Diagnosed with Cancer? Your two greatest challenges are understanding cancer and understanding possible side effects from chemo and radiation. Knowledge is Power!
Learn about conventional, complementary, and integrative therapies.
Dealing with treatment side effects? Learn about evidence-based therapies to alleviate your symptoms.
Click the orange button to the right to learn more.
- You are here:
- Home »
- Blog »
- side effects ID and prevention »
- Cardiomyopathy- Non-toxic approach
Cardiomyopathy- Non-toxic approach
The goal of cardiomyopathy treatment is to help your heart be as efficient as possible and to prevent further damage and loss of function.
I am a cardiomyopathy (CM) survivor not a cardiologist. Well, actually, I am a long-term cancer survivor who developed chemotherapy-induced cardiomyopathy from the administration of cardiotoxic chemo regimes when I was first diagnosed with cancer.
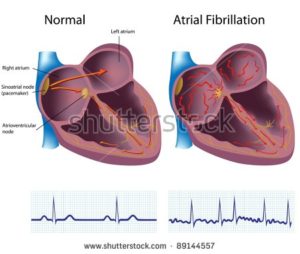
My heart flipped into chronic atrial fibrillation (Afib) in December of 2010. I underwent cardiotoxic chemotherapies in late 1995. In other words, my heart was fine for 15 years post chemo. This is the definition of a late stage side effect of cancer treatment.
The point of this post is simply to explain cardiomyopathy and to talk about evidence-based heart therapies. When I developed CM, I went to a cardiologist at the Cleveland Clinic, one of the best places to go for heart health, and my doctor prescribed metoprolol. No discussion of
- Nutrition
- Nutritional Supplementation
- Lifestyle therapies such as exercise
My cardiologist went straight to heart drugs. After having a reaction to metoprolol, I researched and built a daily regiment of evidence-based non-toxic heart therapies such as exercise, sauna, sleep, nutrition, supplementation, etc. And I’ve improved or stabilized all of my heart metrics such as
- ejection fraction
- blood pressure
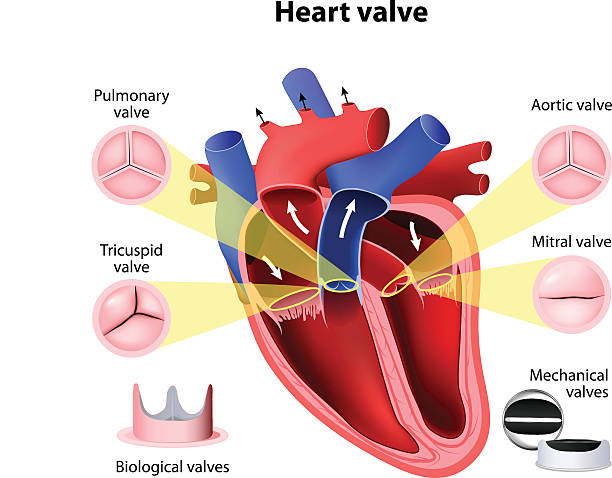
- valve health
etc. I am NOT saying that everyone with cardiomyopathy can manage their heart health without conventional heart medications. I am just offering another possible therapy plan to consider. Or consider combining conventional heart meds with non-conventional heart therapies.
What is Cardiomyopathy?
Cardiomyopathy is a term that refers to diseases of the heart muscle. In this condition, the heart muscle becomes enlarged, thickened, or rigid, which can lead to the heart’s inability to pump blood effectively. As a result, the heart may weaken over time, and other complications can arise.
There are several types of cardiomyopathy, including:
- Dilated Cardiomyopathy (DCM): The heart chambers become dilated (enlarged) and weakened, affecting the heart’s pumping ability.
- Hypertrophic Cardiomyopathy (HCM): The heart muscle becomes abnormally thick, making it harder for the heart to pump blood.
- Restrictive Cardiomyopathy (RCM): The heart muscle becomes stiff and less elastic, restricting the heart’s ability to fill with blood properly.
- Arrhythmogenic Right Ventricular Dysplasia/Cardiomyopathy (ARVD/C): This rare type involves the replacement of normal heart muscle tissue with fatty or fibrous tissue, leading to arrhythmias and other issues.
