherapy emerged as independent predictors of chemotherapy-related cardiac dysfunction (CTRCD).
Close monitoring for CTRCD is crucial, especially for left breast-involved, hypertensive patients and those undergoing high-dose radiotherapy. Early diagnosis and prompt initiation of heart failure therapy led to complete recovery in 77% of patients, with 23% experiencing partial recovery.
Notably, LV dysfunction was independent of cumulative chemotherapy doses. Patients with
- ER-positive,
- PR-positive, and
- HER2-positive status,
- as well as those in cancer stages III and IV,
are at higher risk of developing LV dysfunction. Further studies are warranted to refine risk stratification and optimize treatment strategies for CTRCD in breast cancer patients.”


