I encourage breast cancer patients to undergo hyperbaric oxygen therapy- especially if they’ve undergone radiation therapy. I say this because both chemo and radiation can kill cancer cells but also can kill normal cells at the same time.
I say this for two reasons. First, countless studies confirm that HBOT can heal radiation therapy. Secondly, I am a cancer survivor myself. I underwent several courses of radiation therapy. I sustained several different types of radiation fibrosis (scarring).
Unfortunately, I didn’t know about HBOT as a healing therapy and did not undergo HBOT treatments for several years after I finished my radiation treatments. I healed and felt better after HBOT but I could have healed the fibrosis much more if I had begun soon after my radiation.
How does hyperbaric oxygen therapy heal radiation fibrosis?
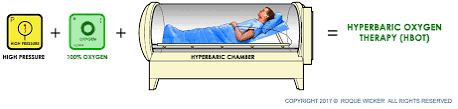
Hyperbaric oxygen therapy (HBOT) is a medical treatment that involves breathing pure oxygen in a pressurized room or chamber. It is commonly used to treat conditions such as decompression sickness, carbon monoxide poisoning, and non-healing wounds. In the context of radiation fibrosis, HBOT is sometimes used as an adjunctive therapy to help alleviate symptoms and promote healing. However, it’s important to note that while HBOT may provide relief, it is not considered a cure for radiation fibrosis.
Radiation fibrosis is a condition that can occur as a result of radiation therapy for cancer treatment. It involves the development of scar tissue (fibrosis) in the irradiated area, which can lead to a range of symptoms including pain, stiffness, and impaired function. The exact mechanisms by which HBOT may help in the treatment of radiation fibrosis are not fully understood, but there are several potential ways in which it may provide benefit:
- Increased oxygen delivery: Radiation therapy can damage blood vessels and reduce oxygen levels in the affected tissues. HBOT increases the amount of oxygen dissolved in the blood, which can help to deliver oxygen to oxygen-deprived tissues. This increased oxygen delivery may promote healing and reduce inflammation in the irradiated area.
- Stimulation of angiogenesis: HBOT has been shown to stimulate the formation of new blood vessels (angiogenesis). By promoting the growth of new blood vessels, HBOT may improve blood flow to the irradiated tissues, which can help to alleviate symptoms and promote healing.
- Reduction of inflammation: Radiation therapy can trigger inflammation in the irradiated tissues, which can contribute to the development of fibrosis. HBOT has anti-inflammatory effects, which may help to reduce inflammation in the affected tissues and alleviate symptoms associated with radiation fibrosis.
- Enhancement of tissue repair: HBOT has been shown to enhance the body’s natural healing processes, including tissue repair and wound healing. By promoting tissue repair, HBOT may help to improve the function and appearance of the irradiated area.
It’s important to note that while HBOT may provide symptomatic relief and promote healing in some cases of radiation fibrosis, it may not be effective for everyone, and the benefits can vary depending on the individual patient and the severity of the condition. Additionally, HBOT may be associated with certain risks and side effects, so it’s essential to discuss the potential risks and benefits with a healthcare provider before undergoing treatment.

According to the top article linked below, HBOT has been approved by the FDA for radiation injury. Keep in mind however, that your health insurance may not cover HBOT. You may need to have your oncologist specifically prescribe HBOT for you.
Also keep in mind that radiation fibrosis is often a damaging side effect that does not rear its ugly head for years after your radiation treatment ends. This is what happened to me. Again, if you are a breast cancer patient who has undergone radiation, undergo hyperbaric oxygen treatments as soon as you can once your radiation concludes.

man hand holding his nutritional supplemets, healthy lifestyle background.
If you would like to learn more about evidence-based, non-conventional therapies for breast cancer, send me an email with your stage and treatment history- David.PeopleBeatingCancer@gmail.com
Hang in there,
David Emerson
- Cancer Survivor
- Cancer Coach
- Director PeopleBeatingCancer
“Hyperbaric oxygen chambers are classified by the US Food and Drug Administration (FDA) as “Class II medical devices.” Class II medical devices are those devices that have a moderate to high risk to the patient and/or user and the majority of medical devices fall under this category…
Despite the fact that the FDA labeling does not limit appropriate clinical use of a device, payers often use the FDA clearance list as a reason to deny payment for off-label use…
As of July 2021, the FDA has cleared hyperbaric chambers for the following disorders:
Hyperbaric Oxygen Therapy (HBOT) has been gaining attention as a potential treatment for late toxicities such as fibrosis and pain associated with radiation therapy in breast cancer patients. However, the effectiveness of this treatment remains a topic of debate, with a recent Dutch randomized study shedding more light on the issue.
A Closer Look at the Dutch Study
The Dutch study, which was partially funded by the Da Vinci Clinic, found that HBOT was ineffective for reducing pain but effective for reducing fibrosis among women with late local toxic effects after breast cancer irradiation. However, the acceptance rate of the treatment was low, with only 25% of the women offered HBOT accepting and completing the treatment. The low acceptability rate was linked to the high treatment intensity of HBOT, which played a significant role in patient decision-making.
Despite the disappointing results in terms of pain reduction, the study’s complier average causal effect (CACE) analysis showed that HBOT was associated with decreased pain and fibrosis. Nonetheless, due to the smaller-than-anticipated number of patients willing to undergo HBOT, the study was underpowered. Both the authors and editorialists called for adequately powered randomized, sham-controlled, double-blind trials to better determine the true benefit of HBOT.
HBOT: A Controversial Treatment
While the US Food and Drug Administration has cleared HBOT for marketing for several conditions, including radiation injury, concerns about unproven claims of effectiveness and potential misuse at unaccredited facilities persist. This skepticism is further fueled by the limitations of studies such as the Dutch randomized trial, including the possibility of reporting bias.
HBOT’s Potential Benefits
Despite the skepticism, HBOT holds promise in reducing radiation-induced tissue damage and improving the quality of life for breast cancer patients who have undergone radiation therapy. By delivering almost 100% oxygen in a pressurized chamber, HBOT promotes a healing environment, fostering tissue repair, reducing inflammation, and enhancing blood flow to affected areas. Such benefits make HBOT a potential treatment for post-radiation injuries.
Furthermore, HBOT’s recognition as a therapeutic tool for addressing the long-term effects of radiation therapy is underscored by its coverage by Irish Life Health at OxyGeneration for post-radiation damage. This highlights the perceived therapeutic value of HBOT in the medical community.
Conclusion
While the Dutch randomized study has shed some light on the effectiveness of HBOT in treating late toxic effects of breast cancer radiation therapy, more research is needed. Adequately powered randomized, sham-controlled, double-blind trials could provide a more definitive answer on the true benefits of HBOT. In the meantime, the potential benefits of HBOT, coupled with early intervention, could play a significant role in managing post-radiation injuries effectively, offering relief and healing to breast cancer patients.