The causes of cardiomyopathy can vary and may include
- genetic factors,
- infections,
- certain medications,
- excessive alcohol consumption,
- and other underlying health conditions.
Symptoms can also vary depending on the type of cardiomyopathy but may include fatigue, shortness of breath, swelling of the legs, ankles, or abdomen, and irregular heartbeats.
Treatment for cardiomyopathy depends on the type and severity of the condition. It may involve medications, lifestyle changes, implanted devices (such as pacemakers or defibrillators), or, in severe cases, heart transplantation. It’s essential for individuals with cardiomyopathy to work closely with their healthcare team to manage the condition and improve their quality of life.
My point is that heart health is a huge issue that requires a broad understanding beyond what conventional cardiology will tell you. Yes, cardiologists are central to managing your heart but also learn about and consider all the evidence-based approaches.
Have you been diagnosed with cardiomyopathy? Do you have any questions? Let me know- David.PeopleBeatingCancer@gmail.com
David Emerson
- Cancer Survivor
- Cancer Coach
- Director PeopleBeatingCancer
Recommended Reading:
- Evidence to Manage My Heart Disease is “Weak”
- Coffee, Afib, Cardiomyopathy and Cancer Survivor
- David Emerson: Multiple Myeloma Survivor Since 3/94
New York Heart Association Functional Classification
“The New York Heart Association (NYHA) Functional Classification[1] provides a simple way of classifying the extent of heart failure. It places patients in one of four categories based on how much they are limited during physical activity; the limitations/symptoms are in regard to normal breathing and varying degrees in shortness of breathand/or angina…”
Cardiomyopathy
“Cardiomyopathy is a progressive disease of the myocardium, or heart muscle. In most cases, the heart muscle weakens and is unable to pump blood to the rest of the body as well as it should. There are many different types of cardiomyopathy caused by a range of factors, from coronary heart disease to certain drugs. These can all lead to an irregular heartbeat, heart failure, a heart valve problem, or other complications.
- Dilated cardiomyopathy
- The most common form, dilated cardiomyopathy (DCM), occurs when your heart muscle is too weak to pump blood efficiently. The muscles stretch and become thinner. This allows the chambers of your heart to expand.
- Hypertrophic cardiomyopathy
- Arrhythmogenic right ventricular dysplasia (ARVD)
- Restrictive cardiomyopathy
- Other types
What are the symptoms of cardiomyopathy?
The symptoms of all types of cardiomyopathy tend to be similar. In all cases, the heart can’t adequately pump blood to the tissues and organs of the body. It can result in symptoms such as:
- general weakness and fatigue
- shortness of breath, particularly during exertion or exercise
- lightheadedness and dizziness
- chest pain
- heart palpitations
- fainting attacks
- high blood pressure
- edema, or swelling, of your feet, ankles, and legs
What is the treatment for cardiomyopathy?
Treatment varies depending on how damaged your heart is due to CM and the resulting symptoms.
Some people may not require treatment until symptoms appear. Others who are beginning to struggle with breathlessness or chest pain may need to make some lifestyle adjustments or take medications.
You can’t reverse or cure CM, but you can control it with some of the following options:
- heart-healthy lifestyle changes
- medications, including those used to treat high blood pressure, prevent water retention, keep the heart beating with a normal rhythm, prevent blood clots, and reduce inflammation
- surgically implanted devices, like pacemakers and defibrillators
- surgery
- heart transplant, which is considered a last resort
The goal of treatment is to help your heart be as efficient as possible and to prevent further damage and loss of function.
What is the long-term outlook?
CM can be life-threatening and can shorten your life expectancy if severe damage occurs early on. The disease is also progressive, which means it tends to get worse over time. Treatments can prolong your life. They can do this by slowing the decline of your heart’s condition or by providing technologies to help your heart do its job.
Those with CM should make several lifestyle adjustments to improve heart health. These may include:
- maintaining a healthy weight
- eating a modified diet
- limiting caffeine intake
- getting enough sleep
- managing stress
- quitting smoking
- limiting alcohol intake
- getting support from their family, friends, and doctor